Trauma! Chest Injuries I
aka Trauma Tribulation 017
A trauma call went out after a 24-year-old man was brought to the ED following an assault. He was set upon by a gang of youths reportedly wielding baseball bats and knives.
You are performing the primary survey as part of his initial assessment, hopefully you won’t miss any important chest injuries… Furthermore, hopefully you’ll know how to treat them.
Questions
Q1. What immediately life-threatening chest injuries should be considered during the primary survey of major trauma patients?
Answer and interpretation
A widely used mnemonic for the 6 killer conditions to think of, and actively search for, during the primary survey is ATOM-FC:
- Airway obstruction or disruption
- Tension pneumothorax
- Open pneumothorax
- Massive haemothorax
- Flail chest
- Cardiac tamponade
Q2. Describe ow you would recognize and manage major airway obstruction or disruption
Answer and interpretation
Recognition
- External neck deformity or hematoma, crepitus from laryngeal fracture, surgical emphysema, hoarse voice or gurgling
- Complete airway obstruction — silent chest, paradoxical chest movements
- Partial airway obstruction — stridor, respiratory distress
- Cyanosis
Management
- High flow oxygen 15 L/min via non-rebreather mask
- Use airway maneuvers and adjuncts to attempt to achieve airway patency (jaw-thrust, suction, oropharyngeal airway) and rapidly proceed to definitive airway if airway disruption confirmed
- Surgical airway may be required as endotracheal intubation with direct laryngoscopy may not be possible due to distorted anatomy
- If a disrupted airway is visible through an open neck wound attempt to secure the distal trachea with forceps (retraction) and intubate through the wound (consider using a bougie)
- Will need bronchoscopy / thoracotomy
Q3. Describe how you would recognize and manage a tension pneumothorax
Answer and interpretation
Simple pneumothorax converts to a tension pneumothorax if the lung defect acts as a one way valve, which allows ongoing air leak into pleural space without letting it leak back out. The condition can be rapidly fatal as intra-thoracic pressure rises cause decreased venous return and kinking of great vessels resulting in obstructive shock.
Recognition
- Anxiety and agitation
- Respiratory distress
- Tachycardia, hypotension
- Neck vein distension
- Ipsilateral hyperexpansion and decreased chest movement
- Tracheal deviation to the contra-lateral side
- Hyper-resonance ipsilaterally
- Decreased breath sounds ipsilaterally
- Bedside ultrasound can rapidly confirm pneumothorax
Management
- High flow oxygen 15L/min via non-rebreather
- Immediate needle thoracocentesis or finger thoracostomy (‘decompression’).
- Proceed to formal intercostal catheter after needle decompression
Have a high index of suspicion in any tachycardic and hypotensive patient — clinical features may not be obvious!
Should you use a needle or a knife for immediate decompression of a tension pneumothorax? Learn more:
- Check out the discussion on EMCrit: Needle versus Knife II: Needle vs. Finger Thoracostomy.
- Resus.ME — Inadequate pre-hospital needle thoracostomy
Q4. Describe how you would recognize and manage an open pneumothorax
Answer and interpretation
Open pneumothorax is essentially a ‘sucking chest wound’. It is thought that once a chest wound is >2/3rds the diameter of the trachea, air will enter wound preferentially.
Recognition
- Open wound on chest wall
- Anxiety and agitation
- Respiratory distress
- Tachycardia
- Decreased chest movement ipsilaterally
- Hyper-resonance ipsilaterally
- Decreased breath sounds ipsilaterally
- Bedside ultrasound can rapidly confirm pneumothorax
Management
- High flow oxygen 15L/min via non-rebreather
- Cover with occlusive 3-sided dressing to form a ‘flutter valve’ that allows the egress of air through the wound but prevents ‘sucking in’.
- Place formal catheter in separate intercostal space
- Will need formal exploration prior to closing
Q5. Describe how you would recognize and manage a massive haemothorax
Answer and interpretation
Massive haemothorax can result from either blunt or penetrating trauma. The source of bleeding can be from the lungs, major vessels, intercostal vessels or even the heart.
