Echo basics: Aortic Stenosis
Understand and identify aortic stenosis. Learn how to measure an accurate aortic valve gradient and calculate the aortic valve area. Be able to diagnose low-flow states and paradoxical low flow
Causes of Aortic Stenosis
- Calcific degeneration is the most common cause:
- Typically affects trileaflet valves in patients over 75 years.
- In younger patients (under 65), it is often associated with bicuspid valves.
- Rheumatic valve disease:
- Now rare in North America and Europe.
- Remains prevalent worldwide.
Identifying the Underlying Cause
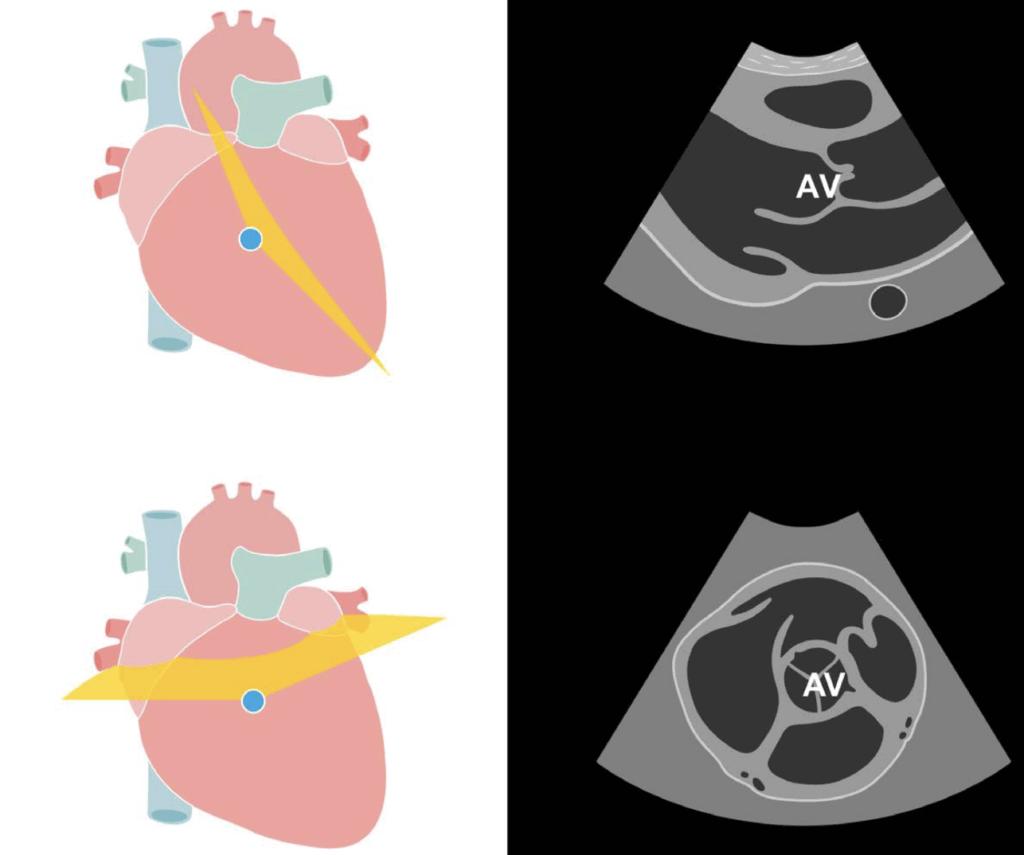
- The parasternal long-axis and short-axis views are key in evaluating valve morphology.
