Intra-aortic Balloon Pump
aka Cardiovascular Curveball 005
One of your patients is a 58 year-old man who had a quadruple coronary artery bypass earlier in the day. He had poor cardiac output after the procedure and required the insertion of an intra-aortic balloon pump (IABP) to augment his cardiac function.
The medical students have a few questions for you concerning IABPs. Can you answer them?
Q1. What is an intra-aortic balloon pump (IABP). How does it work as a circulatory assist device?
Answer and interpretation
The IABP has two parts:
- a large bore catheter with a long sausage-shaped balloon at the distal tip, and
- a console containing a pump that inflates the balloon
The balloon is designed to sit in the proximal descending aorta. It comes in various lengths according to body height, with balloon volumes of about 30-50 mL. The balloon is usually filled with helium gas, and when inflated should fill up 80-90% of the aortic diameter.
The IABP works by inflating and deflating at different phases of the cardiac cycle.
- Balloon inflation augments diastolic blood pressure
- Balloon deflation decreases afterload during systole.
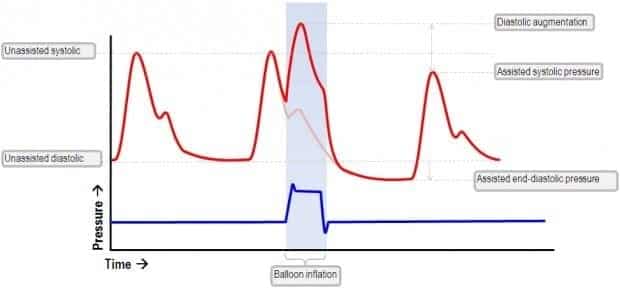
Balloon inflation in early diastole (usually triggered by the R wave on the ECG) increases diastolic blood pressure.
- This in turn increases systemic perfusion and coronary perfusion (at least in the hypotensive patient).
- Balloon inflation thus displaces blood both proximally and distally.
- The increase in coronary perfusion increases myocardial oxygen supply.
Balloon deflation occurs at the end of diastole resulting in a decreased end diastolic blood pressure.
- This reduces the aortic pressure at the start of systolic ejection, thus decreasing the afterload that the heart has to pump against.
- This decreases myocardial oxygen demand and improves systemic perfusion during systole.
This animation may help in visualising how the IABP works (bear with the funky accent! – you may need to increase the volume):
Q2. What are the indications for IABP use?
Answer and interpretation
The IABP can be used whenever there is cardiac pump failure if:
- it may resolve spontaneously, or
- a corrective procedure is planned.
In other words, there has to be some hope of the patient being able to survive without an IABP in the future.
Some situations where an IABP is used include:
- Cardiogenic shock after coronary artery bypass grafting (CABG) or acute myocardial infarction
- unstable angina
- Acute mitral incompetence
- Planned cardiac transplant
- ventricular arrhythmias refractory to conventional treatment
- cardiotoxicity from poisoning, e.g. verapamil overdose
Q3. How is an IABP inserted and positioned?
Answer and interpretation
Explanation 1:
- IABPs are usually inserted using the Seldinger technique via the femoral artery so that the tip of the catheter is advanced proximally into the aorta.
- Fluoroscopy is not essential for insertion, so an IABP can be placed emergently.
- IABP’s must be appropriately positioned:
- The balloon tip is positioned just distal to the origin of the left subclavian artery, and the entire balloon should lie above the renal arteries.
Explanation 2:
A more detailed description of IABP insertion as described by Charles Gommersall:
- heparinise patient prior to insertion of catheter providing there are no contraindications such as recent surgery.
- prep skin
- fully collapse balloon applying 30 ml vacuum with 60 ml syringe
- insert needle into femoral artery at 45° and pass it through both walls of artery. Withdraw needle until strong pulsatile jet of blood is obtained
- pass guidewire through needle and advance until tip is is in thoracic aorta. Wire should pass very easily
- pass sheath over wire in similar manner to insertion of PA catheter sheath
- pass balloon over guidewire through sheath. Must be inserted to at least the level of the manufacturer’s mark (usually double line) to ensure that entire balloon has emerged from sheath
- balloon should be positioned so that the tip is about 1 cm distal to the origin of the left subclavian artery. If fluroscopy is not available during insertion the distance from the angle of Louis down to the umbilicus and then to the femoral artery insertion site should be measured to approximate the distance the balloon should be advanced and the position should be checked on CXR
- remove wire. Return of blood via central lumen confirms that the tip is not subintimal and has not caused a dissection.
