Another Widow Maker
aka ECG Exigency 015
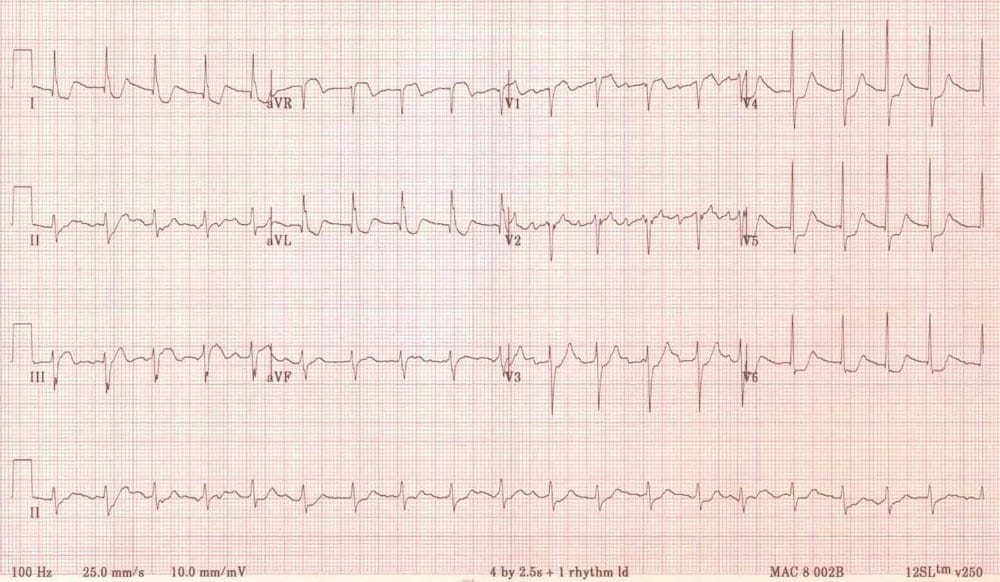
A 55 year old man presents with a good chest pain story that makes you nervous. An ECG is taken on arrival and shown below:
His chest pain and his ST depression seem to settle with some GTN and morphine. You load him with Aspirin, Clopidogrel and Heparin and admit him under the cardiologists with a view to angiography in the next 24 hours.
The junior cardiology registrar seems a bit overwhelmed but is delighted with your management so far and happily accepts the patient.
You arrive in work the next morning and the first thing the night team say is that phrase dreaded by Emergency Doctors the world over:
‘Do you remember that patient you saw last night…?‘
Turns out he crashed and burned in the Coronary care unit and is now in ICU on an intraaortic balloon pump with a guarded prognosis…
The cardiologist storms into the ED and corners you yelling:
‘Didn’t you know ST elevation in aVR means left main coronary artery occlusion?‘
Is he right? Could you or should you have done anything differently?
Is aVR ST elevation a predictor of LMCA occlusion?
Answer and Interpretation
- aVR is the forgotten ECG lead – some even suggest we should call it an 11 lead ECG. ST segment elevation in aVR is often ignored as just being a reciprocal change but does it mean more than that?
- The answer is yes, but it probably isn’t as much of a direct correlate with LMCA stenosis as the cardiologist is stating.
- Some quote a specificity of 98% when ST elevation in aVR is also present in aVL. However this figure seems to be from several deeply flawed papers with small numbers of highly selected non-emergency patients.
- The largest study on ST elevation in aVR found it was associated with LMCA stenosis when compared to patients with ACS without elevation, but nowhere near as strongly as previously suggested (14.7% of patients with ≥ 1mm vs 5.1% without).
- When LMCA stenosis was combined with 3 vessel disease into a composite endpoint (ie: the traditional indications for CABG) it performed substantially better – 55.9% vs 26.1. It’s a good indicator, but certainly not a done deal.
Is aVR ST elevation a Mortality predictor in LMCA occlusion?
Answer and Interpretation
- One study of 775 consecutive patients with NSTEMI found in hospital mortality was 1.3% in those without ST elevation in aVR, compared with 19.4% in those with ≥ 1mm ST elevation.
- However a subsequent much larger (and possibly definitive study) of 5064 patients from the GRACE registry suggests a much less startling , but still substantial difference in mortality (4.2 % vs 7.9%. p<0.03).
In Conclusion…
Reveal Answer
Key Points
- LMCA stenosis is bad – 70 % mortality without surgery / PTCA.
