Echo basics: Aortic Regurgitation
Understand and identify aortic regurgitation. Learn how to identify and grade aortic regurgitation gradient using measurements and visual clues and quantify aortic regurgitation.
Identifying and Grading Aortic Regurgitation
Causes of Aortic Regurgitation
Aortic regurgitation (AR) is always pathological and results from abnormalities of the aortic valve or root. Common causes include:
- Congenital or degenerative causes:
- Bicuspid aortic valve
- Calcific degeneration
- Marfan’s syndrome
- Inflammatory or infectious causes:
- Rheumatic heart disease
- Infective endocarditis
- Acute etiologies:
- Aortic dissection
- Trauma
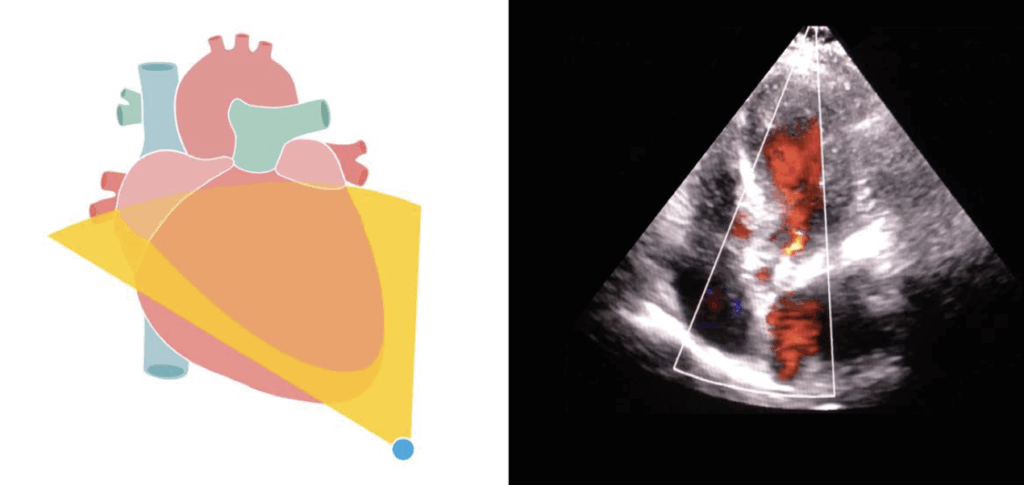
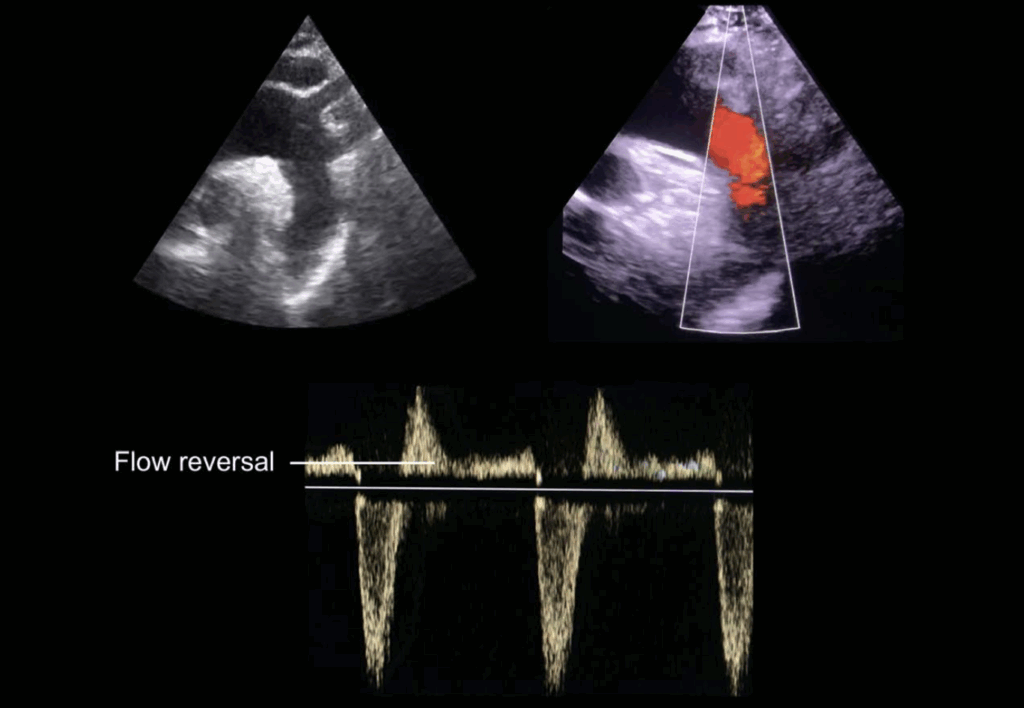
Colour Doppler Assessment
Colour Doppler is the primary tool to confirm AR. Hallmarks include:
- Retrograde blood flow through the aortic valve into the LVOT during diastole
- Apical views: Best for visualizing the jet (typically red/orange)
- Parasternal long- and short-axis views: Best for identifying jet origin
⚠️ Jet length is not a reliable indicator of severity
Grading Aortic Regurgitation by Jet Width
Use the jet width-to-LVOT width ratio (parasternal long-axis view):
- < 25% of LVOT width → Mild AR
- 25–65% of LVOT width → Moderate AR
- > 65% of LVOT width → Severe AR
Use colour M-mode across the outflow tract for improved clarity.
