William Macewen
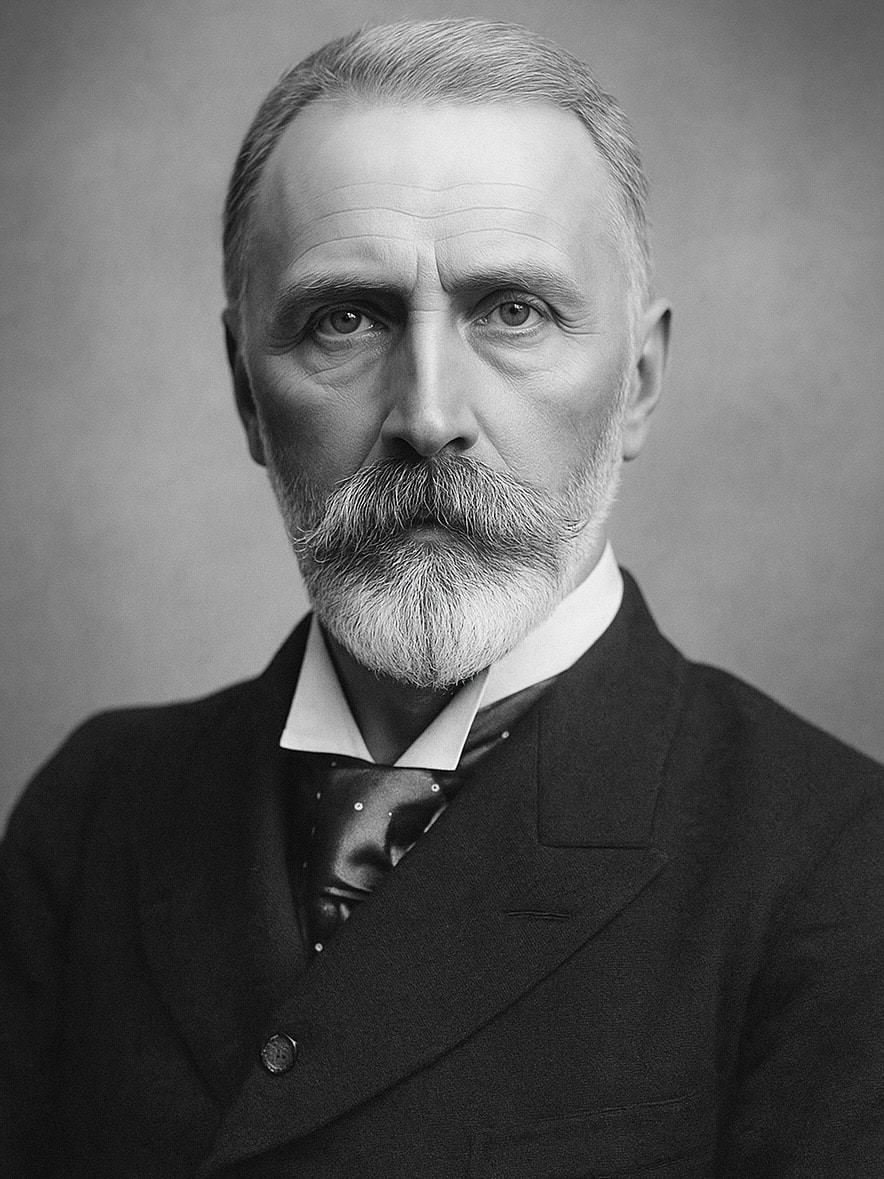
Sir William Macewen (1848–1924) was a Scottish surgeon
Scottish surgeon and pioneer of modern neurosurgery, Sir William Macewen was born 22 June 1848 near Port Bannatyne, Isle of Bute. He studied medicine at the University of Glasgow, graduating MD in 1872, and began his surgical training influenced deeply by Joseph Lister (1827–1912), whose antiseptic techniques revolutionized surgical practice.
By applying rigorous antiseptic methods, Macewen developed an international reputation for innovation and precision. He performed one of the earliest successful brain tumour operations in 1879, and was the first to relieve subdural haemorrhage surgically (1879). He contributed foundational advances in neurosurgery, bone grafting, hernia repair, and pulmonary surgery.
