William H. Park
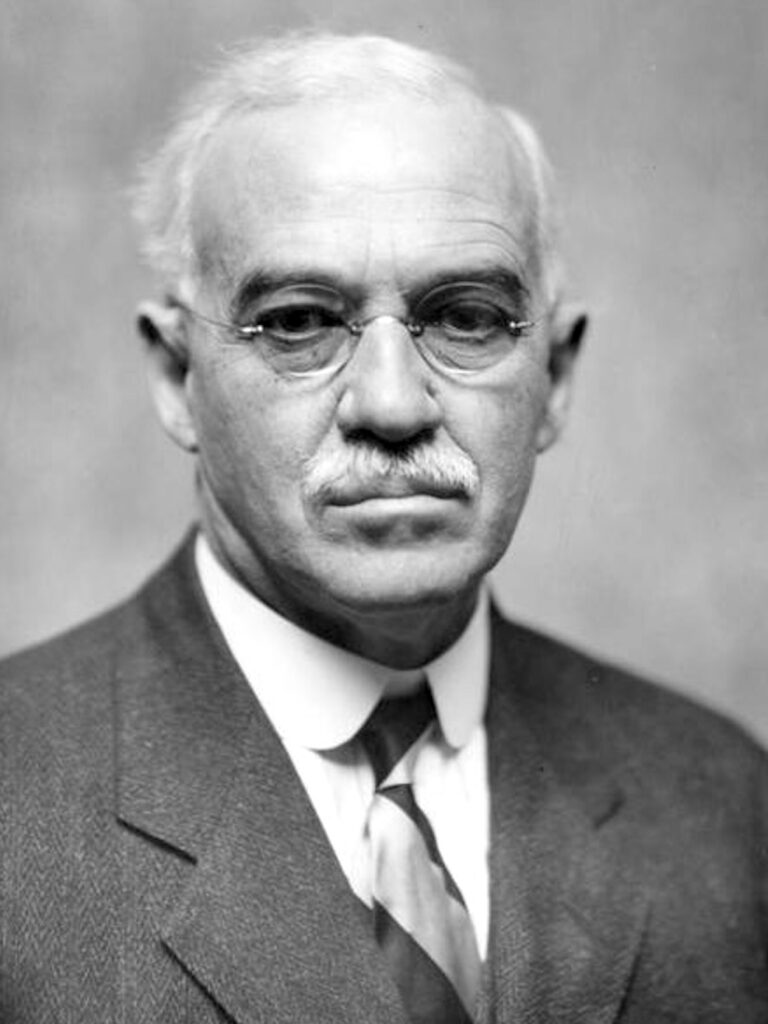
William Hallock Park (1863–1939) was an American Immunologist.
Park was a public health leader whose laboratory work shaped the control of diphtheria, typhoid, and other infectious diseases in the early 20th century. As director of the New York City Department of Health Laboratories for over three decades, Park oversaw a system that became a global model for municipal public health laboratories. His collaborations with Anna Wessels Williams yielded the Park–Williams bacillus (PW8) strain, which enabled large-scale production of diphtheria antitoxin and saved countless children’s lives.
Park’s research extended from bacteriological methods to infant nutrition, milk pasteurisation, and immunisation. He co-developed the Park–Williams fixative, championed pure milk in infant feeding, and designed simple diagnostic tests for diphtheria and typhoid. His commitment to making laboratory medicine practical and reproducible transformed the fight against communicable disease in crowded urban settings like New York City.
He also became a central figure in one of medicine’s most famous public health controversies: the case of “Typhoid Mary” (Mary Mallon). Park’s cultures confirmed her as a chronic, asymptomatic typhoid carrier, framing the unprecedented ethical question of whether society could restrict one person’s liberty to protect the public. In stating “Has the city a right to deprive her of her liberty for perhaps her whole life?”, Park anticipated modern debates over quarantine, carriers, and the balance between individual rights and collective safety.
Biographical Timeline
- Born on December 30, 1863 in New York City
- 1883 – Graduated BA, City College of New York.
