Intraosseous access
Reviewed and revised 10 June 2015
OVERVIEW
- Intraosseous (IO) access can be obtained using manual or drill-inserted devices for insertion of specialised needles
- IO access uses the medullary space as a non collapsible entry point into the systemic venous system
- IO access is useful when vascular access is difficult or likely to lead to delayed management in emergency situations
DESCRIPTION
Devices
- Cook or Jamshidi needle
- Drill inserted IO (e.g. EZ-IO)
EZ-IO device and required items
- EZ IO® power driver
- IO needle set:
- 45mm (humerus insertion or excessive tissue),
- 25mm (> 40kg)
- 15mm (3-39kg)
- EZ Connect IV tubing
- 10ml Syringes x 3
- Sterile saline for flush
- 2% lignocaine (without adrenaline) for pain
- Dressings
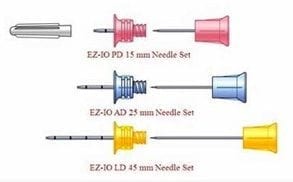
Image used with permission from: www.regval.com
USE
Indications
- Failure to gain intravenous access in a trauma, burns, shock or resuscitation setting
- ILCOR, 2010: “Delivery of drugs via an endotracheal tube is no longer recommended – if IV access cannot be achieved, drugs should be given by the IO route”
- Failure to gain access in a life-threatening situation within a short period of time (e.g. maximum 90 seconds for 2 attempts at paediatric cannulation in APLS)
- Any situation where blood sampling, intravenous access is urgently needed and cannulation is difficult and time-consuming
- A temporising measure to allow stabilisation and facilitation of definitive, long-term intravenous access
Contraindications
- Use on side of definite fractured bones (compartment syndrome risk)
- Use on limbs with possible proximal fractures
- Sites of previous attempts
- Overlying site infection
- osteogenesis imperfecta
- Osteopetrosis (fracture risk)
METHOD OF INSERTION/ USE
Sites of insertion and their landmarks
- Proximal humerus
- Slide thumb up the anterior shaft of the humerus until you feel the greater tubercle, this is the surgical neck
- ~ 1 cm above the surgical neck is the insertion site
- The patient’s hand should rest palm down on the their abdomen with the elbow adducted
- In small children the greater tubercle is poorly developed and may be impalpable
- Proximal tibia
- 2 finger breadths below the patella and 1-2cm medial to the tibial tuberosity in adults
- Distal tibia
- 3 cm proximal to the most prominent aspect of the medial malleolus
- Place one finger directly over the medial malleolus the move ~ 2 cm proximal
- Palpate the anterior and posterior borders of the tibia to ensure that the insertion site is on the flat central aspect of the bone
- Femoral
- anterolateral surface, 3cm above lateral condyle
- iliac crest
- Sternum (this requires a specialised device)
Site and needle selection
- Needle length is determined by the depth of subcutaneous tissue overlying the bone surface, not the size of the patient – one black line (marker 5mm from the hub) should be visible following insertion to ensure that the needle used is of sufficient length
- the proximal humerus is generally the preferred site in a resuscitation scenario as the infusions enter the circulation at the fastest rate through these sites (with the exception of the sternum, which requires a specialised device)
- Fluids given through the proximal humerus reach the central circulation via the superior vena cava, thereby bypassing pelvic and abdominal vasculature. This is important in trauma where there may be abdominal and pelvic injuries resulting extravasation of administered fluid
- In small children (<5 years) the greater tubercle is poorly developed and the proximal humerus landmarks may be difficult to identify. Insertion in the humeral shaft or alternate sites may be preferred
Insertion using EZ-IO
- Explain procedure to patient and obtain consent when appropriate
- Choose appropriate sized needle for insertion site and assemble
- Draw up 10ml sterile saline in syringe and prime the EZ Connect IV tubing
- Locate insertion site (see above)
- Clean site with chlorhexidine wash, and allow to dry
- Connect needle set to driver
- Stabilise site and remove needle cap
- Insert EZ IO needle into selected site with the needle perpendicular to the bone surface until needle tip touches bone
- Confirm that at least one black line is visible, otherwise the needle is too short and larger size should be used
