Aslanger Pattern: Another OMI?
13.3% of inferior MIs may present with Aslanger Pattern, and due to being incorrectly labelled as an NSTEMI, be deprived of emergent revascularisation therapy
Aslanger 2020
In April 2020, Aslanger et al identified a specific ECG pattern concerning for acute inferior occlusion MI (OMI) in patients with concomitant multi-vessel disease, that does not display contiguous ST-segment elevation or fulfil STEMI criteria. The publishers reviewed ECG and angiography findings from 1000 NSTEMI, 1000 control (no myocardial infarction), as well as inferior STEMI patients presenting during the same time period. The Aslanger Pattern was observed in 6.3% of NSTEMI patients and found to be a predictor of larger infarct size and higher mortality.
ECG Criteria
1) Inferior STE isolated to lead III
2) Concomitant ST depression in any of V4-V6, with a positive/terminally positive T-wave
3) ST segment in V1 > V2
(1) STE in III but not in any other inferior lead,
(2) ST depression in any of leads V4 to 6 (but not in V2) with a positive (at least terminally positive) T-wave,
(3) ST in lead V1 higher than ST in V2.
Why is there not contiguous ST elevation?
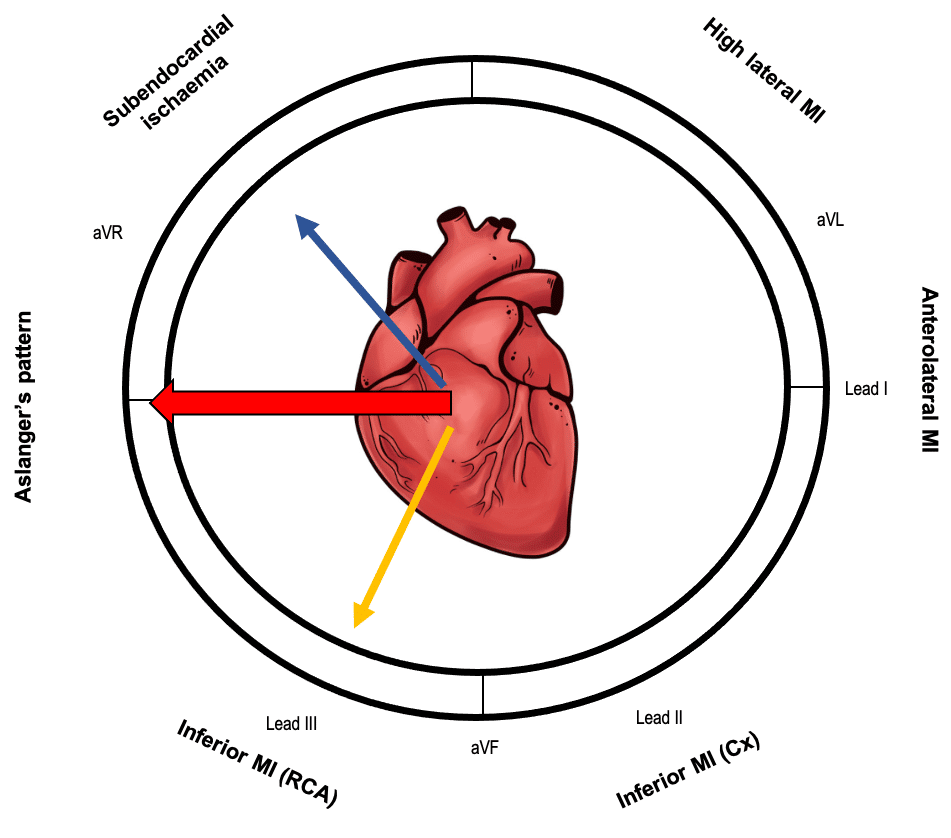
- In cases of limited inferior wall injury, the ST vector of inferior MI localises the area of infarction and is typically directed inferiorly and rightwards (yellow arrow)
- The ST vector of subendocardial ischaemia does not localise to the ischaemia and regardless of involved coronary region directs to lead aVR (blue arrow)
- The resultant average ST vector directs rightwards, causing ST elevation only in lead III and aVR
Clinical significance
- Concurrent multi-vessel disease predisposes these patients to poor outcomes if there is delayed time to emergent reperfusion, and prompt recognition of this potential OMI should improve outcomes
- Identification of the culprit lesion at the time of angiography may be difficult if there is multiple critical stenoses, and this pattern would guide lesions supplying the inferior wall to be opened first
Limitations
- The pattern was found to be present in 0.5% of patients without acute MI, which may be a result of chronic change from a previous ischaemic insult
- Acute inferior MI in the presence of previous infarctions may also change the overall orientation of the lesion vector causing a similiar pattern
- This is an isolated, retrospective study and warrants a further analysis as a predictor of occlusion MI that would be responsive to emergent reperfusion therapy
Associated Persons
- Emre Aslanger; Yeditepe University Hospital, Department of Cardiology, Istanbul, Turkey
