Bullet in the Head
aka Neurological Mind-boggler 009
A middle-aged man presents having been shot in the head and arm:



Questions
Q1. What are the initial principles of management?
Answer and interpretation
The principles of EMST/ ATLS apply; taking part in these courses is highly recommended if you are involved in this area at all.
Initial management is focused on preventing secondary brain injury by preventing hypoxia and hypotension, which have been shown in the context of TBI to be the most important variables affecting outcome.
- Hypotension alone increases mortality in severe TBI from 27% to 60%.
- Hypoxia, in addition to hypotension, is associated with a mortality of 75%.
In the context of trauma, the principles of ATLS are followed, with a primary survey focusing on airway patency and C-Spine protection, adequate ventilation with oxygenation and addressing life threatening haemorrhage. In this case, preventing haemorrhage from the arm injury is crucial to prevent hypovolaemic shock and reduced cerebral perfusion pressure.
This is followed by the appropriate adjuncts and a complete secondary survey. Associated injuries that might result in hypotension or hypoxia must be identified early.
Evaluation for occult injuries is routine, e.g. CT of the abdomen, FAST, DPL, and chest x-ray.
Urgent CT scan, frequent neurologic revaluations, and repeat CT scans are used to identify progressive injuries.
Q2. What are the specific considerations for airway management in this case?
Answer and interpretation
Endotracheal intubation with rapid sequence induction is required for airway protection if the GCS is </=8 or if it falls by >/=2 points.
Intubation may also be required for other reasons, e.g. coexistent respiratory problem or prior to operative intervention.
During intubation it is critical to avoid further elevations in ICP (EICP). This may be exacerbated by hypoxia, hypotension and drugs or various manoeuvres. To avoid this, consider the following measures:
- Experienced airway doctor
- Full preparation for difficult intubation available
- Adequate preoxygenation
- Judicious use of sedative agents (being mindful of blood pressure and ICP)
- Fluids and vasopressors e.g. metaraminol available
After initial resuscitation the patient is taken to the operating theatre; he returns to the neuro-intensive care after a decompresive craniectomy and insertion of several monitoring devices.
Q3. What is this device?
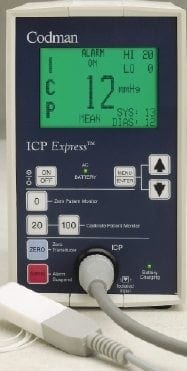
Answer and interpretation
A Codman ICP monitor, used intraparenchymally in this instance.
Q4. What are the pros and cons of different intracranial pressure (ICP) monitors?
Answer and interpretation

Q5. What does this monitor show? What is it used for in the ICU setting?

Answer and interpretation
Trans-cranial doppler
Trans-cranial doppler is a big topic in its own right (see references) and was only used as a component of research in this case.
Trans-cranial doppler is used in the ICU to:
- Detect vasospasm post SAH in unconscious patients
- Predict onset of delayed ischaemic neurological deficit
- Non-invasively estimate ICP after traumatic brain injury (TBI)
- Detect vasospasm post TBI
- Assess cerebrovascular autoregualtion
- Test for brain death (not on its own however)
Q6. What is this bit of kit? How useful is it?

Answer and interpretation
NIRS: Near-infrared spectroscopy.
NIRS is a non-invasive monitor of cerebral oxygenation. It is attracting a lot of interest currently but remains to be validated for use in guiding therapy or inferring prognosis in TBI (see references).
Q7. And what is this? It is inserted through the same bolt as the ICP monitor and the blue box shown below. What are the components shown? What does the device tell you?

Answer and interpretation
It is a cerebral microdialysis catheter
The components of the cerebral microdialysis (MD) catheter are:
- pump connector
- inlet tube
- MD catheter
- MD membrane
- outlet tube
- microvial holder
- microvial for collection of microdialysate
Cerebral microdialysis is a well-established laboratory tool that is increasingly used as a bedside monitor to provide on-line analysis of brain tissue biochemistry during neurointensive care. Microdialysis has the potential to become an established part of mainstream multi-modalitymonitoring during the management of acute brain injury but at present is a research tool for use in specialist centres.
A recent review by Tisdall and Smith (2006) describes the principles of cerebral microdialysis and the rationale for its use in the clinical setting, including discussion of the most commonly used microdialysis biomarkers of acute braininjury, with potential clinical applications and future potential research applications (see references).
Q8. Here is even more multi-modal monitoring. What is it? Is it more or less useful than the rest of the devices we’ve seen?