- Penetrate the bone cortex by squeezing the driver’s trigger and applying gentle, consistent, downward pressure
- Release trigger when a sudden “give or pop” is felt upon entry into the medullary space and the desired depth is obtained (a second “pop” suggests penetration of the posterior bone cortex, which with result in extravasation if used)
- Stabilise the catheter hub and remove the driver from the needle
- remove stylet by turning anti-clockwise and dispose of stylet in a sharps container
- Secure the site
- Obtain aspirate for blood sample analysis if required (before connecting primed tubing)
- Connect primed EZ Connect tubing to exposed Luer-lock hub, and flush with 10ml of normal saline. IN a consciosu patient 40mg of 2% lignocaine (maximum 3mg/kg) can be infused slowly prior to flushing to alleviate pain from infusion (infusion is typically more painful than insertion of the IO needle)
- Connect the EZ Connect extension set to primed IV tubing
- Start infusion using a pressure delivery system
- Monitor for complications
- Document time and date of placement
Use
- Once an IO catheter is inserted, aspirate bone marrow to ensure your in correct space. You can even use this aspirate for pathology testing, then flush the catheter with a 20ml flush to ensure it is patent
- Flow rates can sometimes be slower related to the anatomy of the intraosseous space and catheter patency, if initially slow repeat 20 ml flush
- Application of pressure bags (e.g. 300 mmHg) can increase flow or use pump/syringe drivers for continuous infusions
- Securing and protection of the intraosseous catheter can be difficult, but generally device stays in situ by itself without problems
- Insertion and continuous infusion can caused some localised pain for conscious patients insertion of 2% lignocaine and repeated at regular intervals can minimise this
Infusion
- Any medication/fluid that can be infused through a central line can be infused through the IO route
- the IO route and the IV route are pharmacokinetically equivalent (same doses and onset)
- flow rates: sternum > proximal humerus (~80mL/min) > tibia (15 mL/min)
- 1 unit of packed RBCs can be administered via the humeral IO route in about 10 minutes
Removal
- Removal should be performed:
- within 24 hours of insertion
- if there are signs of erythema, swelling or evidence of extravasation.
- Removing the EZ-IO catheter involves disconnecting infusions, attaching a 10 ml luer-lock syringe to the catheter hub, then rotate the catheter clockwise-while pulling straight back, disposing of catheter in bio-hazard container, and apply simple dressing
COMPLICATIONS
- Osteomyelitis (rare)
- Fracture
- Necrosis of epiphyseal plate
- Extravasation
- Compartment syndrome
- Failure
- Injury to others
OTHER INFORMATION
Advantages of intraosseous route over central access in an emergency:
- Quicker (seconds rather than minutes) and easier
- IO compared to femoral/ SVC CVC landmark insertion techniques in medical emergencies (prospective observational study by Lee et al, 2015):
- higher first pass success rate (90% vs. 38%)
- faster (1.2 vs. 10.7 minutes)
- IO compared to femoral/ SVC CVC landmark insertion techniques in medical emergencies (prospective observational study by Lee et al, 2015):
- Cheaper ($100 vs $300)
- Multiple possible insertion sites
- Less training and experience required
- Less complications and risk of catheter related blood stream infections
- Less pain and discomfort during insertion
- the same drugs may be administered
- blood samples can still be obtained for laboratory analysis
Main disadvantages are lack of multiple lumens and capacity for central venous pressure waveform monitoring
Blood transfusion
- administration of blood via the IO route under pressure may result in some degree of haemolysis (clinical significance uncertain)
- some experts use IO to establish immediate access then switch blood administration to the IV route as soon as further access is obtained
LABORATORY ANALYSIS
IO samples show a good correlation with venous samples for:
- Hemoglobin / haematocrit
- Chloride
- Glucose
- Urea
- Creatinine
- Albumin
IO samples poorly correlate with venous samples for:
- WBCs
- Platelets
- Serum CO2
- Sodium
- Potassium
- Calcium
i-STAT® point-of-care analyser (from Resus.ME, 2013)
- Intraosseous aspirates can be tested on an i-STAT® point-of-care analysers
