Stroke Infarction: Thrombolysis
Carefully selected patients with acute ischaemic stroke can benefit from intravenous thrombolytic therapy, ideally within 9 hours of symptom onset.
This may be used in conjunction with endovascular clot retrieval.
Thrombolysis reduces the risk of moderate to severe disability by approximately 30%.
This treatment is complex, requiring dedicated hospital systems, imaging capability, and experienced stroke teams. Institutions without this infrastructure should not initiate thrombolysis.
This guide outlines general principles and does not replace local protocols or specialist consultation.
Pathophysiology
Cerebral infarction results in a central core of dead tissue surrounded by the ischaemic penumbra—partially perfused, potentially salvageable tissue.
Reperfusion within 9 hours, especially as early as possible, improves the chance of salvaging this penumbra.
Systems
Thrombolysis must be delivered in well-equipped EDs with:
- Experienced stroke teams
- Imaging capabilities (CT, CTA, CTP)
- ICU support
Some regions use Mobile Stroke Units for prehospital thrombolysis.
Hospitals should have Code Stroke protocols that mobilise:
- ED clinicians
- Radiology
- Neurology
- ICU
Criteria
Inclusion criteria
- Clinically measurable stroke (typically NIHSS > 4)
- Within 9 hours of symptom onset (earlier = better)
- CT, CTA, CTP confirm no haemorrhage or mimic
Wake-up strokes may be considered using CT perfusion mismatch or sleep midpoint as onset time.
Absolute contraindications
- Significant disability (Modified Rankin Score ≥ 4)
- BP > 180/110 mmHg unresponsive to IV therapy
- Anticoagulation therapy:
- DOACs: apixaban (<12h), rivaroxaban (<24h), dabigatran (unless reversed)
- Heparin: UFH with raised APTT, LMWH in last 12h
- Warfarin with INR ≥ 1.7
- Platelets < 100 x 10⁹/L
- Glucose < 2.8 mmol/L (reassess after correction)
- CT evidence of large infarction (>1/3 MCA territory)
- Septic embolism
- Previous ICH
- Aortic dissection
