Trauma! Spinal Injury
aka Trauma Tribulation 016
A 24 year old woman is brought into a trauma bay in your emergency department after a fall from a horse. She has a hard collar on and her head is taped to the hard spine board she rode in on. It is immediately apparent that although she is GCS 15, she is unable to move any of her limbs.
Are you up to the task of assessing and managing spinal trauma in the emergency department?
Questions
Q1. Which major trauma patients should have c-spine precautions?
Answer and interpretation
Those with:
- Neck pain or neurological symptoms
- Altered level of consciousness
- Significant blunt injury above the level of the clavicles
As always, what is considered ‘significant’ is contentious. Nevertheless, it is worth noting that 10% of major head injuries will have a concurrent spinal injury.
Q2. How is the cervical spine immobilized?
Answer and interpretation
A hard collar is applied, but by itself this inadequately immobilizes the cervical spine.
The main purpose of a cervical spine collar is to remind healthcare workers that the neck has not yet been cleared.
Adequate immobilisation requires the addition of either:
- Manual immobilization
- Application of sand bags and head tape
Appropriate cervical spine precautions is an evolving area of controversy…
- Resus.ME — Another reason to be skeptical about collars
- Resus.ME — Cervical spine guideline
- Resus.ME — Neck movement in spite of collar
The patient says she feels nauseated and is worried she might vomit.
Q3. What should you do if a patient in cervical spine precautions starts to vomit?
Answer and interpretation
Immediate intervention is needed:
- Log roll if 4 people are available — one to hold the head, and three to perform the roll
- If insufficient numbers of people are available, tilt the bed head down so that vomit runs clear of the airway
- Suction away the vomitus with a Yankauer
Further intervention:
- Administer antiemetics (e.g. ondansetron 4mg IV)
- Seek and treat underlying causes — patients often vomit due to pain or opioid analgesia, but it can also be a sign of worrying causes such as serious abdominal trauma, hypotension or raised intracranial pressure
Q4. What is the difference between primary and secondary spinal cord injury?
Answer and interpretation
Primary spinal cord injury results from blunt or penetrating mechanisms at the time of the initial traumatic event. Fractures, dislocations, hematomas and soft tissue swelling directly injury the spinal cord via mass effect, disrupted blood supply or transection.
Secondary spinal cord injury occurs after primary spinal cord injury due to mechanical instability contributing to ongoing direct injury, or insults from other factors such as hypoxia and hypoperfusion. The later may be due to associated injuries in a multiply injured patient or due to spinal cord injury associated respiratory insufficiency and neurogenic shock.
Much of the acute management of spinal cord injury is aimed at preventing secondary spinal cord injury.
You notice that the patient is now mildly tachypnoeic with shallow breaths and a weak cough.
Q5. How do patients with spinal injuries develop respiratory insufficiency?
Answer and interpretation
The mechanism of respiratory insufficiency varies according to the level of injury:
- High cervical injuries may lead to airway obstruction due to local hematoma and swelling.
- Lesions at the C5 level or higher lead to diaphragmatic paresis or paralysis, as the phrenic nerve arises from the C3-5 levels.
- Thoracic or higher lesions may lead to respiratory distress due to paralysis of intercostal muscles, as the intercostal nerves arise from the T1-12 levels.
Other causes include:
- Coexistent thoracic injuries
- Coexistent traumatic brain injury (e.g. decreased respiratory drive from coma)
- Complications of spinal cord injury (e.g. aspiration, atelectasis, pulmonary embolus, metabolic acidosis from spinal shock)
- Complications of treatment (e.g. sedation, fluid overload, transfusion- associated acute lung injury, ventilator associated pneumonia).
Observe spinal injury patients closely for evidence of respiratory insufficiency — early signs include mild tachypnea with shallow breaths and a weakening cough.
The patient’s vital signs are rechecked. She has a blood pressure of 80/50 mmHg.
Q6. What is the most likely cause of hypotension in a major trauma patient with a possible spinal cord injury?
Answer and interpretation
Haemorrhage
Any hypotension in a trauma patient should be assumed to be hypovolaemic in origin until proven otherwise, even in a patient with an overt spinal injury. Sources of bleeding must be aggressively sought and controlled. Neurogenic shock is rare in comparison.
No source of bleeding can be found on physical examination or on the extended FAST scan performed at the bedside. Her heart rate is only 50/min. The medical student attached to your team asks if this means the patient has spinal shock.
Q7. What is the difference between neurogenic shock and spinal shock?
Answer and interpretation
These are often confused — even esteemed textbooks such as Dunn’s ‘The Emergency Medicine Manual’ can get it wrong (see page 1160 in the hard bound 5th edition — but corrected in the online edition (see Bob Dunn’s comment below)…
Neurogenic shock is classically characterised by hypotension, bradycardia and peripheral vasodilatation. Neurogenic shock is due to loss of sympathetic vascular tone and happens only after a significant proportion of the sympathetic nervous system has been damaged – as may occur with lesions at the T6 level or higher.
The patient’s vital signs are consistent with neurogenic shock.
Spinal shock is not a true form of shock. It refers to the flaccid areflexia that may occur after spinal cord injury, and may last hours to weeks. It may be thought of as ‘concussion’ of the spinal cord and resolves as soft tissue swelling improves. Priapism may be present.
Q8. Describe your overall approach to the management of a patient with spinal cord injury.
Answer and interpretation
- Activate the trauma team and use a coordinated team-based approach in a dedicated trauma bay appropriately staffed and equipped for resuscitation.