- in some centers this is not allowed due to concerns that IO samples will block the analysers
VIDEOS
Demonstration of EZIO (tibial insertion)
References and Links
Introduction to ICU Series
Introduction to ICU Series Landing Page
DAY TO DAY ICU: FASTHUG, ICU Ward Round, Clinical Examination, Communication in a Crisis, Documenting the ward round in ICU, Human Factors
AIRWAY: Bag Valve Mask Ventilation, Oropharyngeal Airway, Nasopharyngeal Airway, Endotracheal Tube (ETT), Tracheostomy Tubes
BREATHING: Positive End Expiratory Pressure (PEEP), High Flow Nasal Prongs (HFNP), Intubation and Mechanical Ventilation, Mechanical Ventilation Overview, Non-invasive Ventilation (NIV)
CIRCULATION: Arrhythmias, Atrial Fibrillation, ICU after Cardiac Surgery, Pacing Modes, ECMO, Shock
CNS: Brain Death, Delirium in the ICU, Examination of the Unconscious Patient, External-ventricular Drain (EVD), Sedation in the ICU
GASTROINTESTINAL: Enteral Nutrition vs Parenteral Nutrition, Intolerance to EN, Prokinetics, Stress Ulcer Prophylaxis (SUP), Ileus
GENITOURINARY: Acute Kidney Injury (AKI), CRRT Indications
HAEMATOLOGICAL: Anaemia, Blood Products, Massive Transfusion Protocol (MTP)
INFECTIOUS DISEASE: Antimicrobial Stewardship, Antimicrobial Quick Reference, Central Line Associated Bacterial Infection (CLABSI), Handwashing in ICU, Neutropenic Sepsis, Nosocomial Infections, Sepsis Overview
SPECIAL GROUPS IN ICU: Early Management of the Critically Ill Child, Paediatric Formulas, Paediatric Vital Signs, Pregnancy and ICU, Obesity, Elderly
FLUIDS AND ELECTROLYTES: Albumin vs 0.9% Saline, Assessing Fluid Status, Electrolyte Abnormalities, Hypertonic Saline
PHARMACOLOGY: Drug Infusion Doses, Summary of Vasopressors, Prokinetics, Steroid Conversion, GI Drug Absorption in Critical Illness
PROCEDURES: Arterial line, CVC, Intercostal Catheter (ICC), Intraosseous Needle, Underwater seal drain, Naso- and Orogastric Tubes (NGT/OGT), Rapid Infusion Catheter (RIC)
INVESTIGATIONS: ABG Interpretation, Echo in ICU, CXR in ICU, Routine daily CXR, FBC, TEG/ROTEM, US in Critical Care
ICU MONITORING: NIBP vs Arterial line, Arterial Line Pressure Transduction, Cardiac Output, Central Venous Pressure (CVP), CO2 / Capnography, Pulmonary Artery Catheter (PAC / Swan-Ganz), Pulse Oximeter
LITFL
Journal articles
- Dubick MA, Holcomb JB. A review of intraosseous vascular access: current status and military application. Mil Med. 2000;165:(7)552-9. [pubmed]
- Foëx BA. Discovery of the intraosseous route for fluid administration. J Accid Emerg Med. 2000;17:(2)136-7. [pubmed]
- Hoskins SL, do Nascimento P, Lima RM, Espana-Tenorio JM, Kramer GC. Pharmacokinetics of intraosseous and central venous drug delivery during cardiopulmonary resuscitation. Resuscitation. 2012;83:(1)107-12. [pubmed]
- Lee PM, Lee C, Rattner P, Wu X, Gershengorn H, Acquah S. Intraosseous versus central venous catheter utilization and performance during inpatient medical emergencies. Crit Care Med. 2015;43:(6)1233-8. [pubmed]
- Leidel BA, Kirchhoff C, Bogner V, Braunstein V, Biberthaler P, Kanz KG. Comparison of intraosseous versus central venous vascular access in adults under resuscitation in the emergency department with inaccessible peripheral veins. Resuscitation. 2012;83:(1)40-5. [pubmed]
- Luck, R. Haines, C. & Mull, C. (2010). Intraosseous Access. The Journal of Emergency Medicine. 39(4), 468-475. PMID: 19545966
- Ngo, A. et.al. (2009). Intraosseous vascular access in adults using the EZ-IO in an emergency department. International Journal of Emergency Medicine. 2, 155-160. PMID: 20157465
- Philbeck TE, Miller LJ, Montez D, Puga T. Hurts so good. Easing IO pain and pressure. JEMS. 2010;35:(9)58-62, 65-6, 68; quiz 69. [pubmed]
- Rosenberg H, Cheung WJ. Intraosseous access. CMAJ. 2013;185:(5)E238. [pubmed]
- Von Hoff, D. et.al. (2008). Does intraosseous equal intravenous? A pharmacokinetic study. American Journal of Emergency Medicine. 26, 31-38. PMID: 18082778
FOAM and web resources
- Arrow EZ-IO educational resources (no finanical conflicts, just the device I am most familiar with)
- Resus.ME — Point of care analysis of intraosseous samples (2013)
- Resus.ME — i-STAT® analysis of intraosseous aspirate (2014)
- Trauma Professionals Blog — Lab Values From Intraosseous Blood

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
