Not just pneumonia
aka Pulmonary Puzzler 001
A 30 year-old male presented with 24 hours of worsening respiratory distress, following a 5-day prodrome of cough, fever, diarrhoea, lethargy and malaise. He was obese, had a 20 pack-year smoking history, and a history of schizophrenia with no other comorbidities.
He developed progressive type 1 and 2 respiratory failure in the emergency department and was intubated using a bougie on the second attempt. His plasma sodium was 112 mmol/L and his plasma creatine kinase was 9,000 iu/L.
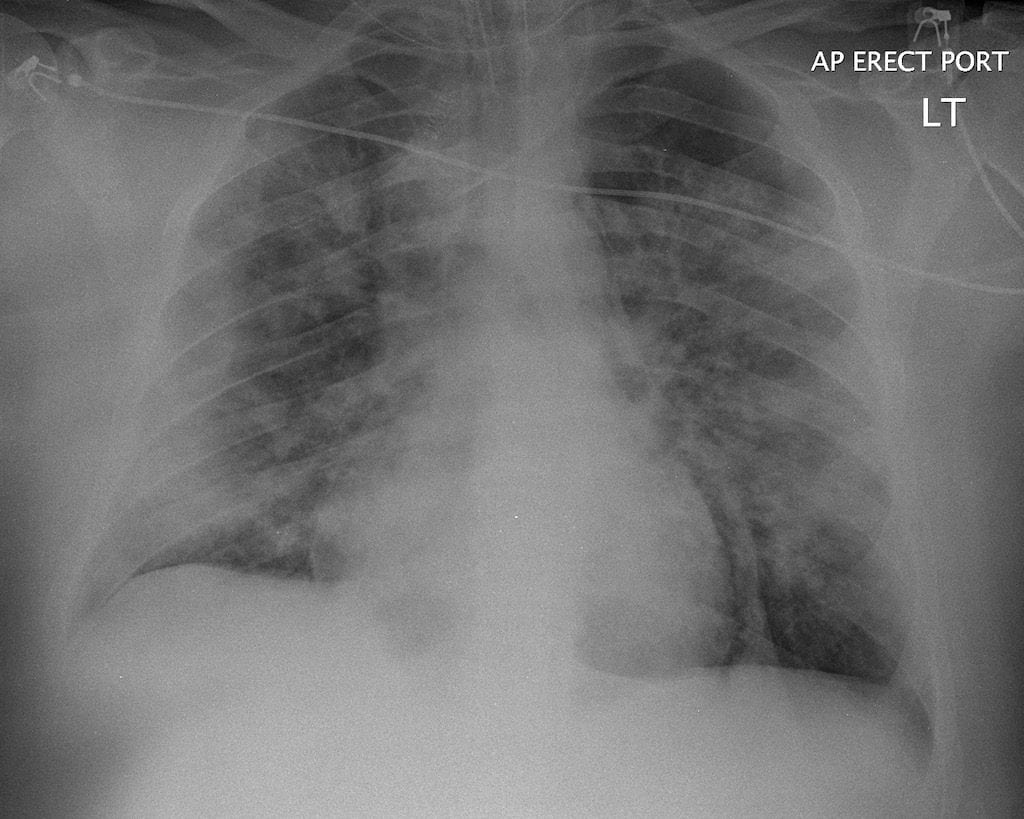
A chest radiograph performed 12 hours after intubation is shown.
Questions
Q1. Describe the chest radiograph.
Answer and interpretation
Chest radiograph findings:
- supine AP film of an obese male
- endotracheal tube present (arguably sited a little high in the trachea – the tip is between the medial heads of the clavicles but well above the level of the aortic knuckle)
- bilateral diffuse patchy infiltrates
- pneumomediastinum (a radiolucent band is clearly visible along the left heart border)
- A nasogastric tube is barely visible in the esophagus but gastric placement of the tip cannot be confirmed
- No pneumothorax or subcutaneous emphysema
Q2. What is your differential diagnosis for the presenting illness?
Answer and interpretation
Together with a history suggestive of an infective process, the widespread bilateral diffuse infiltrates are consistent with a viral pneumonitis or a bacterial pneumonia, or the latter supervening on the former.
Possible viral causes:
- Swine-origin influenza virus (SOIV) (H1N1 2009 pandemic influenza A)
- Other viruses – e.g. seasonal influenza A, ‘bird flu’ or ‘highly pathogenic avian influenza A virus of subtype H5N1’ (HPAI A (H5N1)), influenza B, parainfluenza, respiratory syncytial virus, adenovirus, coronavirus (e.g. SARS), hantavirus, metapneumovirus.
Bacterial pneumonias in smokers are usually caused by:
- Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Moraxella catarrhalis, Chlamydia pneumoniae, Legionella spp, and Pseudomonas aeroginosa. Mycoplasma pneumoniae should also be considered in this case.
A history of immunosupression, aspiration, exposure to animals, travel, and occupational exposures may implicate other potential etiologies.
Diffuse infiltrates can also be present with interstitial lung diseases (e.g. sarcoidosis, pneumoconiosis), neoplastic disease (e.g. lymphoma, metastatic carcinoma), and vasculitis (e.g. polyarteritis) but these differentials are much less likely in this setting.
Q3. Explain the laboratory and radiographic findings in light of the likely diagnosis and the clinical information given.
Answer and interpretation
Chest radiograph findings:
- Bilateral infiltrates – consistent with a viral pneumonitis or bacterial pneumonia as discussed in Q2.
- Pneumomediastinum – may have resulted from airway or alveolar rupture secondary to forceful coughing, traumatic intubation including use of the bougie, or barotrauma from positive pressure ventilation.
Laboratory findings:
- Hyponatremia– Further investigation is necessary, but possibilities include:
- dehydration
- syndrome of inappropriate antidiuretic hormone secretion (SIADH) secondary to pneumonia – usually suggestive of an atypical pneumonia, such as Legionnaire’s disease.
- adrenal insufficiency
- psychogenic polydipsia
- Elevated creatine kinase
- found in ~30% of ‘swine flu’ patients admitted to ICU.
- can occur in many viral and atypical pneumonias, such as Legionnaire’s disease and Mycoplasma pneumoniae.
- Rhadomyolysis may also have resulted from pressure areas due to prostration.
In the case on which this scenario is based, the patient had ‘swine flu’ – his sputum sample was positive for SOIV RNA on PCR analysis.
References
- The ANZIC Influenza Investigators. Critical Care Services and 2009 H1N1 Influenza in Australia and New Zealand. N Engl J Med. 2009 Oct 8.
- For more Pulmonary cases check out the LITFL Top 150 Chest X-Rays

CLINICAL CASES
Pulmonary Puzzler
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC