Rapid descent
aka Pulmonary Puzzler 008
A 30 year old male presents with a 3 day history of fevers and increasing breathlessness. On presentation he is noted to be severely hypoxic with sats of 80% on room air.
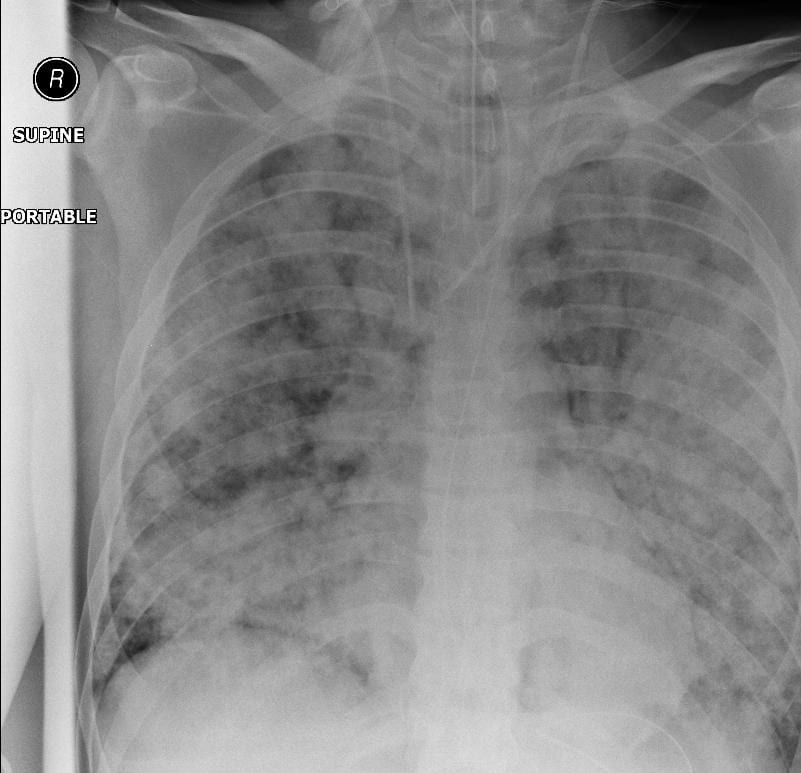
The following chest X-ray is obtained:
Questions
Q1. Describe the chest X-ray and outline the differential diagnosis
Answer and interpretation
There are diffuse bilateral pulmonary infiltrates which have a nodular appearance.
The differential diagnosis here includes infectious causes such as viral pneumonia and typical and atypical causes of bacterial pneumonia. Non-infectious causes would include hypersensivity pneumonitis and diffuse alveolar haemorrhage.
The short history favors an infectious aetiology.
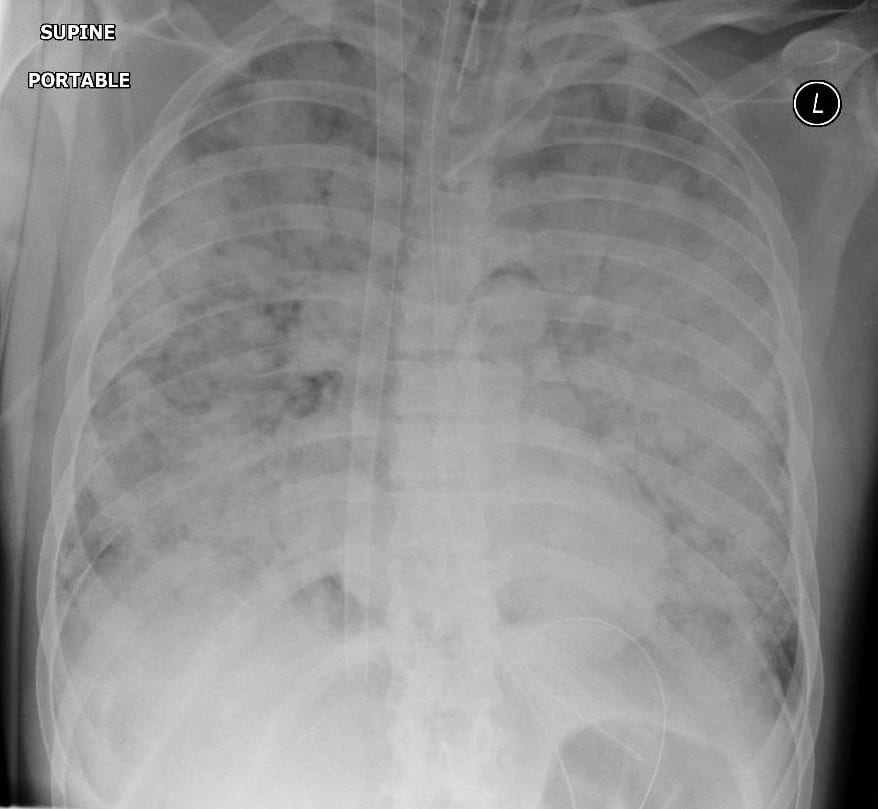
The patient is admitted to the intensive care unit and continues to deteriorate with an increasing oxygen requirement. An arterial blood gas shows a PaO2 of 55 on 15L O2 via a facemask. The respiratory rate rises to the high 40s. Another chest X-ray is obtained
Q2. Describe the chest X-ray now. What would you do next? What problems would you anticipate?
