Seizing and No Access
aka Ruling the Resus Room 002
A 28 year-old male is brought in by paramedics with ongoing generalised tonic/clonic seizures. They have continued for 35 minutes. The paramedics have given 15mg of Midazalam IM with no effect, and were unable to gain IV access due to extensive track marks over the patient’s veins from extensive IV drug use.
Vascular access is urgently needed to terminate this state of status epilepticus and to prevent further neurological sequelae. You consider placing a central line but don’t like the idea of even a few minutes delay, nor the idea of a moving target…
You decide to reach for the EZ-IO to obtain intraosseous access in seconds.
Questions
Q1. Describe the history of the intraosseous catheter?
Answer and interpretation
The intraosseous route and device was first discovered and developed in 1922, and became popular during World War II for resuscitating combat victims. However popularity soon died off with the advent of steel needles and plastic peripheral cannulas. A resurgence was seen between 1980 and 2000 in paediatric patients that had difficult vascular access and needed rapid access for resuscitation purposes. However, since the middle of the last decade intraosseous use has really taken off, and it is now widely used and accepted in adult patients, particularly in emergent situations but also in some non-emergent situations.
The devices have dramatically changed over the years. The early days saw the use of the modified manual Dickmann Needle and the Jamshidi Needle, and now we have equipment like the Bone Injection Gun and the popular power-driven EZ-IO.
The bone marrow space allows for a non-collapsible vein to be created, and allows rapid access to central circulation.
The EZ-IO is one of the most popular devices currently in use in emergency departments and is the device the LITFL team are most familiar with. The EZ-IO can insert a catheter into the intraosseous space within 10 seconds, has a 92-97% first pass success rate, and can manage 5-9 liters of fluid per hour through a single catheter hub.
Q2. What are the indications for intraosseous catheter/infusion?
Answer and interpretation
Intraosseous access should be considered in patients who:
- are critically ill and peripherally shut-down
- have an immediate need for drugs and fluids
- previously required central venous access for infusion due to difficult vascular access
- have limited or no vascular access
- require multiple IV sticks to obtain vascular access for medication or fluid infusion
- immediate pain management
- need immediate fluid resuscitation
- are in cardiac or respiratory arrest
- require rapid intubation or sedation
- are experiencing a psychiatric emergency
- are involved in pre-hospital, disaster and mass casualty situations
Q3. What are the advantages of intraosseous over central venous access?
Answer and interpretation
- Quicker (seconds rather than minutes)
- Easier
- Cheaper ($100 vs $300)
- Multiple insertion sites are avaialble
- Less training and experience required
- Less complications and catheter related blood stream infections
- Less pain and discomfort during insertion
- the same drugs may be administered
- blood samples can be obtained for laboratory analysis
“Delivery of drugs via an endotracheal tube is no longer recommended – if IV access cannot be achieved, drugs should be given by the IO route”
— ILCOR 2010
The main disadvantage of intraosseous access is that haemodynamic monitoring is not possible.
Q4. What medications/fluids can be infused through an intraosseous catheter?
Answer and interpretation
Any medication/fluid you infuse through an IV/CVC can go be administered IO.
Some examples are provided in these case reports:
Q5. What anatomical locations and catheter sizes can be used with the EZ-IO?
Answer and interpretation
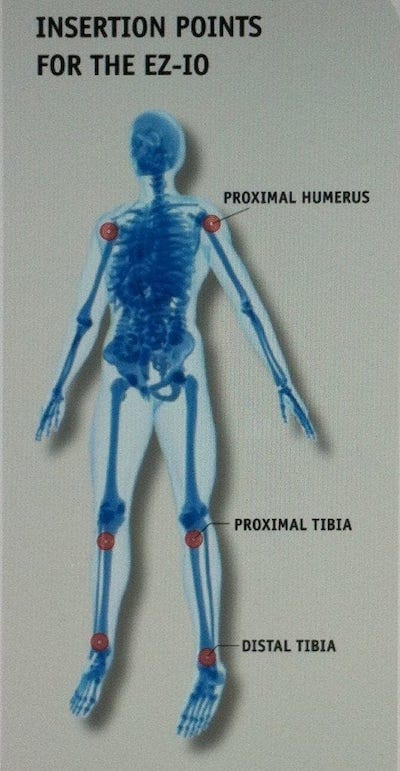
Currently recommended sites (from the manufacturer) for the EZ-IO are the:
- Proximal humerus – (Palpate the anterior mid-shaft humerus, and continue palpating proximally up the anterior surface of the humerus until the greater tubercle is met. Palpate the coracoid and acromion, then imagine a line between them. The insertion point is about 2cm from its midpoint).
