R&R In The FASTLANE 106
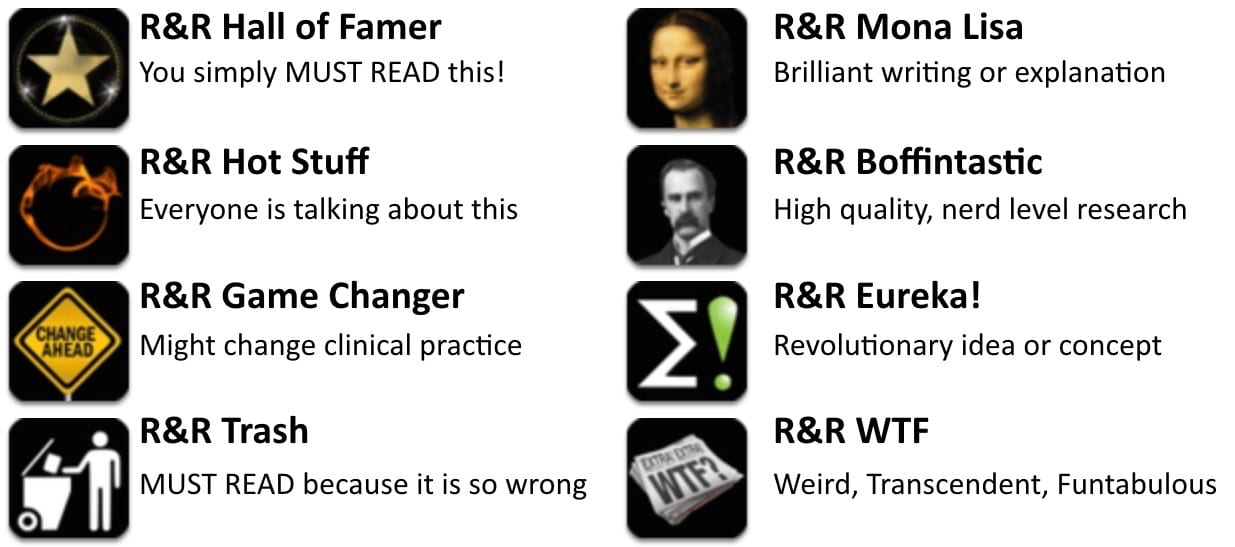
Welcome to the 106th edition of Research and Reviews in the Fastlane. R&R in the Fastlane is a free resource that harnesses the power of social media to allow some of the best and brightest emergency medicine and critical care clinicians from all over the world tell us what they think is worth reading from the published literature.
This edition contains 6 recommended reads. The R&R Editorial Team includes Jeremy Fried, Nudrat Rashid, Soren Rudolph, Anand Swaminathan and, of course, Chris Nickson. Find more R&R in the Fastlane reviews in the : Overview; Archives and Contributors
This Edition’s R&R Hall of Famer
Young , et al. Effect of a Buffered Crystalloid Solution vs Saline on Acute Kidney Injury Among Patients in the Intensive Care Unit. JAMA 2015. PMID 26444692
- There’s been an increasing feeling, supported by some mediocre literature, that there’s an association between administration of 0.9% NaCl and acute kidney injury and hyperchloremic metabolic acidosis. The SPLIT trial, an RCT examining ICU patients randomized to plasma-lyte (balanced solution) vs 0.9% NaCl, found no difference in incidence of AKI, renal replacement therapy, or mortality. However, most patients received approximately 2L of fluids, likely not enough to show a difference. Isotonic saline? Probably ok in small quantities.
- Recommended by Lauren Westafer
- Read More: SPLIT Trial Published. Saline or Plasmalyte on the ICU (St. Emlyn’s), The SPLIT Trial: Saline vs. Plasma-Lyte Fluid Therapy (REBEL EM), FOAMCastini – Core Content Journal Club (FOAM Cast)
Semier MW et al. Randomized Trial of Apneic Oxygenation during Endotracheal Intubation of the Critically Ill Am J Respir Crit Care Med. 2015. PMID: 26426458
- Apneic oxygenation has been widely adopted for airway management in the ED despite the absence of literature focusing on ED or critical patients. This study investigated the use of apneic oxygenation in the ICU. The researchers found no difference in the lowest O2 sat. However, it’s unclear if this study is applicable to the ED setting and it likely does not reflect our standard management (33% had BPAP during apnea, 40% had BVM during apnea). For now, collective anecdotes of efficacy reign while we await research in the ED setting.
