Second Cranial Nerve Lesions
Cranial nerve II is also known as the Optic nerve.
The pattern of visual defect found on clinical examination will reveal the anatomical location of the pathology within the optic neural pathways.
This chapter refers specifically to pathology of the peripheral and central optic nerve pathways that result in visual field defects.
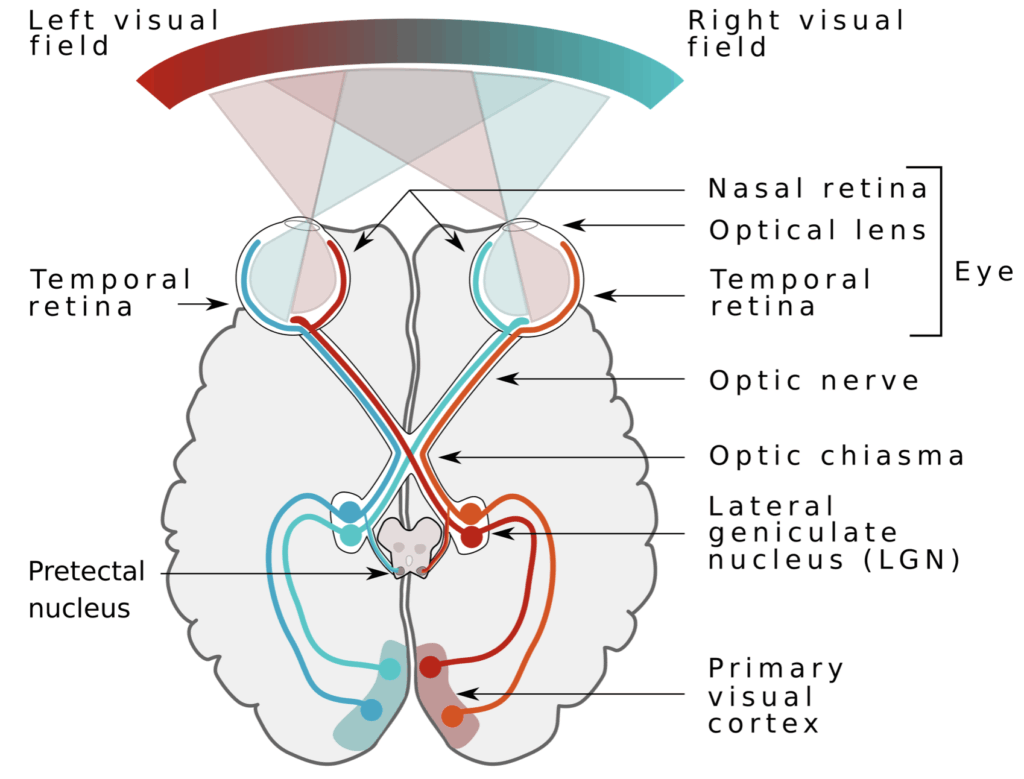
Anatomy
Course of the Optic Nerve
- The optic nerve leaves the orbit via the optic canal of the bony orbit, accompanied by the ophthalmic artery.
- The nerve is surrounded by the three meningeal layers, including the subarachnoid space.
- The two optic nerves meet at the optic chiasma, which sits on the diaphragma sellae, anterior to the pituitary stalk.
At the chiasma:
- Nasal fibres (carrying temporal field information) cross over.
- Temporal fibres (carrying nasal field information) stay lateral and pass back in the optic tract on the same side.
Beyond the chiasma:
- The optic tracts curve around the lateral side of the midbrain and divide into medial and lateral roots.
- The lateral roots synapse in the lateral geniculate bodies.
- Second-order neurones from the lateral geniculate bodies pass back in the optic radiations to the visual cortex:
- Lower temporal lobe fibres → upper visual fields.
- Upper parietal lobe fibres → lower visual fields.
Other fibres bypass the lateral geniculate bodies, entering the superior colliculus and relaying to the oculomotor and Edinger-Westphal nuclei — these are involved in ocular and pupillary reflexes.
Optic Nerve Innervations
- The optic nerve carries purely afferent special sensory neurones conveying impulses caused by photon capture by the retina.
Pathology
Lesions affecting the optic neural pathways will produce visual field defects.
