R&R In The FASTLANE 155
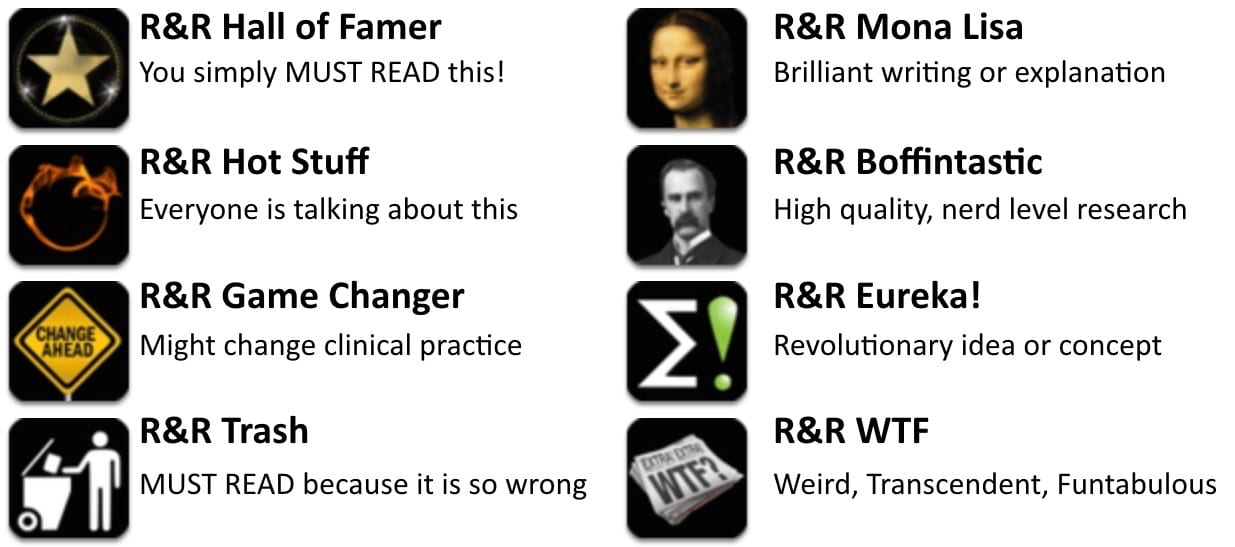
Welcome to the 155th edition of Research and Reviews in the Fastlane. R&R in the Fastlane is a free resource that harnesses the power of social media to allow some of the best and brightest emergency medicine and critical care clinicians from all over the world tell us what they think is worth reading from the published literature.
This edition contains 4 recommended reads. The R&R Editorial Team includes Jeremy Fried, Nudrat Rashid, Soren Rudolph, Anand Swaminathan and, of course, Chris Nickson. Find more R&R in the Fastlane reviews in the : Overview; Archives and Contributors
This Edition’s R&R Hall of Famer
Smith DD et al. Does emergency physician empathy reduce thoughts of litigation? A randomised trial. EMJ. 2016. PMID 27002161
- This is a randomized, controlled trial of a convenience sample of 437 patients sitting in an emergency department waiting room. The participants were shown videos of discharge instructions between a physician and a patient (actor). In half of the videos, there were two specific empathic statements included. The statements were: “verbalisations that (1) the physician recognises that the patient is concerned about their symptoms and (2) the patient knows their typical state of health better than a physician seeing them for the first time and did the right thing by seeking evaluation”. The participants were then asked how likely they were to sue the doctor if there were to be a missed diagnosis. The empathy group was statistically less likely to think about sueing the doctor, although I am not sure how important the magnitude of the difference is (mean Likert scale 2.66 vs 2.95, difference -0.29, 95% CI -0.04 to -0.54, p=0.0176). The big problem is, obviously, that fake decisions to sue after watching a video are going to be very different from real decisions to sue. But I don’t care so much about being sued (maybe that is the Canadian in me). Displaying empathy towards patient complaints on one of the scariest days of their life is just part of being a decent human being (let alone a good doctor). Bottom line: A few simple sentences probably go a long way towards displaying your empathy towards emergency department patients.
- Recommended by Justin Morgenstern
Anderson CS et al. Low-Dose versus Standard-Dose Intravenous Alteplase in Acute Ischemic Stroke. NEJM 2016. PMID 27161018
- Is low-dose (0.6 mg/kg) tPA non-inferior to standard dose (0.9 mg/kg) tPA in ischemic CVA? The simple answer from this article is no but the truth is far more complicated. Low-dose tPA exceeded the upper limit for non-inferiority for the combined endpoint of death or disability. However, secondary outcomes showed that patients receiving low-dose tPA were less likely to be dead at 7 and 90 days and were half as likely (1% vs 2.1%) to develop ICH. Despite not meeting the preset non-inferiority standard, there may yet be a role for low-dose tPA.
- Recommended by Anand Swaminathan
Friedman BW, et al. Diphenhydramine as Adjuvant Therapy for Acute Migraine: An Emergency Department-Based Randomized Clinical Trial. Ann Emerg Med 2016. PMID 26320523
- Looks like diphenhydramine doesn’t help all-comers with migraines in the ED. My bet is there might be a subset of patients it does help; if the patient has had it before and requests it, sure. But no longer a routine part of my migraine cocktail.
- Recommended by Seth Trueger
- Prehospital physians vs paramedics…the war rages on!In this large population-based observational study of 21,165 persons with OHCA over a 7-year period the association between prehospital physician involvement and 30-day survival was examined.
Using logistic regression analysis to assess the association between 30-day survival and involvement of a physician at any time before arrival at the hospital the authors found that overall 10.8% of OHCA patients with physician involvement and 8.1% of OHCA patients without physician involvement before arrival at hospital were alive after 30 days. This was also found for 1-year survival, but with less certainty. Physician involvement was also positively associated with ROSC, OR=1.09 (95% CI=1.00-1.19); and with 1-year survival, OR=1.13 (95% CI=0.99-1.29).1 point goes to the physicians – awaiting the next battle! - Recommended by Soren Rudolph
Hamilton A et al. Association between prehospital physician involvement and survival after out-of-hospital cardiac arrest: A Danish nationwide observational study. Resuscitation 2016. PMID 27565859
Senior Consultant Anesthesiologist, Traumemanager and PHEM doctor. Dedicated to trauma resuscitation, prehospital care and airway management. Barometerbarn | @SorenRudolph |






“Prehospital physicians vs paramedics…the war rages on!”
Regular reader, love the site. I just think it’s too bad that important research into pre-hospital resuscitation has to be couched in the language of combat! Not only is it unnecessarily adversarial but from any perspective–educational, institutional, clinical–‘war’ between paramedics and physicians seems like the proverbial tussle between David and Goliath. Save for the original’s aberrant outcome.
Brandon A
-Advanced Care Paramedic, BCEHS