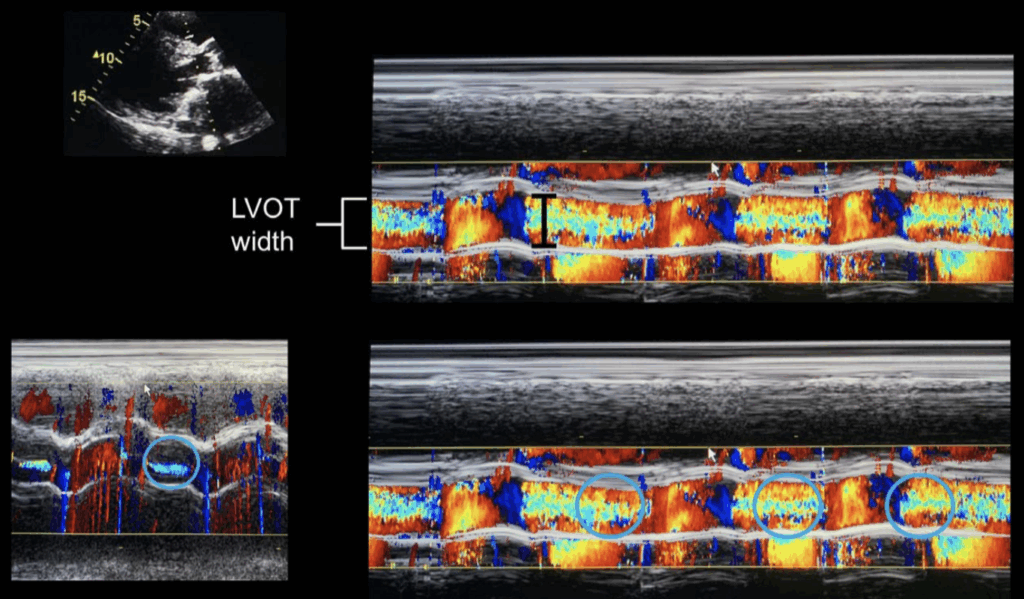
Vena Contracta Measurement
Vena contracta = narrowest portion of the colour jet.
- Measured in parasternal long-axis view, ideally with zoom
- < 3 mm → Mild AR
- > 6 mm → Severe AR
- 3–6 mm → Moderate AR
✅ This method remains valid for eccentric jets.
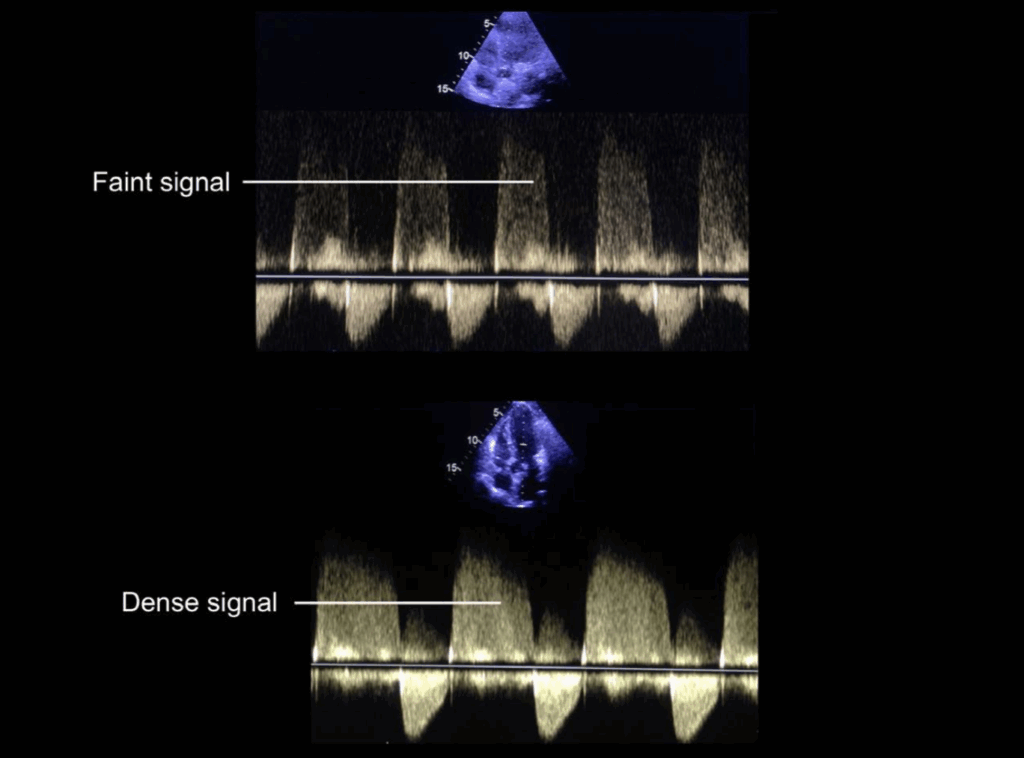
Continuous Wave Doppler Assessment
Best from the apical five-chamber view.