- The authors conclusion is that apneic oxygenation does not appear to increase lowest arterial oxygen saturation during endotracheal intubation of critically ill patients compared to usual care. Although this is the first randomized clinical trial of apneic oxygenation my 2 cents for this study is that they excluded the sickest patients and we all know the keys to avoid desaturation are preparation, pre-oxygenation, patient positioning, and 1st pass intubation. The point of apneic oxygenation is to delay desaturation, not prevent it.
- Recommended by Justin Morgenstern, Anand Swaminathan, & Salim R. Rezaie
- Further information: The FELLOW Trial: An End to Apneic Oxygenation? (REBEL EM), The last breath for apnoeic oxygenation? (St Emlyn’s: JC), Podcast 158 – The FELLOW Trial on Apneic Oxygenation in ICU Patients (EMCrit)
Cunningham S et al. Oxygen saturation targets in infants with bronchiolitis (BIDS): a double-blind, randomised, equivalence trial. Lancet 2015; 386(9998):1041-8. PMID: 26382998
- This is another article investigating mild hypoxia (> 90%) in bronchiolitis and whether normoxia (> 94%) is important using falsely elevated O2 displays. This group found that there was no difference in the time to resolution of cough whether the patient was randomized to the falsely elevated O2 sats (i.e. their sat was 90-94% but monitor read as 94% or greater) or normal O2 sats. Additionally, out of 515 patients enrolled, there were no differences in serious adverse events. This is further evidence that we shouldn’t focus on numbers but rather the overall patient appearance.
- Recommended by Anand Swaminathan
Scales DC et al. Unintentional Continuation of Medications Intended for Acute Illness After Hospital Discharge: A Population-Based Cohort Study. J Gen Intern Med 2015. PMID 26369941
- Much of what we do in the acute setting is about getting patients on the meds they need to save their lives now. We know those medications are supposed to be only temporary.
- Turns out our hospital systems are pretty bad at stopping them.
- Morandi and colleagues have suggested that patients off leave the hospital on inappropriate medications. (PMID: 23855843 and 21670372), particularly antipsychotics. But it was possible to ignore those studies, since they were in modest size cohorts with limited follow-up.
- Scales et al use Ontario wide-data to show that this is not a limited problem. They examined provincial data for more than 1 million older patients hospitalized between 2003 and 2011. They looked at how often patients were sent home on medications that were started in the hospital.
Even better, they were able to carefully confirm that the medications had not been used or indicated in the year before the hospitalization, and (very cleverly!) were not indicated on an ongoing basis afterwards. - Tens of thousands of patients went out on new antipsychotics, benzos, gastric acid suppression and inhalers. About a third were still on the meds a year later, still without an indication. The total cost of these meds they estimate at CAN$ 18,693,043. And that’s assuming there were no side-effects of any of these meds–which we know must not have been true. Clearly, we need to design better systems for handing off patients out of the acute setting to indicate that medications should be stopped on completion of a time-limited course.
- Recommended by Theodore J Iwashyna
Friedman, B.D, et al. Naproxen With Cyclobenzaprine, Oxycodone/Acetaminophen, or Placebo for Treating Acute Low Back Pain A Randomized Clinical Trial. JAMA Oct 2015. PMID 26501533
- An outstanding study which examines how we can best care for our patients who present with low back pain. The authors included patients with acute, non traumatic back pain without radicular symptoms; and examined the effect of naproxen with either placebo, cyclobenzaprine, or oxycodone/acetaminophen. At 7 days and 3 months, there was no significant difference in disability or pain control between placebo and use of the other medications. If you’re currently providing your patients with muscle relaxants or opioids in addition to NSAIDs, this study demonstrates the futility of that approach for the majority of your patients.
- Recommended by Jeremy Fried
Emergency physician with interest in education and knowledge translation. #FOAMed Fan | @jdfried |







http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0020124
http://www.ncbi.nlm.nih.gov/pubmed/12775614