R&R In The FASTLANE 115
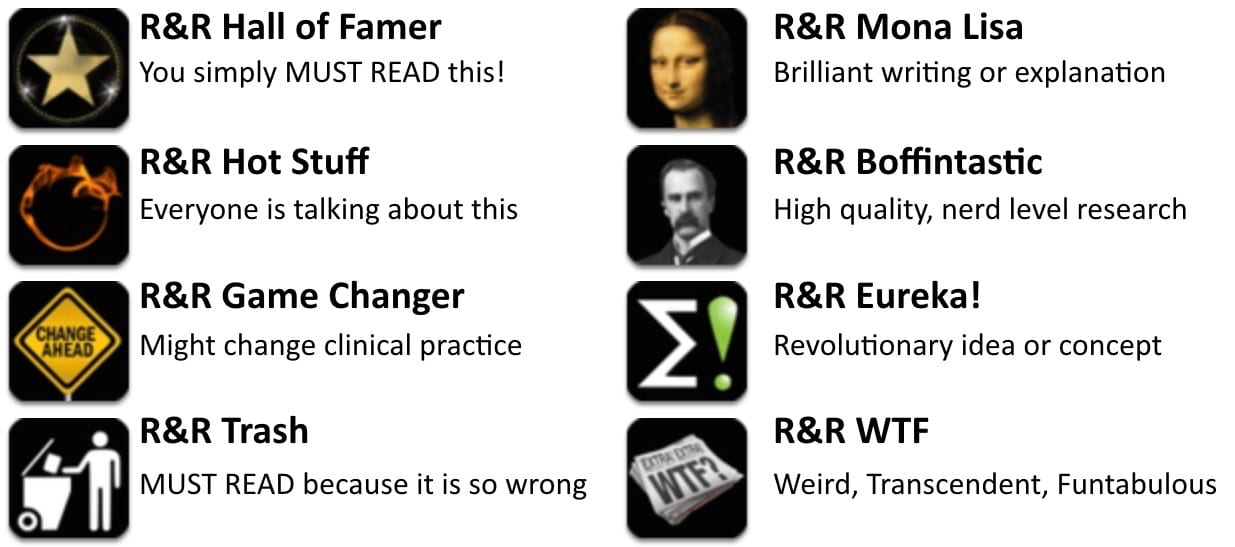
Welcome to the 115th edition of Research and Reviews in the Fastlane. R&R in the Fastlane is a free resource that harnesses the power of social media to allow some of the best and brightest emergency medicine and critical care clinicians from all over the world tell us what they think is worth reading from the published literature.
This edition contains 6 recommended reads. The R&R Editorial Team includes Jeremy Fried, Nudrat Rashid, Soren Rudolph, Anand Swaminathan and, of course, Chris Nickson. Find more R&R in the Fastlane reviews in the : Overview; Archives and Contributors
This Edition’s R&R Hall of Famer
Fassier T et al. Who Am I to Decide Whether This Person Is to Die Today? Physicians’ Life-or-Death Decisions for Elderly Critically Ill Patients at the Emergency Department-ICU Interface: A Qualitative Study. Ann Emerg Med 2015. PMID: 26619758
- This fascinating piece of qualitative research is a rich and complex look at decision making performed by resuscitationists for the critically ill elderly patient. Specifically, the authors interviewed emergency physicians and intensivists at multiple sites in France, examining their decision making process regarding whether or not to further resuscitate elderly patients. We all know this is a complex process, with layers within layers of issues, and the authors do a commendable job of breaking them down. In a nutshell, the authors recommend that future educational strategies to improve decision making focus on: -the influence of cognitive/affective biases -physician conflicts -communication gaps between ED and ICU providers A worthwhile read for all of us who deal with this issue daily, and a good reminder of how to possibly better make these important decisions.
- Recommended by: Jeremy Fried
Bellezzo JM et al. Emergency physician-initiated extracorporeal cardiopulmonary resuscitation. Resuscitation 2012;83: 966-970. PMID: 22306260
- There is growing interest in veno-arterial extracorporeal membrane oxygenation (VA ECMO), also called extracorporeal cardiopulmonary resuscitation (ECPR), amongst emergency physicians. It is considered in cases of refractory cardiopulmonary failure, including cardiac arrest after massive MI. This is a small retrospective observational study serving as proof of concept that ECMO can be initiated by emergency physicians in a highly selected group of patients.
- Recommended by: Meghan Spyres
Guliani S et al. Central aortic wire confirmation for emergent endovascular procedures. J Trauma Acute Care Surg 2015; 79(4):549-554. PMID: 26402527
- Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) is increasingly popular as a replacement for the morbid resuscitative thoracotomy in trauma. Confirmation of guidewire placement can be difficult in some settings as it requires fluoroscopy or x-ray. This pilot study looked at the successful identification of guidewire using ultrasound. In this study, these were patients undergoing angiography, not REBOA, but found that ultrasound works. Surgeons correctly identified the guidewire in 97/100 and 98/100 cases in sagittal and transverse reviews, respectively. Ultrasound to confirm guidewire placement? Seems reasonable.
- Recommended by: Lauren Westafer
Poonai N et al. Oral administration of morphine versus ibuprofen to manage postfracture pain in children: a randomized trial. CMAJ 2014;86(18):1358-63 PMID: 25349008
- Analgesia in fractures is always a very important component of the management, with the concern of not being aggressive enough on its management, specially in pediatric population. This study compares adequate doses of oral morphine vs. ibuprofen for uncomplicated fractures. Remarkable, there was no differences in efficacy but a trend to more complications in the morphine group. Interestingly 25% of the kids in either group, did not require analgesia at all.
- Recommended by: Daniel Cabrera
Donnino MW et al. Temperature Management After Cardiac Arrest An Advisory Statement by the Advanced Life Support Task Force of the International Liaison Committee on Resuscitation and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation 2015. PMID: 26449873
- This publication is the ILCOR advisory statement on temperature management after cardiac arrest. The group basically states that in OHCA with an initial shockable rhythm, patients with ROSC should be cooled to somewhere between 32 and 36 degrees Celsius. In effect, the group endorses the temperature goal from the HACA group and Bernard et al in 2002 AND the Nielsen study from 2013. Unfortunately, this statement adds no clarity to the debate.
- Recommended by: Anand Swaminathan
Mekontso Dessap et al. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med 2015. PMID: 26650055
- The increased right ventricular afterload in ARDS could induce Acute CorPulmonale (ACP). This multi-site study prospectively looked at patients on lung protective ventilation using trans-oesophageal echocardiography to diagnose ACP and reported a 22 % prevalence of ACP and a poor outcome of severe ACP. The authors also propose a simple clinical risk score {which includes the following 4 variables, pneumonia as a cause of ARDS, driving pressure ≥18 cm H2O, arterial oxygen partial pressure to fractional inspired oxygen (PaO2/FiO2) ratio <150 mmHg, and arterial carbon dioxide partial pressure ≥48 mmHg} for early identification of ACP that could trigger specific therapeutic strategies to reduce RV afterload.
- Recommended by: Nudrat Rashid
Intensivist and Donation Medical Specialist, Australia | @NudratRashid |