- A dense Doppler signal suggests more severe regurgitation
- A faint, incomplete signal suggests mild regurgitation
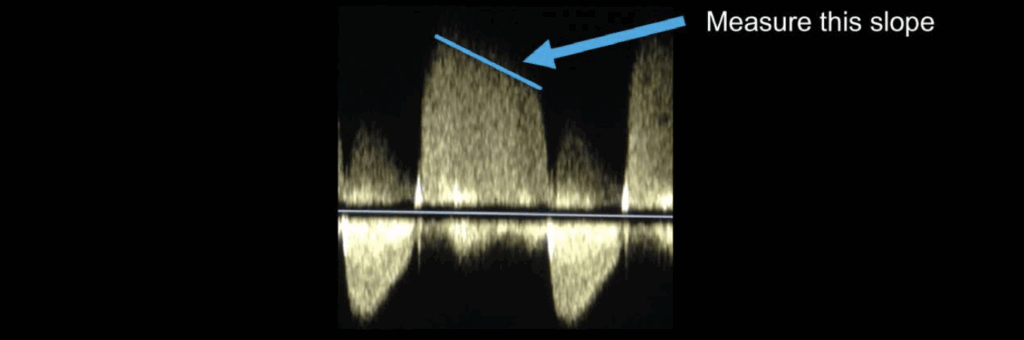
Pressure Half-Time (PHT)
Derived from the slope of the AR jet on CW Doppler:
- < 200 ms → Severe AR (rapid pressure equalization)
- 200–500 ms → Moderate AR
- > 500 ms → Mild AR
❗Requires a full, well-defined spectral Doppler envelope
Using Visual Clues to Help Grade Aortic Regurgitation
Diastolic Flow Reversal
- Colour and pulsed wave Doppler can detect diastolic flow reversal in the descending aorta
- Brief diastolic reversal = normal variant
- Holodiastolic (throughout diastole) reversal = at least moderate aortic regurgitation
🌡️ A continuous (pandiastolic) reversal is a hallmark of significant AR.
Interaction with Mitral Valve
- A regurgitant jet directed toward the mitral valve may:
- Cause anterior leaflet fluttering seen on 2D and M-mode
- Lead to functional impairment or flattening of the anterior mitral leaflet during diastole
- Disrupt normal mitral inflow patterns
Quantifying Aortic Regurgitation
Concept
- In a normal heart, left ventricular (LV) output ≈ mitral inflow.
- In aortic regurgitation (AR), LV outflow exceeds mitral inflow:
- LV output = mitral inflow + regurgitant volume (AR)
📊 The difference between LV outflow and mitral inflow represents the regurgitant volume (RV).
