Seizures, Sedation and Saliva
aka Toxicology Conundrum 052
A 21-year-old male with a background of schizophrenia and previous intentional overdose, weighing 70kg, was brought to the ED via ambulance after having a witnessed seizure at home.
Prior to this, he was witnessed to be drowsy and salivating excessively by his family but was able to admit to taking 2000mg (20 x 100mg) of his own clozapine an hour prior to his witnessed seizure. His family reported that he did not have access to any other medications as he was ‘closely supervised’ at home. After initially found to be drowsy, he subsequently had a generalised tonic-clonic seizure lasting five minutes.
On arrival, paramedics found him to be unresponsive but protecting his airway and sitting up intermittently but non-purposefully. He was tachycardic (130 beats/min) and hypotensive (80mmHg systolic), the latter of which responded to an intravenous fluid bolus of 0.9% saline (1000mL). He had a subsequent seizure en route but this resolved spontaneously.
ECG demonstrated a sinus tachycardia with a manually measured QRS and QT durations of 80 ms and 320 ms respectively.
Questions
Q1. What type of drug is clozapine and what receptors does it act on?
Answer and interpretation
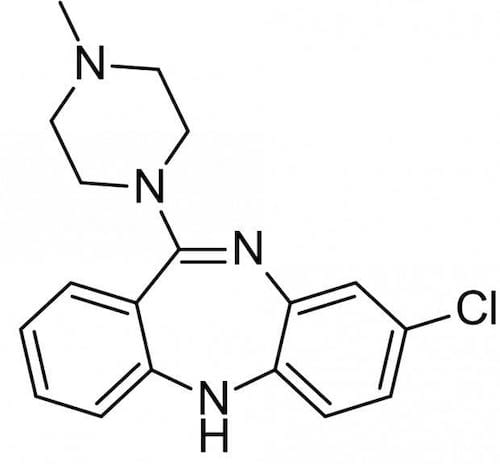
Clozapine is an atypical anti-psychotic agent.
Clozapine is commonly prescribed for treatment-refractory schizophrenia. Given this indication, it is not often used and is usually administered under supervision so overdose with this drug is rare. Clozapine is a tricyclic dibenzodiazepine atypical antipsychotic that acts at multiple receptors with antagonism of D1 and D2 as well as serotonin (5HT2), muscarinic (M1), histaminic (H1), peripheral alpha-adrenoreceptors and gamma-aminobutryic acid (GABA) receptors.
Like other anti-psychotics, the observed action of clozapine at multiple receptors also accounts for the clinical presentation seen in overdose.
Clozapine is available as 25, 50, 100 and 200mg tablets in either packets of 28 or 100 tablets.
Q2. Describe the toxicokinetics of clozapine
Answer and interpretation
Toxicokinetics of clozapine:
- Absorption: Rapidly absorbed following oral administration. Intoxication occurs within 4 hours of ingestion.
- Distribution: Moderate volume of distribution (0.5-3L/kg). Highly protein-bound.
- Metabolism: Metabolised in the lliver by oxidation (cytochrome P450 1A2, 2D6) to its metabolites with significant first pass effect.
- Excretion: Mainly in the urine and faces as metabolites
Q3. What are the clinical features of clozapine overdose?
Answer and interpretation
Clozapine, like many other anti-psychotics, has multiple potential toxicological properties owing to its actions at multiple receptors. Toxicity usually resolves within 24 hours.
Effects include:
CNS effects
- Lethargy, confusion, sedation, coma (the latter requiring intubation is rare)
- Seizures occur in ~5-10% of patients
- Extra-pyramidal side-effects are more common in children
Cardiovascular effects
- Sinus tachycardia, hypotension (due to alpha2-adrenoreceptor blockade)
- QT prolongation is rare
Anti-muscarinic effects
- Agitation, restlessness, delirium, mydriasis (big pupils) but often have miosis (small pupils due to alpha-bloackade), dry, warm skin, tachycardia, ileus, urinary retention (don’t forget an IDC with an agitated patient post overdose with an anticholinergic!)
Hypersalivation is a characteristic and seemingly paradoxical effect of clozapine toxicity. The mechanism is poorly understood and likely multifactorial
Q4. The patient’s family are adamant he could have not taken anything else. The medical student shadowing you asks if that means you don’t need to order a paracetamol level? What is your response?
Answer and interpretation
There are two tests that are incredibly useful in Toxicology (not only my opinion but that of many smarter people too):
- ECG
- paracetamol level
Whilst some patients present to the Emergency Department whilst conscious and clearly volunteer how much and what they have taken, many do not (as in this case). Paracetamol poisoning is often clinically silent initially and, if not treated, can lead to serious morbidity or even mortality. However, it is easily detected via a simple blood test, and has a safe and effective antidote that is widely available. Similarly, the ECG is a cheap, useful non-invasive test useful for identifying otherwise occult cardiotoxicity.
On arrival to the ED, the patient is taken into a resuscitation cubicle. The patient has another episode of hypotension (80/40mmHg) and is given another litre of 0.9% saline. The assist button is pressed thirty minutes later. You race in to find the patient seizing. The seizure is terminated with some midazolam but you notice that the patient is still hypotensive with a blood pressure of 75/40mmHg. What are you going to do?
Q5. What is the risk assessment for this patient?
Answer and interpretation
Whilst clozapine overdose is usually considered to be benign and any accompanying hypotension can be resolved with intravenous fluids alone, this patient has significant hypotension despite adequate filling.
As clozapine is known to act as a peripheral alpha-adrenoreceptor antagonist, commencing an inotrope is suggested. Noradrenaline, an alpha-agonist, is the preferred choice. Alternatives could include other alpha-adrenergic agents such as metaraminol or phenylephrine. In refractory cases, vasopressin has been used with good effect in a previous published case report.
Q6. Whilst the noradrenaline is being hung, your super keen medical student suggests getting an ‘Echo’ because ‘this might be clozapine myocarditis….I read about it once!’. Could it be?
Answer and interpretation
Both agranulocytosis and myocarditis are known complications of chronic therapeutic clozapine use, however they are not features of acute overdose.
An echocardiogram may be appropriate if there were concerns about response to inotropes in the setting of hypotension.
Q7. In general, what is the management of clozapine overdose?
Answer and interpretation
Using the Resus-RSI-DEAD approach as all good toxicologists do…
Resuscitation
- Attention to airway, breathing and circulation always takes precedent. Basic resuscitative measures ensure a good outcome in the vast majority of patients.
- Treat seizures with benzodiazepines
- If intravenous fluid does not improve hypotension, consider the use of an inotrope (noradrenaline is generally preferred)
Supportive care and monitoring
- Supportive care will suffice for most cases so ensure it is done well!
- Secure appropriate IV access
- Ensure adequate hydration with IV fluids
- Remember FASTHUGS IN BED Please especially pressure care, bladder care and DVT prophylaxis
- Cardiac monitoring should continue until toxicity is reversed if ECG changes are present
Investigations
- ECG, paracetamol and blood glucose levels should be performed as recommended for all intentional overdoses
- Consider possible co-ingestants
Decontamination
- Clozapine is rapidly absorbed and usually benign. Activated charcoal is therefore not indicated on these grounds.
Antidotes
- None available
Enhanced elimination
- Not useful
Disposition
- Haemodynamically stable patients that are symptomatic (i.e. drowsy) can be managed as inpatients in an appropriate ward (e.g. observation unit) until medically cleared (awake, able to walk, has passed urine independently and has tolerated oral intake)
- Patients requiring inotropic support require HDU/ICU but this is likely to be for a short period of time (~24 hours)
- Psychiatric review and possible inpatient management
References
- Burns MJ. The pharmacology and toxicology of atypical antipsychotic agents. J Toxicol Clin Toxicol. 2001;39(1):1-14. [PMID 11327216.]
- Rotella JA, Zarei F, Frauman AG, Greene SL. Refractory hypotension treated with vasopressin after intentional clozapine overdose. Eur J Emerg Med. 2014 Aug;21(4):319-20 [PMID 24983646]

CLINICAL CASES
Toxicology Conundrum
FACEM Clinical Toxicology Fellow and Emergency Medicine Physician at Austin Health, Melbourne | LinkedIn |