Answer and interpretation
The chest X-ray shows worsening of the previous alveolar infiltrates.
The combination of the early rapid progression in the clinical and radiological course combined with the severity of the hypoxia indicates that intubation is required.
Non invasive ventilation is not a good option here (except while preparing to intubate) as delaying intubation further here is only likely to make the procedure more dangerous by further limiting the patient’s reserve. The problem that you need to need to anticipate here is rapid desaturation and potential difficulty obtaining adequate oxygenation with bag-mask ventilation if/ when that occurs.
Over the following 12 hours the patients condition continues to worsen to the point that the patient is frequently desaturating on 100% oxygen with a PEEP of 18.
You are asked to see the patient because the patient has desaturated to 80% on the above settings. The ventilator appears to be working appropriately. On examination, you find the right chest is moving less than the left and there is less air entry on that side.
Q3. What do you do now?
Answer and interpretation
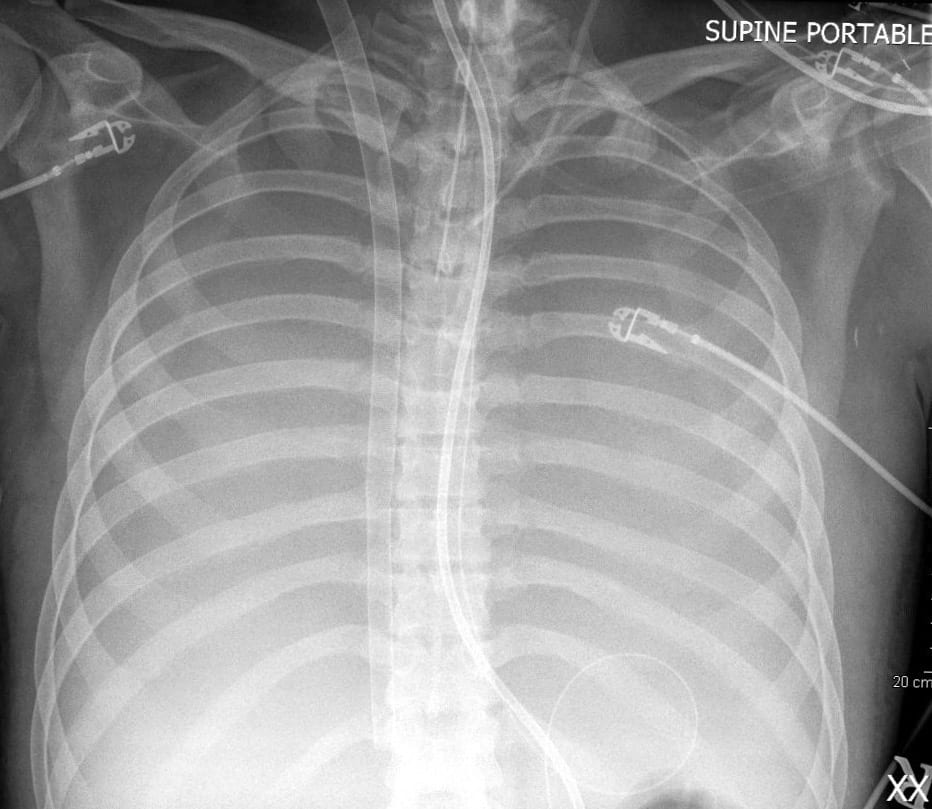
Order a chest X-ray.
Even if you are very strongly suspicious that there is a pneumothorax you should not perform needle decompression here. It is likely given the clinical context that the change here represents progression of disease. If there is no pneumothorax and you create one there is a significant risk that the patient will die.
In this case, there was no pneumothorax:
Q4. What are the options for improving oxygenation now?
Answer and interpretation
This patient is failing conventional ventilation. The options for improving oxygenation are:
- nitric oxide
- prone ventilation
- inverse ratio ventilation
- ECMO
- High Frequency Jet Ventilation
A non-conventional ventilation strategy is employed and the following chest X-ray is obtained:
Q5. Describe the chest X-ray.
Answer and interpretation
This x-ray shows an ECMO cannula inserted via the right internal jugular route.
With this particular cannula, venous blood is taken from the superior vena cava and the inferior vena cava. It is then oxygenated and the cannula has a third lumen which allows arterialised blood to be directed towards the tricuspid valve in the right atrium under TOE guidance.
Q6. Case Outcome
References
- For more Pulmonary cases check out the LITFL Top 150 Chest X-Rays

CLINICAL CASES
Pulmonary Puzzler
Intensivist in Wellington, New Zealand. Started out in ED, but now feels physically ill whenever he steps foot on the front line. Clinical researcher, kite-surfer | @DogICUma |