- flush central lumen with heparin saline and connect to transducer to monitor intra-aortic pressure (the outer lumen transmits helium gas to the balloon)
- monitor Doppler ankle pressures and compare with preinsertion value
Note: once the balloon has been inflated, even if it is then deflated, it must not be removed through the sheath for any reason – the sheath must be removed first.
Q4. When is an IABP contra-indicated?
Answer and interpretation
Contra-indications include:
- Aortic insufficiency
- Aortic dissection
- Patent ductus arteriosus
- Severe peripheral vascular disease
- Thoracic aortic graft <12 months old
- the patient’s cardiac index is too low for there to be a clinical benefit from IABP assistance
Q5. What are the determinants of IABP efficiency?
Answer and interpretation
IABP efficiency is determined by:
- Timing of balloon inflation and deflation
- Assist ratio (e.g. 1:1 – balloon inflation and deflation on every cardiac cycle – provides greater circulatory assistance than 1:2 or 1:4 – balloon inflation and deflation on every 2nd or 4th cardiac cycle )
- Heart rate (efficiency is greatly decreased at heart rates >130/min)
- Gas loss from balloon (balloon volume)
- Minimum cardiac index of 1.2 – 1.4 L/min/m2 is required for IABP assistance to be clinically beneficial
Q6. How can IABP function be optimised?
Answer and interpretation
Optimisation can be achieved by ensuring that:
- inflation of the balloon occurs at the dicrotic notch (forming the sharp ‘V’)
- the slope of rise of augmented diastolic waveform is straight and parallel to the systolic upstroke
- the augmented DBP at balloon deflation exceeds or is equal to end-systolic BP
- the end-diastolic BP at balloon deflation is lower than the preceding unassisted end-DBP by 15-20 mmHg
- the assisted SBP (following a cycle of balloon inflation) is lower than the previous unassisted SBP by 5 mmHg
Q7. What are the complications of IABPs?
Answer and interpretation
Complications can occur during insertion, while the IABP is in use, during removal, or after removal.
During INSERTION
- failure to advance catheter beyond iliofemoral system because of atherosclerotic disease (common)
- aortic dissection and arterial perforation – may cause retroperitoneal haemorrhage.
During USE
Ischemia
- ischemia of the lower limbs (up to 25% of all IABP patients)
- may occur while the IABP is in place, or hours after removal due to thromboembolic showers
- ischemia usually results from thrombosis at the insertion site
- Can affect contra-lateral leg due due to cholesterol emboli and thromboembolic showers from the balloon
- Close neurovascular monitoring essential – sensorimotor loss generally mandates removal
- Pulseless limb may need to be tolerated if IABP is life-saving
- Visceral ischemia
- Spinal ischemia
Balloon rupture causing helium embolus
- this may be heralded by high balloon inflation pressures.
- The key indicator of balloon rupture is the presence of blood in the connecting tubing.
- Management involves immediate cessation of counterpulsation, placement of the patient head down and IAB removal.
- Consider giving broad spectrum antibiotics as the gas chamber of the balloon is not sterile.
Small perforation in balloon membrane
- this may allow a small amount of blood to leak into balloon lumen.
- The blood is dessicated by the dry helium and forms a hard pellet which may stop the balloon from being removed without surgical aortotomy.
Haemolysis and consumptive thrombocytopenia
Peripheral neuropathy
Catheter-related infection
During or after REMOVAL:
- Haematoma
- Pseudoaneurysm
- AV fistula
- Entrapment of the IABP
If this was a walk in the park, try Cardiovascular Curveball 007 for more IABP problem-solving.
References
- Overwalder PJ. Intra Aortic Balloon Pump (IABP) Counterpulsation. The Internet Journal of Perfusionists. 2000;1:(1) (fulltext online) [Scenarios 1-4 are based on a figure from this article]
- Marino’s The Little ICU Book
- Krishna M, Zacharowski K. Principles of Intra-Aortic Balloon Pump Counterpulsation. Cont Edu Anaesth Crit Care & Pain. 2009;9(1):24-28. [Reference]
- Datascope’s IABP elearning modules
- Gomersall C. Intra-aortic balloon pumping. 1999.
- LITFL CCC — Intra-Aortic Balloon Pump
- The IABP waveforms in each of the scenarios were drawn using the open-source vector graphics editor Inkscape.
CLINICAL CASES
Cardiovascular Curveball
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