Answer and interpretation
PbO2 monitor (it measures brain tissue oxygenation)
The prevention and aggressive treatment of cerebral hypo-oxygenation and control of ICP with a PbtO(2)-directed protocol has been shown to reduced the mortality rate after TBI in major trauma, and result in improved clinical outcomes over the standard ICP/CPP-directed therapy. This was shown in two single centre studies with historically matched controls, which have inherent limitations (see references: Narotam et al 2009; Spiotta et al 2010).
However, as there have been no randomized controlled trials carried out to determine whether PbtO2 monitoring results in improved outcome after severe TBI, use of this technology has not so far been widely adopted in neurosurgical intensive care units.
A study is about to commence (see the details here at www.clinicaltrials.gov — it will be the first randomized, controlled clinical trial of PbtO2 monitoring, and is designed to obtain the data required for a definitive phase III study, such as efficacy of physiologic maneuvers aimed at treating PbtO2, and feasibility of standardizing a complex intensive care unit management protocol across multiple clinical sites:
Patients with severe TBI will be monitored with ICP monitoring and PbtO2 monitoring, and will be randomized to therapy based on ICP along (control group) or therapy based on ICP in addition to PbtO2 values (treatment group). 182 participants will be enrolled at four clinical sites in the United States. Functional outcome will be assessed at 6-months after injury.
Q9. What other complications might you expect following this event?
Answer and interpretation
Complications include:
- Poor neurological recovery
- Head wound infection (from shardes of bone/debris suckied in by the bullet)
- Arm wound infection
- Meningitis
- Line sepsis
- Ventialtor associated pneumonia
- Neurogenic cardiomyopathy
- All the other complications of a prolonged ICU admission!
References
Good reviews of different aspects of penetrating brain injury were compiled in a supplement of The Journal of Trauma in 2001, here are the references:
- Antibiotic prophylaxis for penetrating brain injury. J Trauma. 2001 Aug;51(2 Suppl):S34-40. Review. PMID: 11505198
- Surgical management of penetrating brain injury. J Trauma. 2001 Aug;51(2 Suppl):S16-25. Review. PMID: 11505195.
- Antiseizure prophylaxis for penetrating brain injury. J Trauma. 2001 Aug;51(2 Suppl):S41-3. Review. PMID: 11505199.
- Vascular complications of penetrating brain injury. J Trauma. 2001 Aug;51(2 Suppl):S26-8. Review. PMID: 11505196.
- Management of cerebrospinal fluid leaks. J Trauma. 2001 Aug;51(2 Suppl):S29-33. Review. PubMed PMID: 11505197.
Transcranial doppler:
- White H, Venkatesh B. Applications of transcranial Doppler in the ICU: a review. Intensive Care Med 2006 Jul;32(7):981-94. Epub 2006 May 10. Review. PMID: 16791661.
Near-infrared spectroscopy:
- Highton D, Elwell C, Smith M. Noninvasive cerebral oximetry: is there light at the end of the tunnel? Curr Opin Anaesthesiol. 2010 Oct;23(5):576-81. PMID: 20830845
Cerebral microdialysis:
- Tisdall MM, Smith M. Cerebral microdialysis: research technique or clinical tool. Br J Anaesth. 2006 Jul;97(1):18-25. PMID: 16698861
Brain tissue oxygen monitoring:
- Narotam PK, Morrison JF, Nathoo N. Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy. J Neurosurg. 2009 Oct;111(4):672-82. PMID: 19463048
- Spiotta AM, Stiefel MF, Gracias VH, Garuffe AM, Kofke WA, Maloney-Wilensky E, Troxel AB, Levine JM, Le Roux PD. Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg. 2010 Sep;113(3):571-80. PMID: 20415526
Neurological Mind-boggler
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
