Does Roc rock? Does Sux suck?
aka Ruling the Resus Room 004
On the plus side, the patient who took the olanzepine overdose before being delivered to Resus bay 4 is no longer trying to kick and punch the nursing staff. On the minus side, he is descending into a deep coma and is no longer protecting his airway. You decide to perform rapid sequence intubation (RSI) and thus, with meticulous supportive care, ensure his survival… After all, you want to make sure he lives to fight another day.
But what neuromuscular blocker are you going to use? Rocuronium or suxamethonium (aka succinylcholine)?
Questions
Q1. How do roc and sux cause muscle relaxation/ paralysis?
Answer and interpretation
Both roc and sux bind to nicotinic aceytlcholine receptors at the neuromuscular junction, thus preventing motor neurones from triggering action potentials in skeletal muscle.
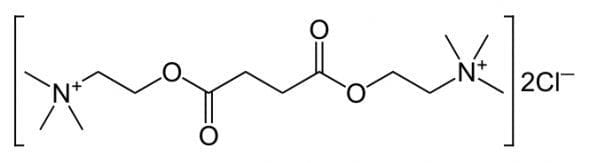
Suxamethonium is really just two acetylcholine molecules stuck together. It acts as a depolarising muscle relaxant — hence fasciculations occur prior to muscle relaxation.
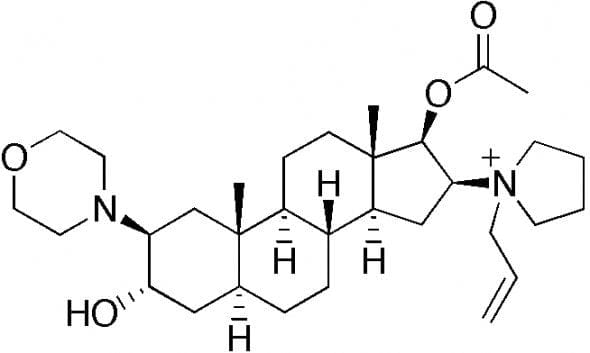
Rocuronium is an analogue of vecuronium, an aminosteroid. It acts as a non-depolarising muscle relaxant.
Q2. How are roc and sux metabolised?
Answer and interpretation
Sux is rapidly hydrolysed thanks to the action of plasma and liver pseudocholinesterases (but not in patients susceptible to suxamethonium apnoea, which occurs in people with rare variations of the pseudocholinesterase gene).
Roc on the other hand, undergoes hepatic/ biliary and urinary excretion, so it is eliminated much more slowly than sux.
Q3. How are roc and sux administered, and in what doses?
Answer and interpretation
Sux is typically given at a dose of 1 to 1.5mg/kg IV. In infants a higher dose of 1.5-2mg/kg is often used. It can also be given IM, but at a higher dose (e.g. double it). Sensitivity to suxamethonium is increased during pregnancy, and some advise decreasing the dose by about 25% (I doubt this is very significant clinically).
The dose of roc used in RSI varies from 0.6 to 1.2 mg/kg IV. I suggest using 1.2 mg/kg IV (or more), as I’ll explain in Q4.
Q4. How rapid is the onset of paralysis with sux and roc?
Answer and interpretation
Except in patients with poor perfusion states, good intubating conditions are typically achieved after 45 to 60 seconds with suxamethonium. Proponents of sux cite this as a major advantage over roc.
Traditionally roc is considered to have a slower onset of action than sux. Indeed, this is true if you use lower doses like 0.6 to 0.9 mg/kg IV. However, if a dose of 1.2 mg/kg IV is used there is no difference between roc and sux in the onset of good intubating conditions.
Q5. How long does paralysis last for with sux and roc?
Answer and interpretation
There is no doubt that roc renders patients paralysed for much longer than sux. Optimal intubating conditions probably last about 5 minutes after giving an RSI dose of sux, although time to complete recovery is more like 10 minutes.
Like the onset, the duration of effect for rocuronium depends on the dose administered. Recovery may occur as early as 30 minutes following a dose of 0.6 mg/kg IV, but will be more like 90 minutes following a dose of 1.2 mg/kg.
Sux proponents typically highlight this difference as a major advantage of sux — you’d only have to bag for 10 minutes and then the patient can be woken up and allowed to breathe spontaneously. This isn’t quite how things work in the resus room though…
If you are performing RSI on a patient and it is feasible to wake them up if things go haywire, then you probably shouldn’t have been doing the RSI in the first place!
In the resus room, if you’re performing RSI and can’t get the tube in first try, then you better turn to Plans B, C, and D, etc. until you find a way to get some sort of airway — even if this means you need to cut the patient’s throat because you’re in a CICVBCO (can’t intubate, can’t ventilate, but can oxygenate) situation. In the resus room RSI, keeping the patient paralysed is an advantage: while you frantically work your way through your back up plans the last thing you need is the patient fighting your attempts at ventilation or pushing your scalpel-wielding hand away in the midst of a hypoxic spiral into the abyss…
Remember to use apneic oxygenation and the other tips shown in the videos featured in Own the Airway!
Anyway, roc can now be reversed in about 2.2 minutes. That’s how long it takes for a 16 mg/kg IV dose of sugammadex to achieve reversal of rocuronium-induced muscle relaxation. However, like I just said, if you’ve planned things right you won’t want to do this….
