Amphetamine poisoning
Amphetamine, first synthesised in 1887 in Germany by Lazar Edeleanu who named it phenlisopropylamine. Ephedrine is a plant derivative from the plant Ma-Huang (Ephedra), 5 years later the Japanese had synthesised methamphetamine from ephedrine.
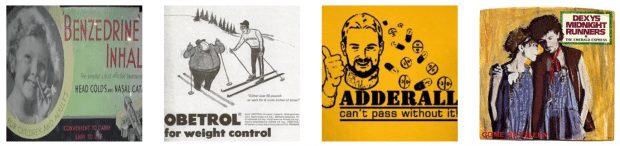
It was not until 1934 that a pharmacological use had been established. Smith, Kline and French started selling the amphetamine inhaler “Benzedrine” as a decongestant. During World War II amphetamine and methamphetamine was widely used by multiple forces known for its stimulant effects. Many prescriptions were given out for all sorts of ailments including obesity.
It was not until the 1950s in Japan and 1960s in America that stricter controls were introduced once the addictive and detrimental properties were known by which time slang terms for the pills included ‘pep pills’ and black market production began.
Its use has been so common in many facets of life that it was not until 2006 that the Major League Baseball formally enforced a ban on its players.Other groups using derivatives such as Adderall include college students to help with concentration and young white-collar workers who find they need it to perform adequately. Finally, for the best pop knowledge fact, the band who performed the number one hit “come on Eileen” are named after dexedrine – Dexys Midnight Runners.
Amphetamine Toxicology:
- Amphetamines and other sympathomimetics produce both peripheral and central sympathomimetic effects.
- Lethal complications include: Severe Hyperthermia and Hypertension, Dysrhythmias, Ischaemia, Dissections and Intracranial haemorrhage.
- Small doses in the intolerant can produce significant toxicity (especially children – ‘one pill can kill’).
- The presence of complications require aggressive management and investigation.
- Benzodiazepines are largely used for Hypertension, Tachycardia and Hyperthermia.
- Repeated use leads to longterm neuropsychiatric sequelae.
- AVOID beta-blockers. [see also Cocaine and Beta-blockers dogma]
- MDMA and cathinone typically cause hyponatraemia resulting in seizures.
Tox Tute AUDIO – Amphetamine (Quick version)
Tox Tute AUDIO – Amphetamine
The show notes are presented as a ‘show and reveal‘ mini quiz.
Question 1
Resus: What complications require immediate attention?
Reveal the Answer
- Hypertension
- Acute Coronary Syndrome
- Seizures and Agitated Delirium
- Hyperthermia
- Hyponatraemia
Question 2
Resus: What is the mechanism for the ACS and thus why do we avoid thrombolysis?
Reveal the Answer
- Vasospasm
- Dissection
- For both the above causes thrombolysis would not work, it is also relatively contraindicated if the patient has severe hypertension, headache or focal neurological deficit due to the concerns surrounding a dissection or intracranial haemorrhage.
Question 3
Resus: What symptoms or pathology would be a contraindication to using thrombolytics in an acute coronary syndrome?
Reveal the Answer
- Severe hypertension
- Seizures
- Intracranial haemorrhage
- Aortic dissection
Question 4
Resus: What drugs beyond a benzodiazepine could you use for severe agitation?
Reveal the Answer
- Droperidol 2.5 – 10mg IV or
- Olanzapine 10mg IM
- If the patient is at severe risk to self, staff or others they may require a rapid sequence induction with intubation and ventilation.
Question 5
Resus: At what serum sodium and symptoms should you treat hyponatraemia? What will you use and at what dose and infusion?
Reveal the Answer
- Most texts advocate correcting a sodium below 120 mmol/L with associated altered mental status or seizures.
- The solution of choice is 3% sodium chloride, 4 ml/kg over 30 mins and then repeat serum sodium levels to achieve a serum sodium >120 mmol/L.
Question 6
Resus: What temperature would you want continuous core monitoring and what treatments would you provide at this point? What temperature requires rapid external cooling and paralysis?
Reveal the Answer
- A Temperature >38.5 requires close monitoring. Use benzodiazepines and fluid resuscitation to help reduce further rises in temperature.
- Temperatures >39.5 require rapid external cooling which is only reasonably possible if the patient is paralysed, intubated and ventilated.
Question 7
Resus: We keep saying not to give beta blockers but what would beta blockade do at a receptor level?
Reveal the Answer
“In theory” it would promote a situation of unopposed alpha stimulation resulting in vasoconstriction. See additional resources for related video.
Question 8
Risk assessment: What percentage of amphetamine emergency presentations have a seizure?
Reveal the Answer
- 4%
Question 9
Investigations: Your patient has an altered GCS, what investigations would you perform?
Reveal the Answer
- Blood glucose level
- Venous blood gas to establish sodium value
- CT brain +/- angiogram if there are focal neurological deficits or concerning chest pain.
Question 10
Investigations: Your patient reports he has been running around all night, what potential complications might they have and how would you investigate and manage this?
Reveal the Answer
- Potential for rhabdomyolysis, detected by ordering a CK, EUC and a urine test for myoglobin.
- Supportive care would involve IV hydration and tracking of their renal function and CK 8 to 12 hours later.
Question 11
Decontamination, enhanced elimination and antidotes: Is there a role for activated charcoal, dialysis or any antidotes?
Reveal the Answer
- In most circumstances there is no indication for any of the above that good supportive care does not provide.
- Very rarely, in a massive ingestion or in a body stuffer you were concerned about it might be necessary to intubate to assist with decontamination or enhanced elimination (seek expert advice before doing this).
Question 12
Disposition: Your patient is requiring 20 min boluses of benzodiazepines to control their blood pressure and tachycardia, they are otherwise stable and easy to manage. When can you discharge them?
Reveal the Answer
Patients need to be symptom free for 4 hours post benzodiazepine administration. This however, maybe easier said than done and relies on clinical judgement and the safety net that each individual patient has.
References
- Gray SD et al. Amphetamine related presentations to an inner city tertiary emergency department: a prospective evaluation. Medical Journal of Australia 2007; 186(7):336-339.
- Jenner L et al. Management of patients with psychostimulant toxicity: guidelines for emergency departments. Canberra, Australian Government Department of Health and Ageing, May 2006.
- See cocaine page for further ‘show and reveal’ questions surrounding management.
- Controversies with giving beta-blockers is it just dogma?
Additional Resources
Adrenoceptors and the sympathomimetic syndrome
Movement disorders and toxicology
Converting % to mg/ml and Hypertonic Saline

Toxicology Library
DRUGS and TOXICANTS
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.