Adding insult to injury?
aka Trauma Tribulation 012
You’re in the trauma bay coordinating the assessment and management of a 40 year-old man who was involved in a motor vehicle crash. A nurse passes you a bluey, some KY and sterile gloves as the patient is about to be logged rolled.
Are you going to perform a digital rectal examination (DRE) on this man?
One finger in the throat and one in the rectum makes a good diagnostician
Wiliam Osler
Questions
Q1. What are you trying to detect when you perform a DRE in a trauma patient?
Answer and interpretation
Th DRE is performed to detect the following key findings:
- rectal hemorrhage
- rectal mucosal injury or wall defects
- loss of anal tone suggesting spinal cord injury
- palpable pelvic fractures
- a high riding prostate suggestive of posterior urethral disruption
Q2. Is it mandatory to perform a DRE in trauma patients?
Answer and interpretation
No
Traditional ATLS teaching was that a DRE is mandatory in trauma patients: “a finger or tube in every orifice”. This is no longer the case. The 8th edition of ATLS recommends that ‘DRE be performed selectively before inserting an indwelling urinary catheter’ (Kortbeek et al, 2008).
Over the past 10 years or so, the published literature has consistently downplayed the role of the DRE in the assessment of trauma patients. It is clear that:
DRE rarely changes the management of trauma patients.
- DRE was felt to change management in only in 1.2% of cases in Porter and Ursic’s prospective observational study (2001) and only 4% in Esposito et al’s prospective study (2005).
- Espsoito et al (2005) found that none of 512 patients would have had a significant injury missed had the DRE been omitted.
The DRE is not a useful screening test in trauma patients.
- In a retrospective study of over 1400 patients, Shlamovitz et al (2007) found that the DRE was only 23% sensitive for a composite of significant injuries in trauma patients.
- This means that about three-quarters of the time the DRE will miss significant injuries (such as GI perforation, rectal mucosal injury, urethral rupture, pelvic fracture and spinal cord injury).
Q3. What are the downsides of performing a DRE in a trauma patient?
Answer and interpretation
Some have argued that despite the poor sensitivity of the DRE, it should still be performed as part of a complete examination as it is “cheap, quick and non-invasive”.
I disagree…
DREs should only be performed selectively
…and I certainly don’t consider DREs to be ‘non-invasive’.
Downsides of performing DREs in trauma patients include:
- physical discomfort
- emotional distress
- risk of verbal and/ or physical violence from an agitated patient
- litigation
- possible infection risk — e.g. contamination of local wounds; risk of transmission of infection to the clinician (likely to be extremely low)
- injury — potential for worsening of the patient’s injuries (e.g. unstable pelvic fracture, rectal defects); and also risk of injury to the clinician (e.g. foreign bodies, bone fragments)
- the occurrence of false positive and false negative DRE findings
Q4. Why might DREs be unreliable?
Answer and interpretation
Factors contributing to DREs being unreliable include:
- DREs are often performed by junior staff
— either because it is considered a menial task, or so that the junior staff ‘gain more experience’. - positive findings on DRE are rare… anyone ever felt a ‘high riding’ prostate?… (i.e. before the diagnosis of posterior urethral disruption was confirmed by some other means…)
- the findings on DRE have poor inter-observer agreement
— this is well document for the assessment of prostate size and the detection of rectal tumours… even when performed by ‘experts’ such as urologists and proctologists.
Q5. Are ‘false positive’ and ‘false negative’ DREs a concern?
Answer and interpretation
Yes…
DRE findings may be falsely positive or negative.
Esposito et al (2005) found that 6% of DREs in trauma patients had findings that were later shown to be false (either positve or negative) when other investigations or follow up over time was performed.
Shlamovitz et al (2007) found high rates of falsely negative DREs:
- 63% for decreased anal sphincter tone
- 94% for the presence of gross rectal blood
- 67% for disruption of the rectal wall integrity
- 100% for palpation of bony fragments
- 80% for abnormal position of the prostate.
False negative DREs may lead to
- injuries being missed, resulting in increased morbidity and/ or mortality
- delays in performing necessary investigations and/ or interventions
False positive DREs may lead to:
- unnecessary investigations (cost, time, radiation, contrast exposure, decreasing access for other patients, etc)
- unnecessary interventions (the possibilities include prolonged time in a c-spine collar, unnecessary fasting, being cut open for no reason, etc)
- prolonged observation (possible increase in hospital length of stay)
Q6. Do you need to perform a DRE in trauma patients to detect posterior urethral injury?
Answer and interpretation
Probably not… You can usually rely on other clinical findings and a (gentle) attempt at IDC insertion will reveal all.
Ball et al (2009) found that in patients with posterior urethral disruption, 60% of the time there there were no clinical signs prior to urinary catheter insertion (41 urethral injuries were included in this retrospective study). Possible clinical signs and their sensitivities are shown below:
- blood at the urethral meatus (20% sensitivity)
- gross hematuria prior to catheter insertion (17% sensitivity)
- abnormal prostate position (2% sensitivity)
- scrotal or perineal echymosis
- inability to void
(Unfortunately likelihood ratios could not be calculated from the data provided in the paper.)
