R&R In The FASTLANE 133
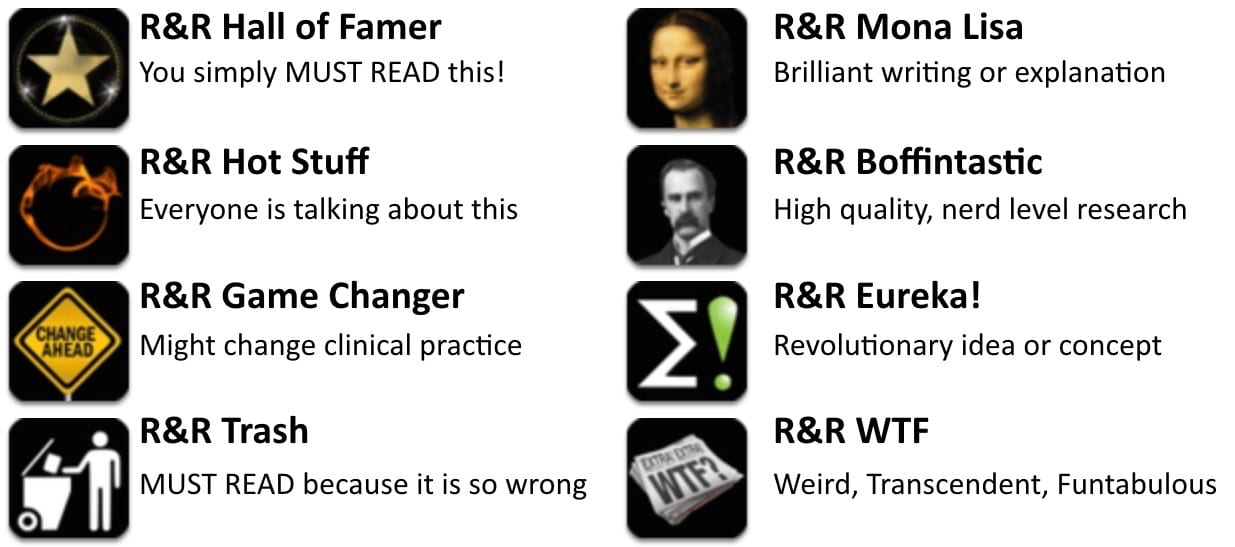
Welcome to the 133rd edition of Research and Reviews in the Fastlane. R&R in the Fastlane is a free resource that harnesses the power of social media to allow some of the best and brightest emergency medicine and critical care clinicians from all over the world tell us what they think is worth reading from the published literature.
This edition contains 6 recommended reads. The R&R Editorial Team includes Jeremy Fried, Nudrat Rashid, Soren Rudolph, Anand Swaminathan and, of course, Chris Nickson. Find more R&R in the Fastlane reviews in the : Overview; Archives and Contributors
This Edition’s R&R Hall of Famer
Reade MC, et al; DahLIA Investigators and the Australian and New Zealand Intensive Care Society Clinical Trials Group. Effect of Dexmedetomidine Added to Standard Care on Ventilator-Free Time in Patients With Agitated Delirium: A Randomized Clinical Trial. JAMA. 2016 Mar 15. PMID: 26975647.
- This was a multicentre, double blind, placebo controlled, parallel group randomised clinical trial of 74 adult ICU patients who could not be extubated due to agitation and delirium. The addition of Dexmedetomidine to standard care compared with standard care alone (placebo) in these patients resulted in more ventilator-free hours at 7 days, earlier extubation and accelerated resolution of delirium. This study certainly suggests a benefit to using Dexmedetomidine in these patients.
- Recommended by: Nudrat Rashid
Mark DG, et al. False negative interpretations of cranial computed tomography in aneurysmal subarachnoid hemorrhage. Academic Emerg Med. 2016. PMID: 26918885
- This chart review identified 452 patients diagnosed with subarachnoid hemorrhage and looked at the subset of 18 patients (4%) who were diagnosed by lumbar puncture after a normal CT. The supposedly normal CTs were then reviewed by 2 specialty neuro-radiologists, and in 9 of the 18 patients the neuro-radiologists thought there was evidence of bleed on the scan initially reported as normal. The false negative rate was 71% (5 of 7) for the scans done within 6 hours of headache. Of course, re-reading studies without the time pressures of a normal shift, especially after an LP has already shown blood (although these radiologists were blinded) is probably easier. Bottom line: Radiology isn’t perfect. This might still be the fatal flaw in the famous Perry study.
- Recommended by: Justin Morgenstern
Chang AK, et al. Efficacy of an Acute Pain Titration Protocol Driven by Patient Response to a Simple Query: Do You Want More Pain Medication? Annals of Emerg Med. 2015. PMID: 26074387
- How can you tell if your patient needs more pain medicine? This study supports the common sense approach: just ask them. I’ve always liked this approach, and it left 97% of patients satisfied or very satisfied with their pain control. The only problem is it wasn’t compared to other strategies, so we can conclude that this method controls pain, we just don’t know if it is any better than other methods.
- Recommended by: Justin Morgenstern
Beadle KL et al. Isopropyl alcohol nasal inhalation for nausea in the Emergency Department: A randomized controlled trial. Ann Emerg Med. 2015. PMID: 26679977
- This is a small double-blinded RCT comparing inhaled isopropyl alcohol to saline placebo for short-term relief of nausea in the ED. Although it is hard to believe patients (and possibly investigators) were truly blinded to the odor of isopropanol, this study found isopropanol superior to placebo for improvement of nausea at ten minutes. This effect may be short lived however, as there was no difference in subsequent use of antiemetics between the two groups. In light of recent attention to possible side effects of existing medications, including prolongation of the QT interval with ondansetron, isopropyl alcohol pads offer an intriguing option for short-term relief of nausea in the ED.
- Recommended by: Meghan Spyres
Wasserstein RL, Lazar NA. The ASA’s statement on p-values: context, process, and purpose. The American Statistician. 2016. doi:10.1080/00031305.2016.1154108
- Statistical significance and p values are widely touted, proudly displayed, and increasingly reported. Yet p values are problematic, so much so the American Statistical Association created a statement essentially calling the literature out for misuse. P values indicate how incompatible the data are with a specific statistical model. They NEITHER reflect the probability that the null hypothesis is true (they are calculated assuming the null hypothesis is true) NOR the probability that the data were produced by chance alone. P values also do not measure effect size or significance. We see a great deal of research overturned and it appears that misused statistics may be to blame. Handle p values cautiously.
- Recommended by: Lauren Westafer
Gabayan GZ, et al. Poor Outcomes After Emergency Department Discharge of the Elderly: A Case-Control Study. Ann Emerg Med. 2016; PMID: 26947799
- If you were thinking of admitting that elderly patient, maybe you should – and other (weak) predictors of demise after Emergency Department discharge.
- Recommended by: Ryan Radecki
Intensivist and Donation Medical Specialist, Australia | @NudratRashid |