- Proximal tibial – (In adults, two fingers’ breadths below and medial to the tibial tuberosity)
- Distal tibia – (In adults, two fingers’ breadths proximal to the tip pf the medial malleolus)
However any bone with an intraosseous space can be used to place an intraosseous catheter. Current literature and studies seem to favour the proximal humerus as the preferred site, as it is close to the heart and allows the quickest absorption of fluids/medications into the central circulation.
Selecting catheter size is similar to an IV with different sizes, for different ages and bone size:
- Pink — paediatric patients 3-39kg
- Blue — Patients >39kg
- Yellow — for patients with extensive soft tissues of insertion site.

Q6. What are the contraindications for intraosseous use?
Answer and interpretation
The intraosseous catheter is contra-indicated in the following situations:
- Previous IO attempts in the same bone
- Previous surgery at the same site (knee replacement, etc.)
- Osteogenesis imperfecta
- Osteoporosis
- Infection of the tissue overlying the insertion site
- Difficulty or inability to locate landmarks
Q7. What complications can occur from intraosseous catheters?
Answer and interpretation
Complications are rare, however the following have been reported:
- Osteomyelitis
- Extravasation
- Subcutaneous abscess
- Leakage around insertion site
- Difficulty removing device
Q8. How does the EZ-IO compare to CVC/IVC for medication delivery?
Answer and interpretation
Medications administered through the IO are pharmacokinetically equivalent in blood serum concentrations to those administered via the IV route.
The following videos demonstrate how quickly fluids/medication are absorbed once injected into the intraosseous space.
Q9. What ongoing care do intraosseous infusion require?
Answer and interpretation
- Once an IO catheter is inserted, aspirate bone marrow to ensure your in correct space. You can even use this aspirate for pathology testing, then flush the catheter with a 20ml flush to ensure it is patent.
- Flow rates can sometimes be slower related to the anatomy of the intraosseous space and catheter patency, if initially slow repeat 20 ml flush. Application of pressure bags over the fluids can increase flow or use pump/syringe drivers for continuous infusions.
- Securing and protection of the intraosseous catheter can be difficult, but generally device stays in situ by itself without problems.
- Insertion and continuous infusion can caused some localised pain for conscious patients insertion of 2% lignocaine and repeated at regular intervals can minimise this.
- The EZ-IO catheter can only stay in situ for up to 24 hours (manufacturer’s recommendation). The site should be monitored frequently for signs of erythema, swelling or evidence of extravasation. If these are noted, then remove the device immediately.
- Removing the EZ-IO catheter involves disconnecting infusions, attaching a 10 ml luer-lock syringe to the catheter hub, then rotate the catheter clockwise-while pulling straight back, disposing of catheter in bio-hazard container, and apply simple dressing.
References
- Burgert, J. (2009). Intraosseous infusion of blood products and epinephrine in an adult patient in haemorrhagic shock. AANA Journal. PMID: 19911645
- Chatterjee, D. et.al. (2011). Resuscitation in massive obstetric haemorrhage using an intraosseous needle. Anaesthesia. 66, 306-310. PMID: 21401545
- Fenwick, Rob. (2010). Intraosseous approach to vascular access in adult resuscitation. Emergency Nurse. 18(4), 22-25. PMID: 20662405
- Knuth, T. Paxton, J. & Myers, D.(2011). Intraosseous injection of iodinated computed tomography agent in an adult blunt trauma patient. Annals of Emergency Medicine. PMID: 21111513
- Langley, D. Moran, M. (2008). Intraosseous needles: They’re not just for kids anymore. Journal of Emergency Nursing. 34(4), 318-319. PMID: 18640412
- Luck, R. Haines, C. & Mull, C. (2010). Intraosseous Access. The Journal of Emergency Medicine. 39(4), 468-475. PMID: 19545966
- Mac Kinnon, K. (2009). Intraosseous vascular use at signature healthcare Brockton hospital department of emergency services. Journal of Emergency Nursing. 35(5), 425-428. PMID: 19748022
- Ngo, A. et.al. (2009). Intraosseous vascular access in adults using the EZ-IO in an emergency department. International Journal of Emergency Medicine. 2, 155-160. PMID: 20157465
- Ong, M. et.al. (2009). An observational, prospective study comparing tibial and numeral intraosseous access using the EZ-IO. American Journal of Emergency Medicine. 27, 8-15. PMID: 19041528
- Phillips, L. et.al. (2010). Recommendations for the use of intraosseous access for emergency and non-emergent situations in various healthcare settings: A consensus paper. Journal of Emergency Nursing. 36(6), 551-556. PMID: 21030876
- Ruiz-Hornillos, P. et.al. (2011). Systemic fibrinolysis through intraosseous vascular access in ST-segment elevation myocardial infarction. Annals of Emergency Medicine. PMID: 29047209
- Von Hoff, D. et.al. (2008). Does intraosseous equal intravenous? A pharmacokinetic study. American Journal of Emergency Medicine. 26, 31-38. PMID: 18082778

CLINICAL CASES
Resus Room Reflection