R&R In The FASTLANE 144
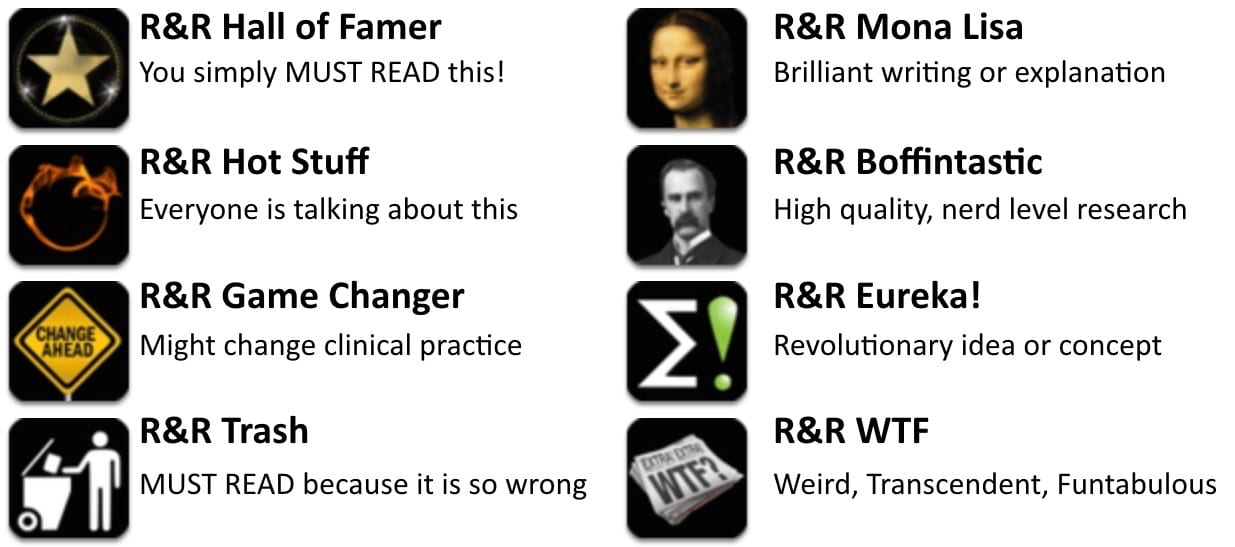
Welcome to the 144th edition of Research and Reviews in the Fastlane. R&R in the Fastlane is a free resource that harnesses the power of social media to allow some of the best and brightest emergency medicine and critical care clinicians from all over the world tell us what they think is worth reading from the published literature.
This edition contains 6 recommended reads. The R&R Editorial Team includes Jeremy Fried, Nudrat Rashid, Soren Rudolph, Anand Swaminathan and, of course, Chris Nickson. Find more R&R in the Fastlane reviews in the : Overview; Archives and Contributors
This Edition’s R&R Hall of Famer
Ortiz M, et al. Randomized comparison of intravenous procainamide vs. intravenous amiodarone for the acute treatment of tolerated wide QRS tachycardia: the PROCAMIO study. European heart journal. 2016. PMID: 27354046
- The evidence for amiodarone has always been on the weak side. This is a good paper that should be practice changing for some people. It is a multicenter, randomized trial comparing amiodarone (5mg/kg over 20 minutes) to procainamide (10mg/kg over 20 min) in 74 adult patients with hemodynamically stable ventricular tachycardia. Procainamide was better. The primary outcome of cardiac adverse events (mostly hypotension requiring cardioversion), occurred in 9% of the procainamide group and 41% of the amiodarone group (odds ratio 0.1, 95%CI 0.03-.06, p=0.006). In terms of stopping the v.tach, procainamide worked 67% of the time as compared to only 38% with amiodarone (OR = 3.3; 95% CI 1.2-9.3; P = 0.026). Unfortunately, the trial was originally designed to include 300 patients, but they stopped it early because of slow recruitment. However, this comparison may not be all that relevant to you if, like me, you prefer to go straight to electricity in these patients.