Macewen emphasised localisation in cerebral pathology and used symptoms of agnosia to plan landmark brain operations on the angular gyrus—decades ahead of widespread acceptance. His 1887 observations on pupillary changes in raised intracranial pressure helped establish neurological indicators that remain essential to this day.
He was appointed Surgeon to the Queen in Scotland, knighted in 1902, made Companion of the Bath (CB) in 1917, and given the Freedom of Rothesay in 1922. Sir William Macewen died in Glasgow on 22 March 1924, aged 75.
Biography
- Born June 22, 1848 near Port Bannatyne, Isle of Bute, Scotland
- 1872 – Graduated MD from the University of Glasgow
- 1874 – Fellowship of the Faculty (later the Royal College) of Physicians and Surgeons of Glasgow
- 1875 – Began surgical career at Glasgow Royal Infirmary; lecturer in Clinical Surgery (1881); Professor (1889)
- 1878 – (July 5) – Performed the first documented oral endotracheal intubation for anaesthesia
- 1879 – (July 27) First operation to remove brain tumour (left frontal meningioma)
- 1879 – First surgical relief of subdural haemorrhage
- 1880s – Developed bone grafting techniques and early osteotomy procedures
- 1887 – Described pupillary dilation in raised intracranial pressure (Macewen’s sign)
- 1892 – Appointed Surgeon to the Queen in Scotland
- 1895 – Fellow of the Royal Society (London)
- 1902 – Knight Bachelor (K.B.) for his services to surgery
- 1917 – Made Companion of the Order of the Bath (CB)
- 1922 – Awarded Freedom of Rothesay
- Died March 22, 1924 in Glasgow
Medical Eponyms
Macewen’s Sign (1893)
A clinical sign in which a resonant, hollow “cracked pot” percussion note is elicited over the skull in infants and children with raised intracranial pressure—most commonly from hydrocephalus or cerebral abscess.
Technique: Percuss the skull at the pterion (junction of frontal, parietal, temporal, and sphenoid bones). The note is best elicited when the child is upright, using gentle digital percussion or a plexor.
Historical Context
- Described by Macewen in Elicitation of a differential cranial percussion note (1893), following nearly a decade of systematic observation.
- Macewen did not use the term “cracked-pot” for this finding. Instead, he spoke of a differential cranial percussion note, dependent on skull thickness and intracranial fluid distribution.
- The sound was found to vary with head position and was most distinct when the lateral ventricles were distended.
Clinical Utility: Aids in diagnosing hydrocephalus and ventricular enlargement in children. In Macewen’s series, the sign was particularly helpful in detecting cerebellar abscesses causing secondary ventricular dilatation.
Clarifying the Confusion
- In 1898, Dr. Norman Bruce Carson (St. Louis) published a paper in Annals of Surgery titled “The Cranial ‘Cracked-Pot’ Sound as a Symptom of Cerebellar Tumors”.
- Carson described similar auscultatory findings in children with posterior fossa tumours, attributing the sound to suture separation from internal pressure.
- Carson’s terminology likely led to later conflation of Macewen’s diagnostic resonance with the traumatic “cracked-pot” sound of skull fracture.
Summary
- Macewen’s sign reflects a non-traumatic, pressure-induced resonance aiding diagnosis of intracranial fluid shifts.
- The “cracked-pot” descriptor became popularised post hoc, but is not faithful to Macewen’s original language or intent.
- This sign remains an insightful, albeit historical, bedside test for paediatric raised ICP.
Macewen’s Osteotomy and Bevelled Osteotome (1879)
Between 1875 and 1880, Sir William Macewen developed a groundbreaking method for subcutaneous osteotomy to correct skeletal deformities—especially those resulting from rickets, a widespread condition among urban working-class children.
In 1879, Macewen introduced a uniquely designed osteotome, a chisel-shaped bone-cutting instrument, bevelled on both sides, enabling precise cuts through bone without producing bone dust or comminution. This innovation drastically reduced trauma and the risk of postoperative infection compared to traditional wedge resections.
The chisel is used for paring, shaving, and cutting wedges of bone out, such as removing a cuniform portion from the tibia in anterior curvature. The osteotome is used only for making simple incisions, or wedge-shaped openings without removal of bone.
The osteotome is an instrument of the chisel order, bevelled on both sides, so as to resemble a very slender wedge. The handle and the blade form one piece. The handle is octagonal, which is preferable to the oval or cylindrical, as it affords a better grip, and enables the operator to readily detect any deviation winch the instrument might assume while in the wound.
