NICE fever guidelines for kids
Fever is the most common presentation to Paeds ED and it can be difficult to identify a focus. This causes us (me anyway) a great deal of concern. After 10 years in paediatrics it still is the one thing weighing at the back of my mind – how to identify the child with the life-threatening bacterial infection amongst all the viral illnesses. NICE have updated their guidance in May 2013.
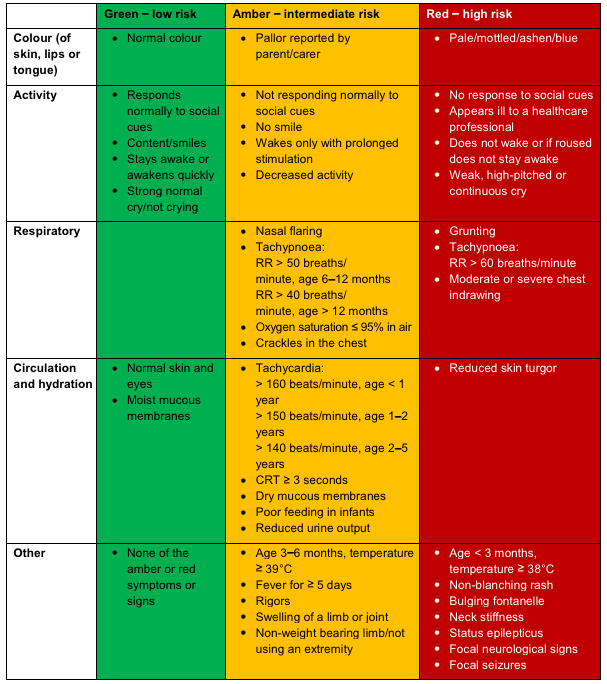
Often, they make it easy for us. Knowing how to recognise a sick child comes pretty early on in your paediatric experience. It’s the ones that don’t look desperately sick that are tricky. Let’s be honest, at 4am, every hot child looks miserable and sleepy. You need to have a system and the NICE guideline offers a great framework, focusing around their traffic light system.
Here are the points that are most useful to those of us assessing kids in ED.
Temperature measurement myths dispelled
The NICE guidance clarifies the numbers. If a <3 month old has a temp of 38 or more then that puts them into red. If a 3-6 month old has a temp of 39 or more then they are amber. But the height of the temp once over 6 months old does not correlate with the severity of the illness.
Diagnosis
- Consider signs of meningitis; UTI; pneumonia; meningococcal disease; herpes simplex encephalitis. But also don’t forget about septic arthritis or osteomyelitis (easily missed).
- As an additional point always think of Kawasaki disease in a fever lasting more than 5 days.
The importance of tachycardia
- This is one of the most valuable lessons I have learned and it has changed my practice over the last couple of years. I rarely send home a child with tachycardia when they have a fever of no clear focus.
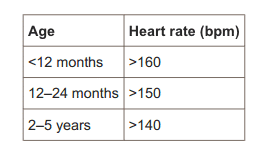
- NICE now says that tachycardia puts the child into amber.
Management – under 3 months
- If <3 months with a fever then investigate with bloods (FBC, CRP, B/C), urine and CXR/stool culture if indicated.
- Perform a lumbar puncture if: less than 1 month; 1-3 months and unwell; or 1-3 months with WCC<5×109/L or >15×10/L.
- Give IV antibiotics for the same criteria as the LP (i.e. if you’ve done a lumbar puncture for the above reasons, then they should be getting IV antibiotics).
Management – 3 months or older
- Investigate fever with no source if they have any red features – FBC, CRP, B/C and urine. Consider LP, CXR, UEC and gas if indicated.
- Investigate fever with no source if there are any amber features unless deemed unnecessary by an experienced paediatrician. This is clearly the greyest area. My rule of thumb is that if they look well (clinical judgement), and are not tachycardic then I would not bother doing bloods – NICE doesn’t offer any further advice on this unfortunately.
- Check urine for all children with fever (over 37.5) and no source, even if they are green.
Antipyretics
- As well as the meds, children should not be over-wrapped or underdressed. And tepid sponging is not recommended.
- Use either paracetamol or ibuprofen but only for a child who appears distressed and not simply to bring down the fever. Don’t give both agents together and only switch agents if the child remains distressed.
When to discharge
- Do not rely on the temp coming down with antipyretics to distinguish between serious and non-serious illness.
- Any child with amber or red features should be reassessed after 1-2 hours.
When to admit
Use your usual markers of clinical conditions but also other social factors should help with decision: social circumstances; parental anxiety and instinct; serious infectious contacts; travel abroad; repeated presentations; when the child has remained ill for longer than expected for a self-limiting illness.
How to discharge
Give the parents advice on recognising red or amber signs by providing written information and/or arranging follow-up.
New in 2013
- Assess children using the new traffic light system to predict risk of serious illness (red: high-risk, amber: intermediate-rish, green: low-risk)
- Recognise the importance of tachycardia and that this puts children into the amber (intermediate-risk category)
- Any child younger than 3 months with fever should be investigated
- Alternate antipyretics and don’t use both at the same time
- Recognise that lowering the temp does not prevent febrile convulsions
Consultant in Paediatric Emergency Medicine at the Royal London Hospital and a Senior Lecturer at Queen Mary University of London | Don't Forget The Bubbles |


New update in 2019, not much changed .