- ST Elevation of more than 1mm inaVR in the setting of Acute Coronary syndrome:
- is associated with left mainstem disease and 3 vessel disease
- suggests urgent angiography is necessary
- is associated with an increase in mortality.
- probably not an indication for emergent angiography @ 3am unless the patient is not settling with standard medical therapy.
References
- Yan AT, Yan RT, Kennelly BM, Anderson FA Jr, Budaj A, et al.Relationship of ST elevation in lead aVR with angiographic findings and outcome in non–ST elevation acute coronary syndromes. Am Heart J. 2007 Jul;154(1):71-8. PMID: 17584554
- Kosuge M, Kimura K, Ishikawa T, Ebina T, et al. Combined prognostic utility of ST segment in lead aVR and troponin T on admission in non-ST-segment elevation acute coronary syndromes. Am J Cardiol. 2006 Feb 1;97(3):334-9. PMID: 16442391
- Kosuge M, Ebina T, Hibi K, Morita S, et al. Early, accurate, non-invasive predictors of left main or 3-vessel disease in patients with non-ST-segment elevation acute coronary syndrome. Circ J. 2009 Jun;73(6):1105-10. PMID: 19359810
- S Kurisu, I Inoue, T Kawagoe, M Ishihara, et al. Electrocardiographic features in patients with acute myocardial infarction associated with left main coronary artery occlusion. Heart. 2004 Sep;90(9):1059-60. PMID: 15310704
- Barrabés JA, Figueras J, Moure C, Cortadellas J, Soler-Soler J. Prognostic value of lead aVR in patients with a first non-ST-segment elevation acute myocardial infarction. Circulation. 2003 Aug 19;108(7):814-9. PMID: 12885742
- Hampton, JR. The ECG In Practice, 6e
- Mattu A, Brady W. ECG’s for the Emergency Physician 1
- Mattu A, Brady W. ECGs for the Emergency Physician 2
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric, 6e
- Wagner, GS. Marriott’s Practical Electrocardiography 12e
Further Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
CLINICAL CASES
ECG EXIGENCY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |

hi Ed
another extraordinary case.
Stephen Smith, an ECG guru from Hannepin in minneapolis, (i hope i ma quoting him correctly!) says that true acute complete occlusions of the left main almost never make it to us, because it is so devastating. and on his blog, he has shown a case of true OMI involving the LM and there was actually ST seg depression (!) in aVR., as well as global ischemic changes.
i think that st elevation in aVR, with global depression elsewhere often represents significant multi-vessel disease, or a critical narrowing /stenosis (but not yet complete occlusion ) of the left main, or very prox LAD. ( i would not give this patient PLavix , since they may require open heart surgery, like yesterday.).
sometimes, say with multi-vessel severe disease, these findings are seen when the heart is “stressed” by other more critical factors, like sepsis, or afib with RVR.
one more point, if i may. this ecg is quite interesting.
see leads III, and V1. there is up-coving of the T waves, very abnormal, i think. STEMI-ish.
i wonder if the disease/occlusion involved something like an OM/diagonal off the prox LAD with wrap around to the apex, inferiorly.
it would have been nice to see serial ecg’s , perhaps an echo, and the angiogram itself.
and a more polite cardiologist.
thank you again, Ed
tom
There is a big difference between “occlusion” (100%) and “stenosis” (1-99%), and you (and others) seem to use these terms interchangably here, which is not correct. A real occlusion of the left main is rarely survived acutely out in the field, unless there is very good collateral circulation from the right coronary artery (supplying the anterior wall with blood instead).
The more concerning thing on the above ECG is not the finding in aVR (what people always seem to get hung up about), but the widespread ST-Depression in many leads, which should alert the person reading the ECG that there is a widespread severe perfusion problem, usually severe stenoses in all 3 heart arteries, sometimes combined with a stenosis in the left main (as the same progress, arteriosclerosis, can obviously also narrow that bit of the coronary tree). So ST-elevation in aVR should not be seen isolated, but in the picture of the global myocardial ischaemia. And someone with such widespread ischaemia should have their coronaries looked at rather rapidly. That´s why the cardiologist was so annoyed that this wasn´t done earlier and the patient arrested.
Great post.
Considering there looks like STE in Lead 111 in addition to the STE in aVR + v1 and widespread STD throughout, could this be Aslanger Pattern. So Tripple vessel disease with RCA occlusion?
Thanks
Humbly. In addition to the Aslanger pattern, it seems that the patient is not in sinus rhythm. It seems to me to be a dissociation of the P waves due to AV block, and probably AIVR, which would be even more suggestive of compromise of the inferior wall.