- Recommended by Justin Morgenstern
- Further reading The Case of the Dysrhythmic Heart (EM Nerd)
Wray CM, Loo LK. The Diagnosis, Prognosis, and Treatment of Medical Uncertainty. Journal of graduate medical education 2015. PMID: 26692960
- This is an nice editorial reviewing uncertainty in medicine that is worth reading. They point out that no matter how much information we are able to gather, the inherent complexity of human life, the variability of presentations, and the fact that we cannot predict the future will always leave us with an intrinsic uncertainty. They point out the problem in medical education in that we value certainty from our students, and present them with black and white multiple choice exams that don’t well represent the grey of real life medicine. They close with an excellent quote from Sir William Osler: “A distressing feature in the life of which you are about to enter … is the uncertainty which pertains not alone to our science and art, but the very hopes and fears which make us men. In seeking out the absolute truth we aim for the unattainable, and must be content with finding broken portions.’’
- Recommended by Justin Morgenstern
Bijur PE, et al. Temperature measurement in the adult emergency department: oral, tympanic membrane and temporal artery temperatures versus rectal temperature. Emerg Med J 2016. PMID: 27334759.
- Does your patient have a fever? This seemingly simple question can oftentimes be difficult to answer. These authors attempted to answer which of the various non invasive methods (oral, tympanic, temporal artery) best answers that question when compared with rectal temperature as the gold standard. Surprisingly, tympanic membrane measurement was the most precise with a cutoff of 37.5C (99.5F) having high specificity and sensitivity. Previously, I have asked for an oral temperature when I question the accuracy of the tympanic membrane measurement. It seems time to let go of that practice and simply move to the more invasive measurement if the temperature is going to have clinical import in the patient’s care.
- Recommended by Jeremy Fried
Carpenter CR et al. Spontaneous Subarachnoid Hemorrhage: A Systematic Review and Meta-Analysis Describing the Diagnostic Accuracy of History, Physical Exam, Imaging, and Lumbar Puncture with an Exploration of Test Thresholds. Acad Emerg Med 2016. PMID: 27306497
- This is an excellent systematic review and meta-analysis looking at the test characteristics of different components of the history, physical exam and testing in suspected SAH. The critical findings are:
- Neck Pain: (+)LR = 4.1
- Neck Stiffness: (+)LR = 6.6
- NCHCT < 6 hours: (+)LR = 230, (-)LR = 0.01
- NCHCT > 6 hours: (-)LR = 0.07
- Overall, the group concludes that an LP is only useful when the post-NCHCT probability of SAH is > 5% which corresponds to a pre-NCHCT probability of ~ 20%. Basically, high risk patients should have strong consideration for an LP after a negative NCHCT even within 6 hours. For the low-risk patients, perhaps NCHCT is enough.
- Recommended by Anand Swaminathan
Quill TE, et al. Discussing treatment preferences with patients who want “everything”. Annals of internal medicine 2009. PMID: 19721022
- “When asked about setting limits on medical treatment in the face of severe illness, patients and their families often respond that they want “everything.” ” If you struggle with an approach to this common and difficult situation, this article will help you.
- Recommended by CPN
Hermann LK, et al. Comparison of frequency of inducible myocardial ischemia in patients presenting to emergency department with typical versus atypical or nonanginal chest pain. Am J Cardiol 2010 PMID: 20494662.
- Great paper from Mount Sinai in NYC: they analyzed HPIs for all 2500 ED stress tests done from 2004-2008 and found the rate of positives is the same, regardless of whether the patient had “typical” chest pain, “atypical” chest pain, or no chest pain (non-chest pain anginal equivalents). Most useful for convincing the skeptical “well it’s atypical…”
- Recommended by Seth Trueger
Emergency physician with interest in education and knowledge translation. #FOAMed Fan | @jdfried |