Why is DRE to detect ‘abnormal prostate position’ such a poor test? In addition to the reasons discussed in Q4, examination is often limited by tenderness or the finding of a ‘high riding prostate’ may be concealed by hematoma formation from a coexistent pelvic fracture or vessel injury.
- Abnormal prostate position is near useless for detecting posterior urethral injury.
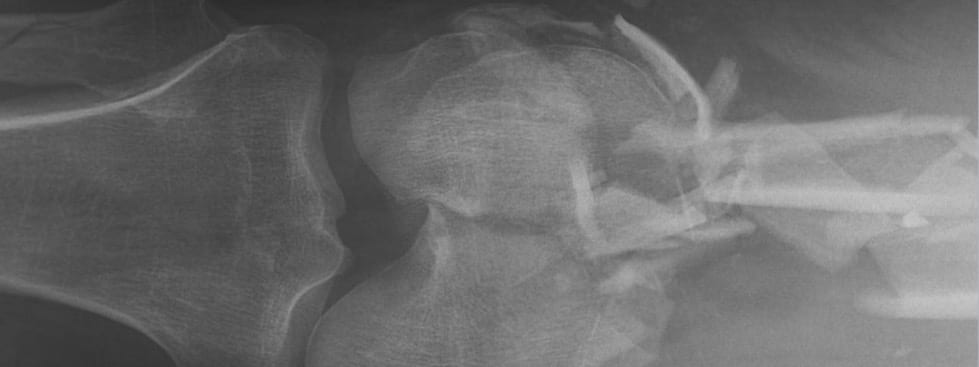
The key finding that should make you think about posterior urethral disruption is the presence of pelvic fractures. Ball et al (2009) found that 95% patients with posterior urethral injuries occurred had pelvic fractures.
- Consider posterior urethral disruption if a pelvic fracture is present.
Current ATLS guidelines advise that a retrograde urethrogram be performed before inserting an indwelling urinary catheter (IDC) in trauma patients if posterior urethral injury is suspected. In practice, this rarely occurs. This is partly because posterior urethral injury is often first suspected once frank blood is returned following attempted IDC insertion, or if the IDC is difficult to pass. It probably doesn’t matter in the long run if posterior urethral disruption is diagnosed this way — just be very gentle when you’re passing an IDC!
- Suspect posterior urethral disruption if there is hematuria on IDC insertion or if the IDC doesn’t pass easily.
Michael McGonigal describes how to perform a retrograde urethrogram on the excellent Trauma Professional’s blog.
- Perform a retrograde urethrogram to confirm posterior urethral disruption.
Q7. Do you need to perform a DRE in trauma patients to detect spinal cord injury?
Answer and interpretation
Probably not, unless the patient has a neurological deficit.
If the patient is otherwise neurologically intact on clinical examination, anal tone is very unlikely to be altered.
- Normal anal tone does NOT exclude spinal cord injury.
Sensitivity is too low for DRE to have have much bearing on making a serious diagnosis like spinal cord injury:
- Shlamovitz et al (2007) found DRE was only 37% sensitive with a negative likelihood ratio (LR) of 0.66
- Guldner et al (2006) had similar findings, with a negative LR of 0.5.
Of course, a positive DRE finding of decreased anal tone is more useful, but these patients are likely to have other reasons for suspecting spinal cord injury (such as paralysis…).
- Shlamovitz et al (2007): positive LR = 8.5
- Guldner et al (2006): postive LR = 6.8
Two important points about the use of DRE in patients with suspected spinal cord injury:
- Assessing rectal tone is of little use if the patient has been given neuromuscular blockers following intubation. Tone may also be reduced in the unconscious patient, as a result of post-intubation sedation or traumatic brain injury for instance.
- In the patient with neurological deficits, assessment for sacral sparing is important. This can be assessed by checking anal tone, but anal wink or the bulbocavernosus reflex are alternatives and may be more useful and/or better tolerated.
Q8. Do you need to perform a DRE in trauma patients to detect bowel injury?
Answer and interpretation
Usually not… sensitivity is poor and other investigations are likely to be needed.
The DRE is only 6% sensitive for bowel injury (LR- 0.95), and only 33% sensitive for rectal mucosal tears (LR- 0.65 with confidence intervals that crossed 1) according to Shamlovitz et al (2007). As such it cannot be used a screening test in trauma patients to exclude either of these types of injuries.
Don’t rely on a negative DRE in a patient at high-risk of a bowel or rectal injury. Such patients need further investigation.
On the other hand, Shlamovitz et al (2007) found that a positive DRE was more useful for bowel and particularly rectal injury.
- 98.9% specific for bowel injury (i.e. PR hemorrhage detected) (LR+ 5.2)
- 99.8% specific for disrupted rectal wall integrity (LR+ 996)
But we need to take into account the fact that patients with these positive findings are likely to require further investigation anyway based on other findings (such as the spear sticking out of his or her perineum…).
