Appendagitis
aka Gastrointestinal Gutwrencher 001
A 50 year-old man presented to the ED with sharp abdominal pain localised to his left lower quadrant.
The pain came on rapidly the day before, when he took his dog for a walk after dinner. The pain is non-radiating and worse on movement, but he has no other symptoms. Past medical history is unremarkable. His vitals were within normal limits, his abdomen was soft with no herniae or scrotal abnormalities, but he was distinctly tender in the left lower quadrant.
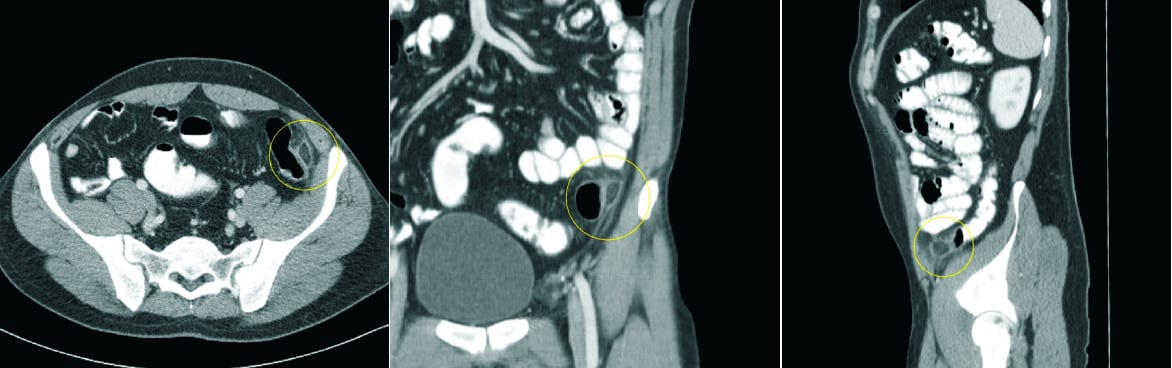
FBC, UEC and urinalysis were within normal limits. Following a surgical review, a CRP was ordered and the following CT abdomen was obtained:
Questions
Q1. What is the diagnosis?
Answer and interpretation
Epiploic appendagitis
Q2. How common is this condition?
Answer and interpretation
The diagnosis is rare.
This is partly because of low awareness of its existence among clinicians.
It can affect any age (mean ~45 years) and has a male preponderance. It is unclear if it is more common in the obese.
Q3. What causes this condition?
Answer and interpretation
Epiploic appendages are the 50–100 fatty blobs that originate in two rows (anterior and posterior) either side of the taenia coli. They are 0.5 to 5 cm long and each is accompanied by one or two arterioles and a venule.
They may become inflamed as a result of torsion or spontaneous venous thrombosis.
Epiploic appendagitis most commonly affects the sigmoid, but also occurs in the cecum and other regions of the colon. However, patients with long sigmoids can have right-sided rather than left-sided pain.
Q4. What are the clinical features of this condition?
Answer and interpretation
Abdominal pain and tenderness with the following characteristics:
- More commonly LLQ than RLQ
- localized, strong, non-migratory, sharp pain
- usually starts after physical movement e.g. postprandial exercise
There is a lack of systemic features (e.g. fever, vomiting or leukocytic response), although CRP may be elevated.
Q5. What is the best way to make the diagnosis?
Answer and interpretation
CT abdomen is the most reliable way of making the diagnosis, short of laparoscopic exploration. Epiploic appendages are not usually seen on CT due to fat attenuation, unless they are surrounded by intraperitoneal fluid or inflammation.
The pathognomonic CT scan finding for epiploic appendagitis is the presence of a 2–4 cm, oval shaped, fat density lesion, surrounded by inflammatory changes.
The key features are:
- Central focal area of hyper-attenuation with surrounding inflammation
- ± Thickening of the parietal peritoneum wall
- Diameter of the colonic wall is mostly regular without signs of thickening (unlike diverticulitis)
Epiploic appendagitis can be diagnosed on ultrasound but this modality has low sensitivity.
Investigations are generally targeted at excluding the serious conditions that epiploic appendagitis may mimic – especially appendicitis and diverticulitis.
Q6. How should this patient be managed?
Answer and interpretation
This is somewhat controversial.
Epiploic appendagitis is generally considered a benign and self-limiting condition. Patients recover in <10 days and usually require only oral analgesia (e.g. paracetamol, NSAIDs)
However, the rate of recurrence – with pain localised to the same region – may be up to 40%. Some authorities suggest that surgical intervention may decrease this. The suggested approach is surgical exploration using laparoscopy, with simple ligation and excision of the inflamed appendage.
References
- Sand, M., Gelos, M., Bechara, F., Sand, D., Wiese, T., Steinstraesser, L., & Mann, B. (2007). Epiploic appendagitis – clinical characteristics of an uncommon surgical diagnosis. BMC Surgery, 7:11 DOI: 10.1186/1471-2482-7-11
CLINICAL CASES
Gastrointestinal Gutwrencher
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