| Visual Defect | Cause / Site |
|---|---|
| Concentric diminution of visual field (tunnel vision) | Glaucoma, Papilloedema |
| Central scotoma | Demyelination, Nutritional, Microvascular, Toxic |
| Irregular scotoma | Retinal tears, Intraocular lesions (e.g. vitreous haemorrhage) |
| Total unilateral visual loss | Unilateral eye disease, Optic nerve disease |
| Bitemporal hemianopia | Lesions of the optic chiasm (e.g. pituitary tumour, sella meningiomas) |
| Binasal hemianopia | Rare. Bilateral lesions affecting uncrossed fibres around chiasma (e.g. carotid siphon atheroma) |
| Homonymous hemianopia | Lesions of optic tracts or optic radiations. Defect nature depends on site: – Optic tract lesion → complete hemianopia without macular sparing. – Posterior optic radiation lesion → macular sparing if ischaemic cause. |
| Homonymous quadrantanopia | Lesions of optic tracts or radiations. – Temporal lobe lesion → upper quadrantanopia. – Parietal lobe lesion → lower quadrantanopia. |
Hayesian Visual Field Defect Chart
A view of Paris demonstrating visual field defect changes
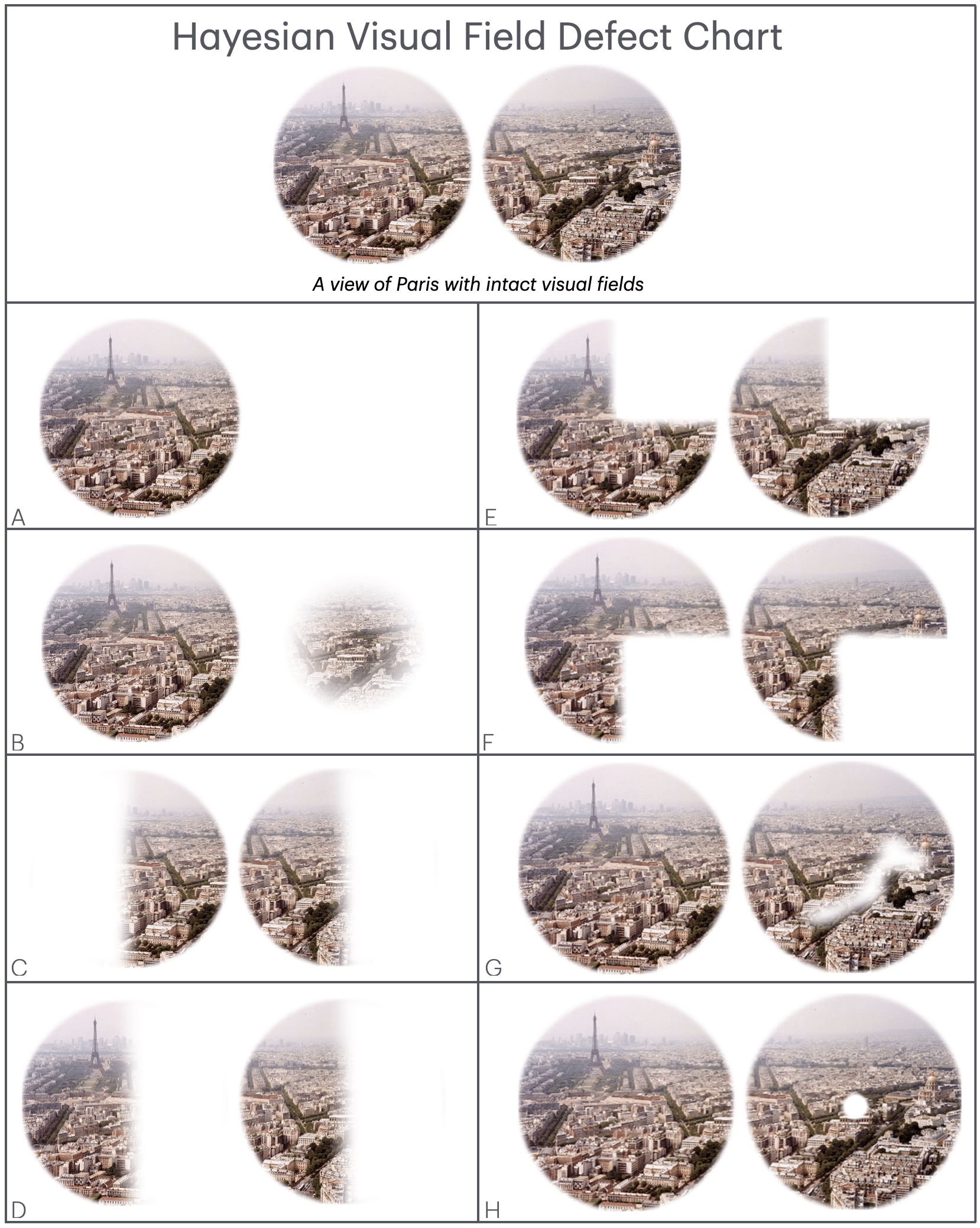
| Key | Visual Field Defect |
|---|---|
| A | …with a right sided complete optic nerve lesion |
| B | …with tunnel vision of the right eye |
| C | …with a lesion of the central optic chiasm, (bilateral hemianopia) |
| D | …with a right homonymous hemianopia |
| E | …with an upper right quadrantic hemianopia |
| F | …with a lower right quadrantic hemianopia |
| G | …with a scotoma of the right eye |
| H | …with an enlarged blind spot of the right eye |
Investigations
Ultrasound
B-scan ultrasound of the eye is useful when direct fundoscopic visualisation is difficult or impossible (e.g. hyphemas, corneal changes, cataracts).
- Detects vitreous haemorrhages or retinal detachments.
CT Scan / CT Angiogram
- CT: Good screening test for intracranial mass lesions.
- CT Angiogram: Done for suspected aneurysmal disease.
MRI
MRI is the best imaging modality for:
- Intracranial, ocular, and orbital space-occupying lesions.
- More sensitive and specific than CT.
- Distinguishes intrinsic soft tissue lesions of the eye and neural pathways not seen on CT.
Management
Management depends on the underlying cause of the lesion.
References
Publications
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Cranial Nerves. LITFL
- Nickson C. Cranial nerve lesions DDx. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