Q9. So, when should you perform a DRE in a trauma patient?
Answer and interpretation
There probably is a subgroup of trauma patients (as yet poorly defined) for whom a DRE is useful and may change management.
This subgroup may include patients with:
- pelvic fractures (complications and associated injuries may be detected)
- abnormal neurological findings
- hypotension
- penetrating abdominal or perineal trauma with possible rectal or other GI involvement
- abdominal tenderness
Again, even in these patients further investigations are typically indicated anyway, which may render the DRE findings redundant. I suspect that most clinicians err on the side of performing a DRE given that, throughout the ages, we have been beaten over the head with the notion that failure to perform a DRE is a sign of gross incompetence (“if you don’t put your finger in it, you’ll put your foot in it”).
Perhaps it is easier to say which trauma patients don’t need a DRE…
Gulder et al (2004) published an as yet unvalidated clinical decision rule for performing DRE in trauma patients, based on an observational study of 862 patients. They found that there is a 0 to 0.8% probabilty of a ‘true positive’ abnormal DRE in patients with all three of:
- a normal neurological exam
- aged <65 years
- absence of blood at the urethral meatus
Q10. What are the take home messages from all of this?
Answer and interpretation
The take home messages for me are that DREs in trauma patients:
- should be performed selectively
— you must have a reason for performing this invasive examination… don’t feel you have to do it! But make sure your reasoning for not performing a DRE is equally sound. In most patients the DRE won’t be useful. - can often be delayed or be performed at the time of a subsequent investigation (e.g. colonoscopy) or intervention (e.g. laparotomy) if necessary
- may be redundant in light of other clinical findings or if further investigation is indicated by other clinical findings
- may be best performed by an experienced practitioner (although there is little or no evidence that their findings are any better than those of their junior colleagues)… and only once!
References
- Ball CG, Jafri SM, Kirkpatrick AW, Rajani RR, Rozycki GS, Feliciano DV, Wyrzykowski AD. Traumatic urethral injuries: does the digital rectal examination really help us? Injury. 2009 Sep;40(9):984-6. Epub 2009 Jun 16. PMID: 19535063.
- Esposito TJ, Ingraham A, Luchette FA, Sears BW, Santaniello JM, Davis KA, Poulakidas SJ, Gamelli RL. Reasons to omit digital rectal exam in trauma patients: no fingers, no rectum, no useful additional information. J Trauma. 2005 Dec;59(6):1314-9. PMID: 16394903.
- Guldner G, Babbitt J, Boulton M, O’Callaghan T, Feleke R, Hargrove J. Deferral of the rectal examination in blunt trauma patients: a clinical decision rule. Acad Emerg Med. 2004 Jun;11(6):635-41. PMID: 15175201.
- Guldner GT, Brzenski AB. The sensitivity and specificity of the digital rectal examination for detecting spinal cord injury in adult patients with blunt trauma. Am J Emerg Med. 2006 Jan;24(1):113-7. PMID: 16338517.
- Kortbeek JB, et al. Advanced trauma life support, 8th edition, the evidence for change. J Trauma. 2008 Jun;64(6):1638-50. Review.PMID: 18545134.
- Porter JM, Ursic CM. Digital rectal examination for trauma: does every patient need one? Am Surg. 2001 May;67(5):438-41. PMID: 11379644.
- Shlamovitz GZ, Mower WR, Bergman J, Crisp J, DeVore HK, Hardy D, Sargent M, Shroff SD, Snyder E, Morgan MT. Poor test characteristics for the digital rectal examination in trauma patients. Ann Emerg Med. 2007 Jul;50(1):25-33, 33.e1. Epub 2007 Mar 27. PMID: 17391807.
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at the Alfred ICU in Melbourne. He is also a Clinical Adjunct Associate Professor at Monash University. He is a co-founder of the Australia and New Zealand Clinician Educator Network (ANZCEN) and is the Lead for the ANZCEN Clinician Educator Incubator programme. He is on the Board of Directors for the Intensive Care Foundation and is a First Part Examiner for the College of Intensive Care Medicine. He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives.
After finishing his medical degree at the University of Auckland, he continued post-graduate training in New Zealand as well as Australia’s Northern Territory, Perth and Melbourne. He has completed fellowship training in both intensive care medicine and emergency medicine, as well as post-graduate training in biochemistry, clinical toxicology, clinical epidemiology, and health professional education.
He is actively involved in in using translational simulation to improve patient care and the design of processes and systems at Alfred Health. He coordinates the Alfred ICU’s education and simulation programmes and runs the unit’s education website, INTENSIVE. He created the ‘Critically Ill Airway’ course and teaches on numerous courses around the world. He is one of the founders of the FOAM movement (Free Open-Access Medical education) and is co-creator of litfl.com, the RAGE podcast, the Resuscitology course, and the SMACC conference.
His one great achievement is being the father of three amazing children.
On Twitter, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