Massive hemothorax is defined by the need for thoracotomy — the indications are:
- Blood loss > 1,500 mL or 1/3rd of blood volume
- Blood loss >200 mL/h (3 mL/kg/h) for 2-4 hours
Recognition
- Anxiety and agitation
- Hemorrhagic shock — pallor, tachycardia, hypotension, cool peripheries
- External evidence of thoracic injury
- Decreased chest movement ipsilaterally
- Ipsilateral dullness
- Decreased breath sounds ipsilaterally
- Persistent blood loss following intercostal catheter insertion
- Bedside ultrasound can rapidly confirm the presence of pleural fluid
Management
- High flow oxygen 15L/min via non-rebreather
- Treat with rapid restoration of blood volume combined with concurrent drainage of thorax
- Immediate intercostal catheter insertion (re-expanding lung may tamponade the bleeding vessels)
- Hemostatic resuscitation — activate massive transfusion protocol, use of an autotransfuser is ideal
- Thoracotomy
Q6. Describe how you wound perform needle thoracocentesis in a major trauma patient.
Answer and interpretation
Videos are worth a million words… Michael McGonigal from The Trauma Professional’s blog gives the answer:
But, hang on a sec… perhaps we shouldn’t be using that needle after all… Listen to Scott Weingart’s take on this in the EMCrit podcast Needle versus Knife II: Needle vs. Finger Thoracostomy.
Q7. Describe how you would insert an intercostal catheter in a major trauma patient.
Answer and interpretation
Here’s another great video from Michael McGonigal:
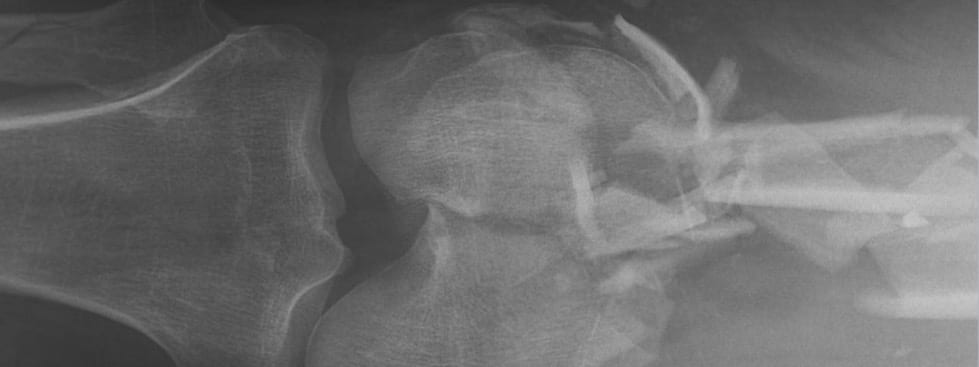
Q8. Describe how you would recognize and manage a flail chest
Answer and interpretation
A flail chest is defined as fractures of 2 or more ribs in 2 or more locations. This results in a segment of the chest wall that is no longer in continuity with the rest of the thoracic cage. Paradoxical movement results, the segment moves inwards on inspiration as the rest of the chest expands and outwards on expiration as the rest of the chest deflates.
Recognition
- Chest pain
- Respiratory distress
- Boney crepitus
- Paradoxical chest wall movements of the affected segment (not apparent if positive pressure ventilation applied)
Management
- High flow oxygen 15L/min via non-rebreather
- Analgesia — paracetamol 1g qid po, NSAIDs if not contraindicated, titrated opiates IV (e.g. fentanyl 25 micrograms q5min prn IV). Early use of regional anesthesia (intercostal nerve blocks, paravertebral block, epidural anesthesia) due to risk of respiratory depression.
- Respiratory monitoring and support — close monitoring of SaO2, respiratory effort, and ABGs is important as patients tend to gradually deteriorate and may require intubation and mechanical ventilation.
Q9. Describe how you would recognize and manage cardiac tamponade
Answer and interpretation
Pericardial tamponade is more common in penetrating thoracic trauma than blunt trauma. As little as 75 mL of blood accumulating in the pericardial space acutely can impair cardiac filling, resulting in tamponade and obstructive shock.
Recognition
- Anxiety and agitation
- Obstructive shock — tachycardia, hypotension, cool peripheries
- Beck’s triad: muffled heart sounds, hypotension and distended neck veins — not especially in a noisy trauma bay!
- Pulsus paradoxus (drop in systolic blood pressure >10 mmHg on inspiration)
- Very hard to differentiate clinically from tension pneumothorax and needs to be actively sought
- Mostly diagnosed following identification of a pericardial effusion on bedside ultrasound as part of the FAST exam ((see hemopericardium at ultrasoundvillage.com)
Management
- High flow oxygen 15L/min via non-rebreather
- May transiently respond to fluid challenge
- Needle pericardiocentesis, preferably ultrasound guided, may be life-saving but may fail due to clotted blood
- Pericardotomy is definitive treatment
References
- Own the Airway – LITFL
- Own the Chest Tube – LITFL
CLINICAL CASES
Trauma Tribulation