- 1886 – MD from the Columbia University College of Physicians and Surgeons. Internship at Roosevelt Hospital, New York City
- 1887–1889 – Post-graduate studies in Vienna, Austria.
- 1890 – Returned to the US, began work on diphtheria bacteriology with Theophil Mitchell Prudden (1849-1924).
- 1893 – Appointed Director, New York City Board of Health Laboratories of Pathology, Bacteriology, and Disinfection. Founded the first municipal bacteriological diagnostic laboratory in the United States.
- 1894 – Following Roux and von Behring’s diphtheria antitoxin discovery, initiated horse inoculation program in NYC. Collaborated with Anna Wessels Williams, who isolated the “Park No. 8 strain” of C. diphtheriae used worldwide in antitoxin production.
- 1897–1933 – Professor of Bacteriology, New York University and Medical College.
- 1905 – Co-authored Pathogenic Microorganisms (with Anna W. Williams), widely adopted textbook, eventually reaching 10 editions.
- 1910s–1920s – Research expanded beyond diphtheria to scarlet fever, tuberculosis, pneumonia, pertussis, meningitis, polio, measles, and infantile diarrhoea. Advocated pasteurisation of milk with Emmett Holt, leading to near elimination of summer infantile diarrhoea in New York.
- 1932 – Awarded Public Welfare Medal, National Academy of Sciences.
- 1933 – Received Townsend Harris Medal, City College of New York. Became Hermann M. Biggs Professor of Preventive Medicine.
- 1936 – Retired as Director, NYC Public Health Research Laboratories. The labs were renamed the William Hallock Park Laboratory.
- Died April 6, 1939 in New York City, age 75 eulogized as the “American Pasteur” and one of the foremost pioneers of public health bacteriology.
Medical Eponyms
Park–Williams Bacillus (PW8 strain, 1894)
In 1894, Anna Wessels Williams isolated a particularly virulent strain of Corynebacterium diphtheriae from a mild case of tonsillar diphtheria. Known as the Park–Williams strain no. 8 (PW8), it proved crucial for the large-scale manufacture of diphtheria antitoxin.
A culture of the diphtheria bacillus, isolated by Dr. A. W. Williams, proved to be especially virulent, and the antitoxic serum prepared from it possessed a high degree of neutralizing power.
Park and Williams, 1896
Prior to PW8, existing strains yielded only limited toxin, restricting antitoxin output. Park and colleagues used PW8 to prepare highly potent serum, which became the international standard strain for diphtheria antitoxin production. By the early 20th century, its use was credited with saving hundreds of thousands of children’s lives worldwide.
Park–Williams Fixative (1890s)
Williams and Park also introduced a fixative solution for preserving bacterial smears in municipal public health laboratories. The fixative stabilized the structural elements of microorganisms, preventing distortion and allowing for permanent, reliable preparations.
This method quickly became standard practice in diagnostic bacteriology, enabling uniform microscopic teaching slides and routine public health surveillance at a time when laboratory bacteriology was still developing as a field.
Park–Holt Pasteurised Milk (1903)
At the turn of the 20th century, infantile diarrhea was a leading cause of child mortality in New York City. As director of the NY Board of Health Laboratory, William H. Park collaborated with paediatrician Luther Emmett Holt (1855-1924) to establish milk stations across the city, distributing pasteurized milk to poor families.
The project, often referred to as the “milk depots,” dramatically reduced infant deaths by controlling bacterial contamination in milk, which was a major vector for E. coli, Salmonella, and other pathogens.
The results obtained with pasteurized milk were most favorable. The mortality among infants fed on it was less than one-third of that among those fed on raw or ordinary milk, and the general health of the children was much better. The evidence from these investigations indicates that the use of pasteurized milk in tenement-houses and institutions of New York City has been followed by a marked diminution in the prevalence and fatality of infantile diarrheal disease.
Park and Holt, 1903
Park’s laboratory verified the bacteriological safety of distributed milk, and by 1911, infant mortality rates in areas served by the milk stations had fallen significantly. This public health intervention became a global model, linking bacteriology, paediatrics, and social reform.