- Remove the patient from a rigid spine board as soon as possible by transferring onto a trauma bed
- Primary survey and resuscitation (ABCDE approach)
- Airway maintenance with cervical spine immobilization
— lesions above C5 require intubation for mechanical ventilation
— maintain cervical spine precautions (hard collar, sandbags, tape forehead) - Breathing and ventilation
— high flow oxygen 15L/min via a non-rebreather mask
— monitor for respiratory insufficiency from thoracic or higher spinal lesions, complications of spinal cord injury, or other thoracic injuries - Circulation with haemorrhage control
— look for neurogenic shock, which may also mask hemorrhagic shock (which is more common)
— treat neurogenic shock with repeated fluid boluses (e.g. 250 mL crystalloid) +/- noradrenaline infusion to maintain organ perfusion (normal mentation, warm peripheries, urine output >0.5 mL/kg/h) an/or a MAP >65 mmHg.
— be aware that vagal stimuli (e.g. suction, NGT insertion, intubation) may exacerbate neurogenic shock; treat with atropine 0.6mg IV boluses. - Disability (neurological evaluation)
— detailed neurological exam including motor and sensory levels bilaterally; check for priapism; check anal sphincter tone and bulbocavernosus reflex. - Exposure and Environmental Control
— higher risk of hypothermia due to peripheral vasodilation resulting from sympatholysis and decreased muscular activity
— use fluid warmer, warm blankets, and/or bair hugger to keep patietn warm - Adjuncts to Primary Survey and Resuscitation
— ECG and full non-invasive monitoring including temperature
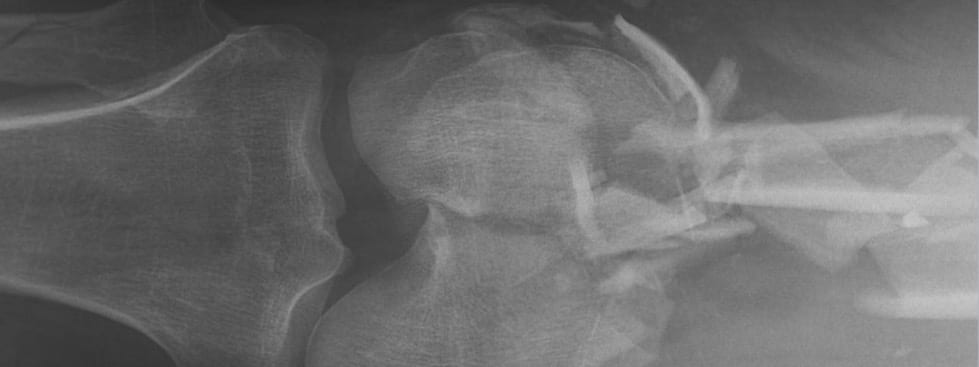
— Obtain trauma series radiographs (lateral cervical spine XR, chest XR, pelvic XR)
— Bedside ultrasound to identify other injuries and sources of haemorrhage (e.g. EFAST)
— Nasogastric tube insertion — spinal patients are at risk of gastric distention
— Indwelling catheter insertion — prevent urinary retention and bladder overdistention due to spinal inury; monitor urine output given the risk of hemorrhagic and neurogenic shock. - Consider transfer
— Organize early transfer to a spinal unit - Secondary survey
— Head-to-toe examination looking for other injuries - Adjuncts to Secondary Survey
— Organize imaging to define the nature of the spinal cord injury (CT is more readily available and defines boney injuries; MRI defines neurological injury)
— Monitor for fluid overload using bedside ultrasound (look for IVC distention and pulmonary edema) and/ or CVP monitoring. - Continued post-resuscitation care and monitoring
— Remember FASTHUGS IN BED Please! - Definitive care and disposition
— Transfer to spinal unit for ongoing care.
Q9. How is spinal cord injury classified and how the level of spinal injury determined?
Answer and interpretation
Use the American Spinal Injury Association (ASIA) classification to avoid confusion.
The ASIA classification is based on:
- The neurological level — the most caudal segment with normal function
- Severity of the neurological deficit — graded A to E on the ASIA Impairment scale (A is complete, E is normal) based on degree of intact motor and sensory function.
Use this chart to determine the ASIA classification for your patients.
Spinal cord injury patients require careful examination and documentation of the level initially, and this should be performed serially. This allows early detection of injury progression or of resolution of spinal shock (bulbocavernosus reflex typically returns after about 48 hours unless there is a complete spinal cord injury).
Q10. How are the thoracic and lumbar spine cleared in major trauma?
Answer and interpretation
There are no validated decisions rules for clearing the thoracic or lumbar spine.
Imaging is generally required if there are the following:
- Point tenderness
- Deformity or bony step
- Neurological findings consistent with a thoracic or lumbar injury
- High risk mechanism, especially in the presence of distracting injuries
If pain is the only symptom, I generally take into account patient factors (e.g. age) and suspicion based on mechanism. If I have a low degree of suspicion of significant injury I will provide analgesia and re-examine after a period of observation. Often the patient’s symptoms resolve and specific imaging is unnecessary. Avoid using this approach in the presence of distracting injuries or an altered mental state.
Note that significant thoracolumbar spinal injury can be present in the absence of midline tenderness.
References
- Young, W. Spinal Cord Injury Levels & Classification, SCI-INFO-PAGES, 2010.
CLINICAL CASES
Trauma Tribulation

Thank you for the nice explanations. My question is as it is universal patients in our trauma bay, on initial stabilisation, we need to avoid organ and organ systems secondary insults like hypoxia, hypotension, hypo or hyperthermia,…
As long as hypotension is concerned the current recommendation in any trauma patient (except TBI and TSCI) is permissive hypotension to prevent the deadly triads, the continuum of which will be damage control surgery.
The target MAP in both TBI and TSCI as end goal directed therapy is 80mmHg or above so as to avoid secondary insults in hospital. This is how we do it in our case!
Any evidence for MAP target of 65mmHg when treating spinal cord injury patients?
Thank you!