Further Examples
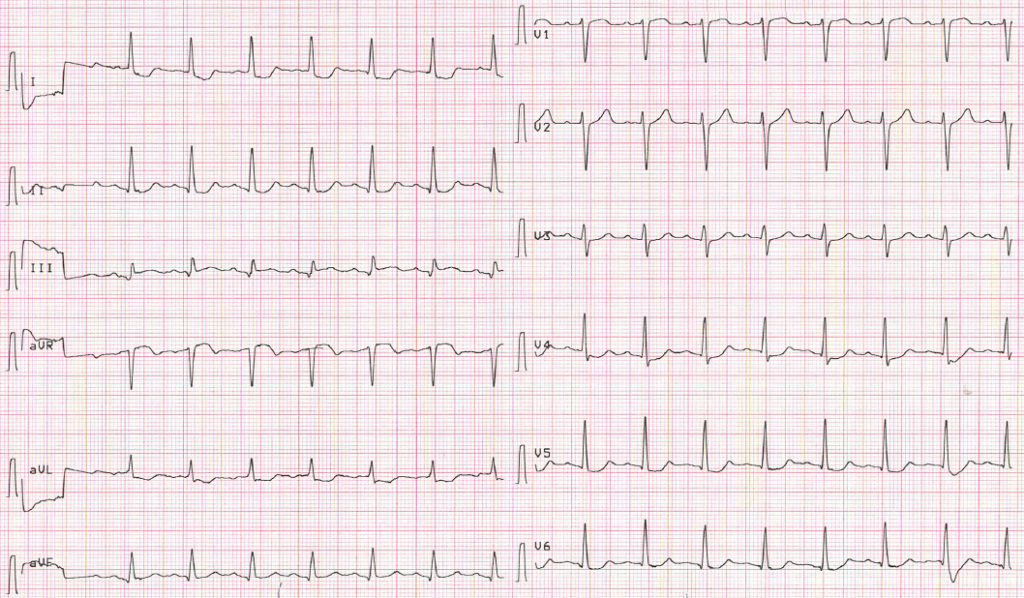
Example 1
57 yo female, without previous heart disease except hypertension, presents with chest pain.
References
Historical references
- Aslanger E, Yıldırımtürk Ö, Şimşek B, Sungur A, Türer Cabbar A, Bozbeyoğlu E, Karabay CY, Smith SW, Değertekin M. A new electrocardiographic pattern indicating inferior myocardial infarction. J Electrocardiol. 2020 Jul-Aug;61:41-46.
- Aslanger EK, Smith SW. Response to: “A new electrocardiographic pattern indicating inferior myocardial infarction”. J Electrocardiol. 2020 Nov 18
Eponymous term review
- Fiol M, Carrillo A, Cygankiewicz I, Velasco J, Riera M, Bayés-Genis A, Gómez A, Peral V, Bethencourt A, Goldwasser D, Molina F, Bayés de Luna A. A new electrocardiographic algorithm to locate the occlusion in left anterior descending coronary artery. Clin Cardiol. 2009 Nov;32(11):E1-6
- Bozbeyoğlu E, Aslanger E, Yıldırımtürk Ö, Şimşek B, Hünük B, Karabay CY, Kozan Ö, Değertekin M. The established electrocardiographic classification of anterior wall myocardial infarction misguides clinicians in terms of infarct location, extent and prognosis. Ann Noninvasive Electrocardiol. 2019 May;24(3):e12628
- Turgay Yildirim Ö, Çanakçı ME. The new ECG pattern for inferior myocardial infarction. J Electrocardiol. 2020 Nov-Dec;63:64
- Smith SW. Subtle ECG Findings of Left Anterior Descending Artery (LAD) Occlusion — LAD Occlusion MI (OMI). Vimeo 2020
- Smith SW. A 58 year old collapses in the hot sun Dr Smith’s ECG Blog 2020
- Smith SW. ECG with Aslanger’s Pattern. CT Pulmonary Angiogram Reveals LAD Ischemia (Septal Transmural). But this is not Contradictory. Dr Smith’s ECG Blog 2021
- Buttner R. OMI: Replacing the STEMI misnomer. LITFL 2021
ECG LIBRARY
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner



I’d be interested to know from someone who is better than me at this how right sided precordial leads would be expected to perform in terms of picking up STE in this scenario.
Maybe, because ST vector changes its direction not only in frontal space (becoming nearly parallel to III lead’s positive pole), but also in horizontal one, so that it sits on V1 lead’s positive pole more than that of V2 lead.
DOI: 10.1016/j.jelectrocard.2023.07.009
[…] Aslanger Pattern OMI […]
Both of those examples have subtle reciprocal change in aVL. As leads III and aVL are electrically opposite, they are often the most useful leads in detecting reciprocal change. It is always worth scrutinising aVL for subtle ST depression or T wave inversion when STE is detected in lead III, and vice versa.