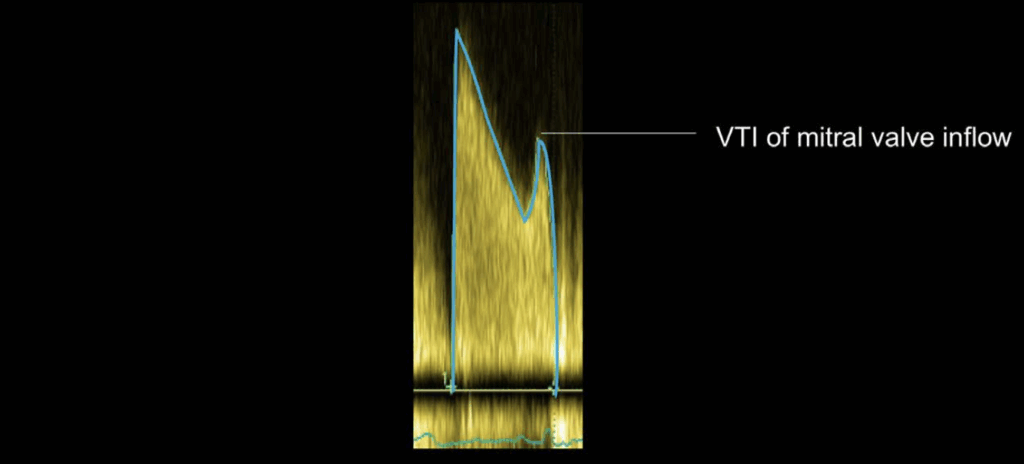
Step 1: Measure Mitral Valve Inflow
- Annulus diameter measured in mid-diastole from apical four-chamber view
- Mitral Valve Area (MVA) = π × (diameter ÷ 2)²
- Pulsed Wave Doppler (PWD) used at annulus level → trace VTI
- Mitral Stroke Volume (SVmitral) = MVA × VTI
Step 2: Measure LV Outflow
- LVOT diameter measured in parasternal long-axis view
- LVOT Area = π × (LVOT diameter ÷ 2)²
- LVOT VTI measured using PWD in apical five-chamber view
- LVOT Stroke Volume (SVlvot) = LVOT Area × VTI
Step 3: Calculate Regurgitant Volume and Fraction
- Regurgitant Volume (RV) = SVlvot – SVmitral
- Regurgitant Fraction (RF) = (RV ÷ SVlvot) × 100
Interpretation
| Metric | Mild AR | Severe AR |
|---|---|---|
| Regurgitant Volume | < 30 mL | > 60 mL |
| Regurgitant Fraction | < 30% | > 50% |
📌 This approach provides a quantitative, objective grading of aortic regurgitation severity.
Managing a Patient with Aortic Valve Disease
General Principles
- Management decisions should be individualized and based on a risk–benefit assessment.
- Ideally coordinated through a multidisciplinary heart valve team with expertise in:
- Structural heart interventions
- Cardiac surgery
- Imaging
- Heart failure
Aortic Regurgitation (AR) Management
Acute AR:
- Common causes: aortic dissection, infective endocarditis
- Requires urgent surgical intervention
Chronic AR:
- Symptomatic AR → Surgical valve replacement or repair
- Asymptomatic AR:
- Consider surgery if:
- LVEF < 50%
- LV end-diastolic diameter > 70 mm
- LV end-systolic diameter > 50 mm
- Consider surgery if:
- In asymptomatic patients, regular monitoring of:
- LV dimensions
- Ejection fraction
- Exercise tolerance
📆 Reviews every 6 months may be appropriate to monitor progression.
Follow-Up Considerations
- Consistency in serial echocardiography is essential.
- Use standardized imaging windows and measurement techniques across time points.
- Inconsistency can lead to false interpretation and inappropriate management.
This is an edited excerpt from the Medmastery course Echo Masterclass – The Valves by Chris Eggett, PhD. Acknowledgement and attribution to Medmastery for providing course transcripts.
Additional echocardiography resources:
- Na, M. Echo Masterclass: Left Ventricular Strain. Medmastery
- Monteiro, C. Echo Masterclass: The Right Heart. Medmastery
- West, C. Echo Masterclass: Adult Congenital Heart Disease. Medmastery
- Naderi, H. Echo Masterclass: The Power of 3D Imaging. Medmastery
Radiology Library: Echocardiography basics
- Eggett C. Echo basics: Valve Views. LITFL
- Eggett C. Echo basics: Valves, Measurements and Reports. LITFL
- Eggett C. Echo basics: Mitral valve. LITFL
- Eggett C. Echo basics: Mitral Regurgitation. LITFL
- Eggett C. Echo basics: Mitral Stenosis. LITFL
- Eggett C. Echo basics: Aortic Valve. LITFL
- Eggett C. Echo basics: Aortic Stenosis. LITFL
- Eggett C. Echo basics: Aortic Regurgitation. LITFL
- Eggett C. Echo basics: Tricuspid Valve. LITFL
- Eggett C. Echo basics: Pulmonary Valve. LITFL
- Eggett C. Echo basics: Prosthetic Valves. LITFL
Further reading
- Otto CM. Textbook of Clinical Echocardiography. Elsevier. 7e, 2023.
- Houghton AR. Making Sense of Echocardiography: A Hands-on Guide. 3e 2023
- Cadogan M. Aortic Regurgitation Eponymythology. LITFL
- Robbins A, Zhang G, Cadogan M. Eponymic Cardiac Murmurs. LITFL
- Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-e227.
Echocardiography Essentials
Cardiac physiologist, echocardiographer, and Professor of Healthcare Science Education, Faculty of Medical Sciences at the University of Newcastle, UK. I direct post-grad programs at the Faculty of Medical Sciences, run an echo clinic at the Freeman Hospital, and teach transthoracic echocardiography to specialists in critical and emergency care and anaesthetic settings