Key Medical Contributions
Mary Mallon (“Typhoid Mary”)
William H. Park was central to the medical confirmation of Mary Mallon (“Typhoid Mary”), the first recognized healthy carrier of Salmonella typhi in the United States.
In 1907, sanitary engineer George Albert Soper II (1870-1948) traced multiple typhoid outbreaks to a cook, Mary Mallon, and sought bacteriological proof from Park at the New York City Department of Health. Soper determined that since 1899 Mallon had been employed in eight families and in seven of these typhoid fever had broken out within a few weeks or months of her arrival. In all twenty-six cases and one death occurred.
I wanted to have her [Mary Mallon] excretions examined by Dr. William H. Park at the Department’s Research Laboratory. I called Mary a living culture tube and chronic typhoid germ producer. I said she was a proved menace to the community. It was impossible to deal with her in a reasonable and peaceful way, and if the Department meant to examine her, it must be prepared to use force and plenty of it.
Soper 1939
On March 20, 1907, Mallon’s samples were brought to Park’s laboratory. His repeated cultures demonstrated massive and persistent excretion of viable typhoid bacilli:
Bacteriological examination revealed the fact that fully 30 per cent of all the bacteria voided with the feces were typhoid bacilli. The urine was negative… The repeated outbreaks occurring after her entrance in families were in themselves proof that the virulence of the bacilli had remained intact
Park 1908
Park recognized the public health dilemma posed by chronic carriers:
The case of this woman brings up many interesting problems. Has the city a right to deprive her of her liberty for perhaps her whole life? The alternative is to turn loose on the public a woman, who is known to have infected at least twenty-eight persons.
Park 1908
This episode firmly established the concept of healthy carriers in infectious disease epidemiology. Park extended his work beyond typhoid to diphtheria, helping define carrier states as a major reservoir for transmission.
Major Publications
- Park WH. Antitoxin. I. The Production of Diphtheria Toxin. J Comp Med Vet Arch. 1895 Apr;16(4):228-229.
- Medical record 1896; 49:
- Park WH, Williams AW. The production of diphtheria toxin. The journal of experimental medicine 1896; 1(1) [Park-Williams bacillus]
- Park WH, Holt LE. Report upon the results with different kinds of pure and impure milk in infant feeding in tenement-houses and institutions of New York City. Medical News, New York 1903; 83: 1066-1078
- Park WH, Williams AW. Pathogenic micro-organisms. 1905 [2e 1910] [11 editions by 1939]
- Park WH. Typhoid bacilli carriers. JAMA 1908; LI(12): 981-982. [Typhoid Mary]
- Park WH, Krumwiede C. The relative importance of the bovine and human types of tubercle bacilli in the different forms of human tuberculosis. J Med Res 1910; 18: 205-368.
- Park WH. Health laboratory organization. JAMA. 1916; LXVII(27): 2013-2015
- Park WH, Williams AW. Who’s who among the microbes. 1929
References
Biography
- William Hallock Park. Am J Public Health Nations Health. 1939 May;29(5):530-1
- Zinsser H. William Hallock Park 1863-1939. J Bacteriol. 1939 Jul;38(1):v.3-3.
- Ramon G. William Hallock Park: an Eminent Microbiologist and a Great American Public Health Officer (1863–1939). The Journal of Immunology, 1939; 37(3): 179–183
- Oliver WW. The man who lived for tomorrow. A Biography of William Hallock Park, M.D. 1941
- Schaeffer M. William H. Park (1863-1939): his laboratory and his legacy. Am J Public Health. 1985 Nov;75(11):1296-302
- William H. Park, M.D. American Association of Immunologists
Eponymous terms
- McCleary GF. The Infants’ Milk Depot: its History and Function. 1904
- Soper GA. The curious career of Typhoid Mary. Bull NY Acad Med 1939; 15: 698-712.
Eponym
the person behind the name
MBBS, BSc (hons) Global and Public Health, Queen Mary University of London. Currently working as a Resident Medical Officer in Sir Charles Gairdner Hospital, Australia. Interests in Radiology, medical education and global public health.
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

