Meow-Meow Mephedrone
Its 5am Sunday morning in the ED, you just finish making your first cup of coffee for the shift! You are handed an ECG on a 26 year old male pharmacology student who presented complaining of palpitations, blurred vision and profuse sweating having taken meow-meow.
Not having heard of the drug before, you turn to your trusted pharmacopaedia – the internet to look for recent clinical cases and determine that meow-meow is the street name for Mephedrone, a new amphetamine-like substance available on the streets.
On examination the patient is restless, agitated and tremulous. He is complaining of chest tightness and worsening palpitations. Recorded vital signs include: sinus tachycardia (143 bpm), hypertension (BP 185/90), temperature 37.9°C, BSL 5.4mmol/L and SaO2 99%
You gain IV access, commence IV fluids and administer 25 mg of IV Diazepam in 5mg increments over the next 40 minutes.
An hour later you review the patient who is now resting comfortable on the trolley. Vital signs have returned to normal and laboratory investigations including Troponin levels are all within normal limits.
The patient is seen in the observation ward later that morning and his discharged home following drug and alcohol counseling.
What is Mephedrone?
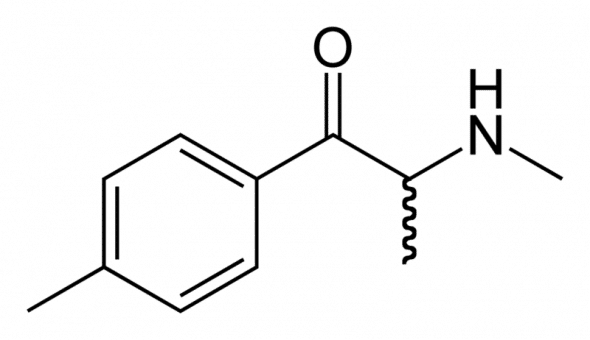
- 4-methylmethacathinone (4-MMC) or 4-methylephedrone.
- Synthetic derivation of cathinone – a pharmacologically active alkaloid from the leaves of the Khat plant.
- Synthetic stimulant with euphoric and empathogenic effects similar to MDMA, cocaine and other methamphetamines.
- Popular club drug especially in the UK and USA, with only a handful of reported cases in Australia.
- Little is known about mephedrone intoxication, although deaths have been reported secondary to sympathomimetic complications or when taken with multiple co-ingestants such as alcohol, ketamine or other recreational drugs.
- Mephedrone is available over the internet, however in Australia methylmethcathinone is a prohibited substance and it is illegal to import.
- In Britain, the Home Secretary has classified Mephedrone as a class-B substance
“Compared to MDMA, similar euphoria (when bombed “swallowed”), far more hornyness, a bit less empathy, no psychadelia (although lights tend to prism after several redoses, I think this is just a serotonin effect) – but what is amazing is that the next day, I felt brilliant, like I hadn’t done anything the previous night. I would also compare it to speed and coke a little in it’s stimulating effects, which were far more than MDMA on its own. The euphoria was absolutely crazy. I looked in a mirror, my eyes were saucers. I felt giddy from how amazing i felt. Stroking my arm was like having an orgasm. It was as mind-blowing as my first ‘e’.”
Presentation and street names:
- Mephedrone usually comes as a clear white powder hence the incorporation into ‘bath salts’. It is also found as crystals, capsules and pills
- The powder form is usually mixed with water and swallowed (bombed) but can be sniffed/snorted or taken intravenously.
- A standard dose is between 75 and 200 mg
Street Names:
- Meph
- Meow-meow
- Miawo-miawo
- khat
- qat
- m-cat
- Drone
- Bubbles
- Kitty cat
Mephedrone toxicokinetics and toxic mechanisms:
- Mephedrone has a very short half life ( 30-90 min) with effects lasting 2-4 hours.
- With such as short half-life, meow-meow is often associated with compulsive ‘re-dosing’
- Limited reports and studies show mephedrone is likely to stimulate the release of, then inhibit, the reuptake of manoamine neurotransmitters.
- The main reported side effect suggest mephedrone causes pronounced peripheral vasoconstriction, which has been speculated to result from the formation of the potent vasoconstrictor 4-methylephedrine. This metabolite is known to have significantly more cardiovascular toxicity than ephedrine.