Named the osteotome…to employ a single word which would at once distinguish it from the ordinary chisel, and at the same time be more euphemistic to a patient’s ear, it has been termed an osteotome.
Macewen’s technique involved making subperiosteal cuts to realign bones without exposing large bone surfaces, preserving periosteal integrity and enhancing healing. His technique provided effective treatment for genu valgum (knock-knee), genu varum (bow-leg), and other deformities.
This work laid the foundation for modern orthopaedic correctional surgery, and Macewen’s beveled osteotome design became a standard tool in surgical practice well into the 20th century.

Macewen’s Triangle (Suprameatal Triangle / Mastoid Fossa)
Macewen’s triangle, also called the suprameatal triangle or mastoid fossa, is a bony surface landmark on the temporal bone used to access the mastoid antrum during mastoidectomy.
This small triangular depression on the temporal bone is a consistent anatomical landmark used to guide surgical entry into the mastoid antrum during mastoid procedures.behind the external auditory canal.
Anatomical Boundaries
- Superiorly – Posterior root of the zygoma
- Inferiorly – Arch of the osseous external auditory meatus
- Posteriorly – Vertical line dropped from the zygomatic root level with the meatus’s posterior edge
Macewen identified this region as a reliable guide to access the mastoid air cells and antrum safelyin his 1893 text Pyogenic Infective Disease of the Brain and Spinal Cord
The mastoid antrum may be reached by an opening made at the base of the triangle formed by the posterior root of the zygoma running somewhat horizontally above ; the portion of the descending plate of the squamous which forms the arch of the osseous part of the external auditory meatus below, and a base line uniting the two, dropped from the former on a level with the posterior border of the external auditory meatus. At this point there is usually a depression in the bone — though occasionally there is a slight prominence as if the antrum had bulged at that point. The apex of this triangular depressed area points forward. The author proposes to name this area the supra-meatal triangle
Key Medical Contributions
Macewen and anaesthesia (endotracheal intubation)
Macewen pioneered oral endotracheal intubation to secure the airway and allow uninterrupted delivery of chloroform anaesthesia during major operations in the mouth and pharynx. He proposed his method as an alternative to the then-standard approach of laryngotomy/tracheotomy with devices such as Trendelenburg’s tampon-cannula.
On July 5, 1878 he performed the first documented orotracheal anaesthetic intubation. Macewen described a patient undergoing removal of an epithelioma involving the pharynx/base of tongue, a procedure expected to bleed heavily. He inserted a tube through the mouth, beyond the vocal cords, and then packed the laryngeal inlet with sponge to prevent aspiration of blood while the patient continued to breathe through the tube; chloroform was administered without interrupting surgery, and respirations could be monitored via airflow through the tube (administered by Dr Symington).
As it was an operation which would cause considerable bleeding, precautions had to be taken to secure the air-passages from occlusion. Hitherto this had been effected by opening the windpipe, by laryngotomy, and the introduction of Trendelenburg’s tampon-canula. Instead of this I had determined, should an opportunity present, to introduce into the trachea, by way of the mouth, a tube which would extend beyond the vocal cords, and through which the patient would respire.
Macewen 1879
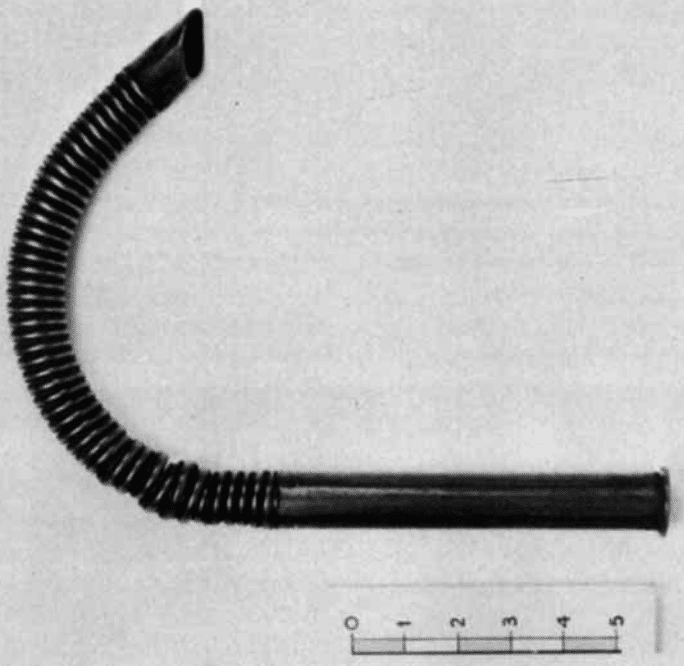
In his British Medical Journal paper on “introduction of tracheal tubes by the mouth,” Macewen set out the technique and argued that oral tracheal tubes could prevent blood entering the airway and could be used “for the purpose of administrating the anaesthetic.”
