Lung ultrasound: Pulmonary oedema
Pulmonary oedema is a common cause of acute respiratory distress in critical care environments.
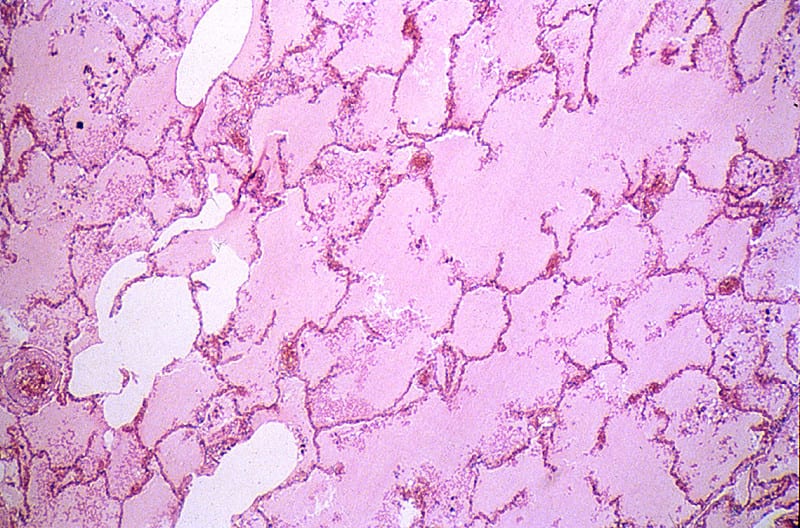
Cardiogenic pulmonary oedema occurs when raised left ventricular filling pressure leads to raised left atrial pressure, raised pulmonary venous pressures and then elevated pulmonary capillary pressure. Protein poor fluid traverses the capillary membranes into the pulmonary interstitium and alveolar air spaces.
The histological appearance of severe pulmonary oedema.
Causes of raised left ventricular filling pressure include:
- Pump failure – left ventricular systolic or diastolic dysfunction.
- Valve failure – severe aortic or mitral stenosis or regurgitation.
- Left sided flow obstruction – severe systemic hypertension, hypertrophic obstructive cardiomyopathy (HOCM), prosthetic valve dysfunction, or atrial myxoma.
- Volume overload.
Noncardiogenic pulmonary oedema occurs most commonly when there is increased permeability of the pulmonary capillaries.
Causes of noncardiogenic pulmonary oedema include:
- Acute respiratory distress syndrome (ARDS).
- Neurogenic pulmonary oedema.
- High altitude pulmonary oedema.
- Pulmonary contusion.
- Re-expansion pulmonary oedema – post large effusion drainage.
- Transfusion-related acute lung injury.
- Post pulmonary embolism pulmonary oedema.
- Post overdose pulmonary oedema – opiate and salicylate.
- Chemical pneumonitis.
- Viral pneumonitis.
The ultrasound features of pulmonary oedema are characteristic, but non-specific. Ultrasound can be used to determine the severity and distribution of oedema but not necessarily the aetiology. Echocardiography can be invaluable in determining the various cardiac causes.
The clinician must differentiate other causes based on the history and the clinical features of the presentation. Sometimes the distribution can be useful in differentiating the cause.
Typical ultrasound features of pulmonary oedema
B-lines
Confluent B-lines
The ultrasound appearance of pulmonary oedema
B-lines
- Vertical echogenic short path reverberation artefacts originating at the pleural line and extending to the deepest part of the ultrasound image.
- They interrupt any horizontal A-lines.
- Occasional B-lines are considered normal.
- More than 3 B-lines in any single view is considered pathological.
- Where there are numerous B-lines in close proximity they become confluent.
- B-lines move with lung movement.
- They are caused by ultrasound energy reverberating in a fluid filled focus that is surrounded by air. These foci may be interstitial or alveolar.
- Cardiogenic and noncardiogenic oedema may have very similar appearances.
- Interstitial thickening due to fibrosis or lymphangitis can also create the sonographic appearance of diffuse B-lines.
Pleural effusions
- Bilateral small to moderate pleural effusions are common particularly in cariogenic pulmonary oedema.
- Explore the posterior costophrenic angles for fluid.
Echocardiographic examination
- Assess left ventricular function, ideally systolic and diastolic.
- Assess for aortic and mitral valve dysfunction.
- Assess for other causes of left sided flow obstruction
Related Clinical Cases
ULTRASOUND LIBRARY
POCUS
An Emergency physician based in Perth, Western Australia. Professionally my passion lies in integrating advanced diagnostic and procedural ultrasound into clinical assessment and management of the undifferentiated patient. Sharing hard fought knowledge with innovative educational techniques to ensure knowledge translation and dissemination is my goal. Family, wild coastlines, native forests, and tinkering in the shed fills the rest of my contented time. | SonoCPD | Ultrasound library | Top 100 | @thesonocave |