Mephedrone Toxidrome
Until further literature is published on mephedrone base your clinical assessment, the same as you would for amphetamine intoxicated patients, and look for the same clinical features and complications:
Central Nervous System:
- Euphoria
- Anxiety, dysphoria, agitation and aggression
- Paranoid psychosis with visual and tactile hallucinations
- Hyperthermia, rigidity and myoclonic movements
- Seizures
Cardiovascular:
- Tachycardia
- Dysrthyhmias
- Acute coronary syndrome
- Acute cardiomyopathy
- Acute pulmonary oedema
- Haemoptysis
Peripheral Sympathomimetic:
- Mydriasis, diaphoresis, and tremor
Clinical features associated with medical complications:
- Rhabdomyolysis, dehydration and renal failure
- Hyponatraemia and cerebral oedema (secondary to temporary SIADH and increased water ingestion)
- Aortic and carotid artery dissection
- Subarachnoid and intracerebral haemorrhage
- Ischaemic collitis
Assessment of Mephedrone intoxication:
Tox Screen:
- Blood sugar level
- 12-lead ECG
- Paracetamol level
- Breath alcohol level
- Temperature
Specific Test as Indicated:
- ECG, CK and Troponin to detect myocardial ischaemia and rhabdomyolysis
- Urea and Electrolytes looking for renal failure and hyponatraemia
- Chest X-ray detect aspiration or aortic dissection
- Urine drug screen is not clinically useful and should not alter management
Emergency Department Management of Mephedrone Intoxication:
Initial Resuscitation:
- Promptly assess airway, breathing and circulation
- Control seizures; always generalised when due to toxicological causes, Benzodiazepines are the first line of therapy
- Correct hypoglycaemia: treat if BSL <4mmol/L
- Correct hyperthermia: Temperature >38.5 prompts urgent management.
Decontamination:
- Mephedrone is rapidly absorbed once ingested, activated charcoal is not clinically useful
Enhanced Elimination:
- Not clinically Useful
Antidotes:
- None Available
Ongoing Management:
- Good supportive care, in an area that is capable of cardiorespiratory monitoring and resuscitation, will provide best outcomes for the patient.
- Benzodiazepines in titrated doses are the main treatment modality available to treat the symptoms of sympathomimetic intoxication such as tachycardia, hypertension, agitated delirium, seizures, and hyperthermia.
- Supportive care including adequate hydration, bladder care and pressure area care can prevent further complications.
- Hyperthermia must be closely monitored. Temperatures above 39.5 which do not respond to benzodiazepine administration and fluid resuscitation, should prompt urgent assessment for intubation and paralysis in order to prevent multi-organ failure and neurological injury.
- Refractory hypertension not responding to benzodiazepine sedation can be treated with alpha-adrenergic antagonist like phentolamine or a titrated infusion of a vasodilator such as Glyceryl Trinitrate.
- Note: Beta-adrenergic blockers are contraindicated
- Sodium levels should be monitored closely especially if patient has a seizure. Hyponatraemia (serum Na <120mmol/L) should be corrected with hypertonic saline administration.
- Increasing agitation and psychosis should be treated with escalating dose’s of benzodiazepines.
- Note: In theory, antipsychotics could be administered, but these have been shown to increase anticholinergic side effects and lower the seizure threshold.
References
- NRG-1? Buphedrone? Flephedrone? — What will follow meow-meow and where will it come from?
- Mephedrone: The Users, The Dealers, The Debate [Guardian]
- Mephedrone after the ban
- Woof-woof: the new meow-meow?
- Mephedrone (meow-meow): first confirmed case report
- Management of Patients with Psychostimulant Toxicity: Guidelines for Emergency Departments: (2006). Canberra: National Drug Strategy
- Murray L, Daly FFS, Little M, and Cadogan M. Chapter 3.8 Amphetamines; in Toxicology Handbook, Elsevier Australia, 2007. [Google Books Preview]
- Wood, A. et.al. (2010). Recreational Use of Mephedrone (4-Methylmethcathinone, 4-MMC) with Associated Sympathomimetic Toxicity. Journal of Medical Toxicology. PMID: 20358417