Brain tumour resection (1879)
On July 27, 1879, 31-year-old Sir William Macewen operated on Barbara Watson, a 14‑year‑old girl. She exhibited focal seizures affecting her right face and arm, along with slowed mental function, suggesting a lesion in the left frontal lobe.
Macewen used clinical localisation based on Jackson, Ferrier, and Broca’s neurological mapping, including motor and language findings, to pinpoint the lesion site. The procedure was meticulously documented in his private journal and published in the Glasgow Medical Journal.
The diagnosis was made solely from the character of the convulsions, and the tumour was found precisely where it had been indicated. The trephine was applied with the strictest attention to antiseptic precautions, and the patient made an uninterrupted recovery.
This case is widely recognized as the first documented successful brain tumour resection, predating similar operations such as Godlee et al. in 1884.
The pupil in head injury (1887)
John Cheyne (1777–1836) was among the first to document pupillary responses in acute brain injury. In his 1812 writings, he noted:
Great changes may be observed in the state of the different functions in the course of every attack of apoplexy… our prognostic is formed accordingly as the vital functions are more or less disordered.
He highlighted the prognostic value of fixed pupils and observed that:
With any return of sensibility our hopes rise, and with the diminution of it they are destroyed.
We do not despair until the pupil ceases to contract
In 1887, Macewen published The pupil in its semeiological aspects, and elaborated upon these observations with systematic clinical detail, describing pupillary changes across stages of raised intracranial pressure:
- Early: sluggish reaction or mild anisocoria
- Mid: unilateral dilation (uncal herniation indicator)
- Late: bilateral fixed dilation (terminal sign)
Key Quotes from Macewen (1887)
- On diagnostic stages of intracranial pressure using pupils: “The condition of the pupil forms a valuable index to the state of the intracranial contents, particularly in injuries where pressure on the brain is suspected.”
- On pupillary changes preceding consciousness recovery: “Where recovery followed, the first indications were frequently the restoration of the pupillary reflex to light, preceding the return of consciousness.”
- On unilateral dilation in head trauma: “One pupil widely dilated while the other retained its normal size and reaction was invariably associated with gross unilateral hemispheric lesion.”
- On the prognostic value of pupillary reaction: “In cases where the pupils remained dilated and insensible to light, the prognosis was almost invariably fatal.”
- On third-stage deterioration: “When the intracranial pressure reasserted itself… both pupils again assumed a widely dilated, fixed aspect—the final and fatal sign.”
First Documented Primary Bone Tumour (1876)
Macewen was among the first to describe and operate on a primary bone tumour of the femur, demonstrating histological differentiation between benign and malignant lesions. His approach laid the groundwork for modern orthopaedic oncology.
Bone Grafting He pioneered bone grafting using autologous bone segments to repair long bone defects. His technique involved meticulous shaping and sterile handling, becoming a cornerstone in reconstructive orthopaedics.