Q6. What are the side effects of roc and sux?
Answer and interpretation
Let’s start with roc as it’s easy — none!
(OK, I’m exaggerating… Allergy is always a risk, but there’s nothing else significant I can think of)
Suxamethonium, on the other hand, can cause:
- bradycardia, potentially leading to cardiac arrest (especially in small children and following repeat doses)
- hyperkalemia, which is potentially fatal (though K only rises about 0.4 mmol/L on average in normal individuals)
- fasciculations which increase oxygen consumption and lead to muscle pain
- increases in:
- intra-gastric pressure, possibly offset by an increase in lower esophageal sphincter tone
- intracranial pressure
- intraocular pressure
- malignant hyperthermia — rare, but very very bad
- suxamethonium apnoea — rare, and not likely to be a major concern in the resus room.
So, no contest here…
Q7. What are the contra-indications to roc and sux?
Answer and interpretation
Again, it’s easier to start with roc — contra-indications… roc allergy, anything else?
The use of sux should be avoided if the following conditions are present:
- hyperkalemia
- risk of hyperkalemia(occurs in many of these conditions because of proliferation of acetylecholine receptors beyond the normal neuromuscular junctions)
- renal failure (a relative CI)
- severe sepsis
- congenital myopathies
- neuromuscular disorders such as tetanus and botulism
- upper motor neuron disorders: stroke >72h, motor neuron disease, mutliple sclerosis, spinal cord injury >72h
- burns > 72h
- crush injury
- malignant hyperthermia
- suxamethonium apnoea
Most of these conditions are seen rarely in the resus room, so widespread use of sux is rarely going to cause problems. However, it will happen to someone… It is not always possible to exclude all of these conditions prior to rapid sequence intubation in the resus setting.
Q8. How do sux and roc compare in terms of ‘safe apnoea times’?
Answer and interpretation
The ‘safe apnoea time‘ is how long a patient can remain apnoeic for before developing hypoxemia.
Rocuronium appears to have longer safe apnoea times than suxamethonium. For instance, in ASA grade 1 or 2 patients with BMIs of 25 to 30 receiving general anesthetic, patients who were given rocuronium took 40 seconds longer to fall to an SO2 of 93% when apneic than those who received suxamethonium. This might be a result of increased oxygen consumption from the fasciculations caused by depolarising neuromuscular blockade.
Q9. How do roc and sux compare in terms of cost and storage time?
Answer and interpretation
A 50mg/5mL amp of roc costs about 10 times as much as a 100mg/2 mL amp of sux. A difference of about $20… Absolute peanuts in the context of a critically ill patient.
Roc can be stored safely at room temperature for about 12 weeks, six times longer than sux (stable at room temperature for 14 days).
Well, you answered all the hard questions… So, do you think roc rocks and sux sucks, or vice versa? Which are you going to use next time you perform rapid sequence intubation? I’m with Reuben Strayer on this one
References
- El-Orbany M, Connolly LA. Rapid sequence induction and intubation: current controversy. Anesth Analg. 2010 May 1;110(5):1318-25. Epub 2010 Mar 17. Review. PMID: 20237045.
- Mallon WK, Keim SM, Shoenberger JM, Walls RM. Rocuronium vs. succinylcholine in the emergency department: a critical appraisal. J Emerg Med. 2009 Aug;37(2):183-8. Epub 2008 Dec 20. Review. PMID: 19097730.
- Perry JJ, Lee JS, Sillberg VA, Wells GA. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev. 2008 Apr 16;(2):CD002788. Review. PMID: 18425883. [read the last line of the results section of the abstract carefully, as it explains the conclusion]
- Reid C. Less RSI desaturation with Roc Resus.ME
- Reid C. Longer apnoea time with roc in the obese too Resus.ME
- Reid C. More on Rocuronium (and Sugammadex) Resus.ME
- Strayer, R. EM Updates. Screencast: Rocuronium vs. Succinylcholine in 8 minutes

CLINICAL CASES
Resus Room Reflection
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

one thing you neglect to mention when discussing pros and cons: paralyzing your patient for 90 minutes with an RSI dose of roc has distinct disadvantages in terms of your ability to clinically reassess critically ill patients post-intubation. You can’t assess if they are seizing or if they are developing lateralizing neurologic deficits. You can’t assess for peritonitic signs / abdominal rigidity. You can’t as easily assess for increasing pain/discomfort at all. To me, this seems like a pretty pertinent downside to just paralyzing all critically ill patients for 90 minutes just to avoid a few rare side effects of a medication that only paralyzes for 10 minutes.
Good points Matthew. I agree that there is a clear role for suxamethonium in the right contexts – especially if early/ ongoing clinical neurological assessment is needed.
For context this post was written over a decade ago (the date at the top doesn’t reflect the original publication date) with the intention of being deliberately provocative in a climate where rocuronium was used infrequently.
The question “When should you use sux?” prob needs to be added at the end!
Thanks for the comment.
Love this article, Chris! Every point you make is a valid. It feels like you have recorded countless discussions I have had with registrars, even down to the point of that once-in-a-career CICO. I can’t imagine having the presence of mind, spiralling down the VORTEX to think: “Hmmm, probably should give some Roc before the sux wears off.”