- Active bleeding
- Recent GI ulcer/varices
Relative contraindications
These require specialist judgement:
- Premorbid disability (Rankin ≥ 4)
- Major trauma, surgery, CPR in past 14 days
- CNS tumours (except meningioma)
- Recent MI (<30 days)
- Pregnancy
- Previous stroke (<3 months)
- Age <18 (discuss with paediatrics)
- DOAC use 12–48h ago
Investigations
Bloods:
- FBC
- U&Es / glucose
- LFTs
- Coags
- CRP / ESR
- Group and hold
Thrombolysis should not be delayed awaiting non-critical results.
ECG: Required but must not delay treatment.
Imaging:
- Plain CT (rule out haemorrhage)
- CT angiogram
- CT perfusion scan
Management
Code Stroke activation
- ABC management
- 1–2 IV access points
- Draw bloods
- Check BSL
- 12-lead ECG
- Control BP (<180/110 mmHg)
- IV nicardipine (preferred)
- IV labetalol / GTN / hydralazine
Thrombolytics
Decision made after radiology + neurology review.
Discuss risks/benefits with patient or NOK if possible.
Tenecteplase (0–4.5 hours):
- 0.25 mg/kg IV bolus over 10 sec, max 25 mg
Alteplase (tPA) (4.5–9 hours):
- 0.9 mg/kg IV, max 90 mg
- 10% as 1-minute bolus
- 90% as 60-minute infusion
Post-thrombolysis
- Repeat CT brain at 24–36 hours
- Withhold aspirin, antiplatelets, anticoagulants for 24 hours
- Urgent CT if neurological deterioration occurs
Disposition
- Admit to HD/ICU under stroke team
- Patients remain in ED during thrombolysis
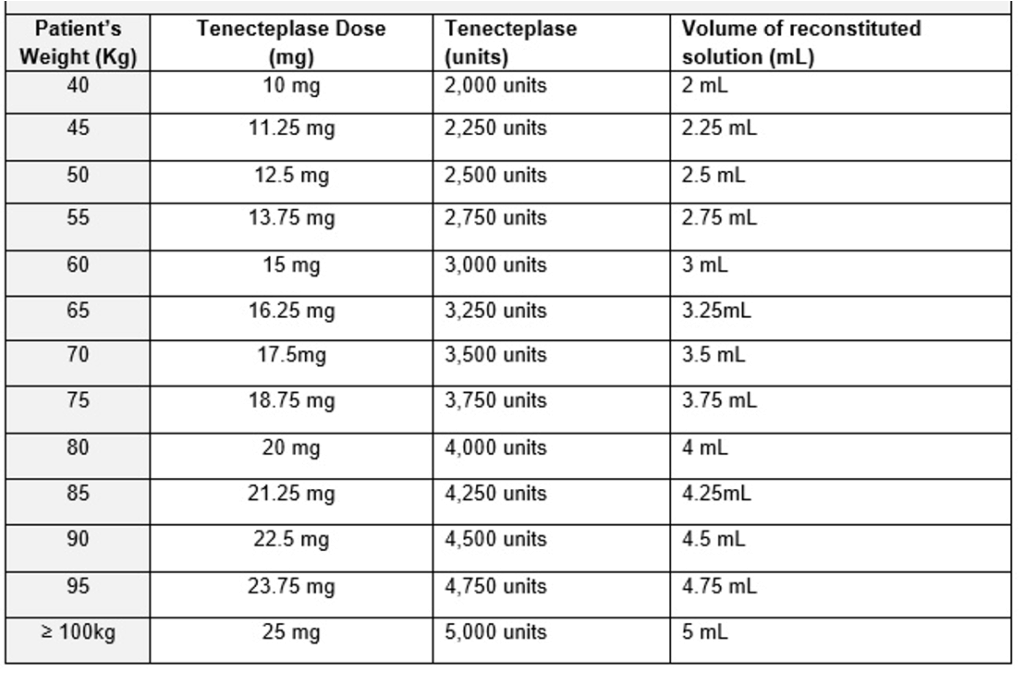
Appendix 1
Tenecteplase dosing in the setting of ischaemic stroke:
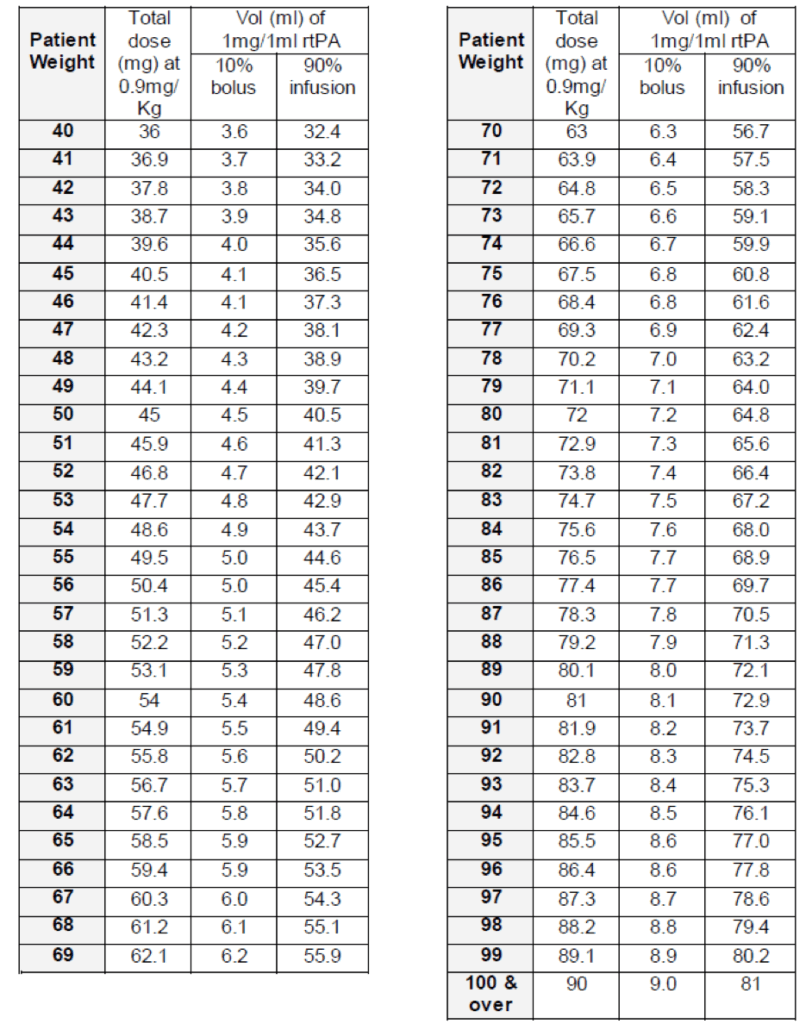
Appendix 2
Alteplase infusion in the setting of ischaemic stroke
References
Publications
- Tremonti C, Thieben M. Drugs in secondary stroke prevention. Aust Prescr. 2021 Jun;44(3):85-90.
- Clinical Guidelines for Acute Stroke Management – National Stroke Foundation
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Cerebral Hemispheres. LITFL
- Nickson C. Stroke Thrombolysis. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