Major Publications
- Macewen W. Treatment for oedema glottidis by the introduction of a tube into the trachea. Meeting II.— Nov. 12th, 1878. Glasgow medical journal 1879; 11: 72-74
- Macewen W. On the introduction of tubes into the larynx through the mouth instead of tracheotomy or laryngotomy. Meeting XIV.— May 2nd 1879. Glasgow medical journal 1879; 12: 218 [Full article at: Louisville Medical News 1880; 10(7): 79-80][Macewen tracheal tube]
- Macewen W. Tumour of the dura mater — convulsions — removal of tumour by trephining — recovery Glasgow Medical Journal 1879; 12: 210-213
- Macewen W. Clinical Lecture on Antiseptic Osteotomy. Br Med J 1879;1:656-658 [Macewen’s Osteotome]
- Macewen W. Osteotomy with an inquiry into the aetiology and pathology of knock-knee, bow-leg, and other osseous deformities of the lower limbs. 1880 [Macewen’s Osteotomy]
- Macewen W. Clinical Observations on the Introduction of Tracheal Tubes by the Mouth, Instead of Performing Tracheotomy or Laryngotomy. Br Med J. 1880 Jul 31;2(1022):163-5 [Macewen tracheal tube]
- Macewen W. Observations concerning transplantation of bone. Illustrated by a case of interhuman osseous transplantation whereby over two-thirds of the shaft of a humerus were restored. Proc Roy Soc 1881; 32: 232–247. [Bone grafting]
- Macewen W. The pupil in its semeiological aspects. American Journal of the Medical Sciences. 1887; 94(187): 123-146 [The pupil in head injury]
- Macewen W. Pyogenic infective diseases of the brain and spinal cord: meningitis abscess of brain, infective sinus thrombosis. 1893 [Macewen’s Triangle] [Macewen’s sign]
- Macewen W. The growth of bone: observations on osteogenesis: an experimental inquiry into the development and reproduction of diaphyseal bone. 1912
References
Biography
- Sir William Macewen, F.R.S. Nature 1924; 113: 613–615
- Sir William Macewen C.B., M.D., F.R.C.S., F.R.S. Br Med J. 1924 Mar 29;1(3300):603–8.
- Sir William Macewen. Glasgow Med Jour, 1924; 101: 217
- Power D. Macewen’s osteotomy. British Journal of Surgery, 1925; 12(47): 413–416
- James CD. Sir William Macewen and anaesthesia. Anaesthesia. 1974 Nov;29(6):743-53.
- Keys TE. Sir William Macewen (1848-1924). Anesth Analg. 1974 Jul-Aug;53(4):537.
- James CD. Sir William Macewen. Proc R Soc Med. 1974 Apr;67(4):237-42
- Jennett B. Sir William Macewen 1848-1924. Pioneer Scottish neurosurgeon. Surg Neurol. 1976 Aug;6(2):57-60
- Miller JD. William Macewen: master of surgery. Va Med. 1979 May;106(5):362-8.
- Summerly P. Sir William Macewen (1848-1924): surgeon and clinical photographer. Scott Med J. 2007 Nov;52(4):44-6
- Macewen, Sir William (1848 – 1924). Plarr’s Lives of the Fellows
Eponymous terms
- Cheyne J. Cases of apoplexy and lethargy: with observations upon the comatose diseases. 1812
- Carson NB. The Cranial “Cracked-Pot” Sound as a Symptom of Cerebellar Tumors. Ann Surg. 1898;28(3):328–338
- Frost EA. The contributions of Sir William Macewen, a pioneer neurosurgeon, to an early quality assurance survey in anesthesia. J Neurosurg Anesthesiol. 1991 Mar;3(1):28-33.
- Canale DJ. William Macewen and the treatment of brain abscesses: revisited after one hundred years. J Neurosurg. 1996 Jan;84(1):133-42.
- Macmillan M. “I could see, and yet, mon, I could na’ see”: William Macewen, the agnosias, and brain surgery. Brain Cogn. 2004 Oct;56(1):63-76.
- Macmillan M. Localisation and William Macewen’s early brain surgery Part I: the controversy. J Hist Neurosci. 2004 Dec;13(4):297-325.
- Macmillan M. Localization and William Macewen’s early brain surgery Part II: The cases. J Hist Neurosci. 2005 Mar;14(1):24-56.
- Huntley JS, Osman MK. The osteotome: a design by Sir William Macewen. J Perioper Pract. 2014 Jul-Aug;24(7-8):182-4.
- Ellis H. Sir William Macewen and the first successful excision of an intracranial tumour. J Perioper Pract. 2020 Sep;30(9):283-284.
- Shah MH, Awuah WA, Adebusoye FT, Ahluwalia A, Tan JK, Atallah O. Sir William Macewen (1848-1924): Pioneering the Field of Neurosurgery with Early Breakthroughs in Tumor Resection. World Neurosurg. 2024 Sep;189:132-137.
- Wijdicks EFM. The Pupil as Indicator of a Cranial Vault Under Pressure: On Sir William Macewen contributions. Neurocrit Care. 2024 Mar 26.
Eponym
the person behind the name
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