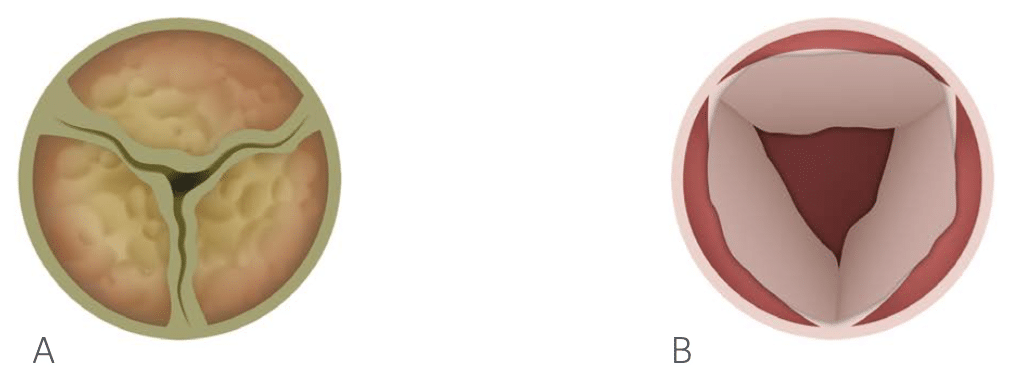
- Calcific degeneration:
- Involves central and basal cusp calcification.
- Rheumatic stenosis:
- Characterized by commissural fusion.
Assessing Cusp Configuration
- Calcium may obscure cusp number, making diagnosis challenging.
- Unicuspid valve:
- Single slit-like commissure with eccentric opening.
- Bicuspid valve:
- Two cusps of equal size, two sinuses, and a single commissure.
- May appear trileaflet if a raphe (seam) is present.
- Distinguishing bicuspid vs trileaflet:
- Observe during systole.
- If three sinuses are present, but cusp fusion is seen → trileaflet with fusion.
Visual Cues Suggesting Bicuspid Valve
- Asymmetric calcification pattern.
- Absence of the star-shaped opening seen in normal trileaflet valves.
- Look for raphe and cusp fusion dynamics during systole.
Grading Valve Calcification
- Mild calcification:
- Localized echobright spots on cusps.
- Moderate calcification:
- More extensive echobright areas.
- Severe calcification:
- Diffuse thickening with strong echogenicity.
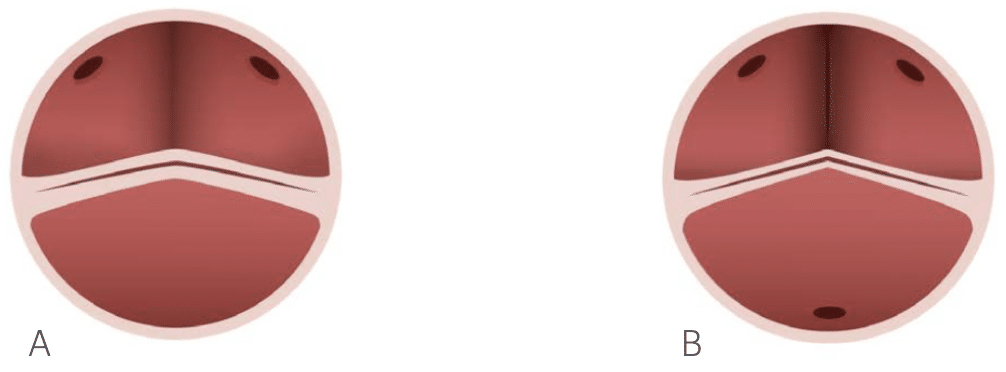
Valve Mobility in Aortic Stenosis
- In aortic stenosis, cusp motion is restricted:
- Cusps do not open fully during systole.
- Tips often point centrally into the aorta.
- Reduced mobility is suggestive of severity:
- However, visual assessment alone is insufficient for definitive diagnosis.
Measuring an Accurate Aortic Valve Gradient
Best Practice Recommendations
- Use Doppler-based measurements to:
- Record the peak jet velocity through the aortic valve.
- Calculate the mean pressure gradient across the valve.
Doppler Technique
- Continuous wave (CW) Doppler is essential for measuring flow velocity across the aortic valve.
- To ensure the maximum velocity is captured:
- Use multiple acoustic windows:
- Apical view (standard).
- Right sternal edge (often gives the highest velocity).
- Suprasternal notch.
- Use multiple acoustic windows:
Use of CW Doppler Probe
- A stand-alone CW Doppler probe (non-imaging) can be especially effective at the right sternal edge:
- It has a small footprint and can be better aligned with blood flow.
- However, it requires practice, so routine use is recommended to gain familiarity.
Recording and Reporting
- Document the maximum recorded jet velocity.
- Always include which view or acoustic window the velocity was obtained from:
- This assists with comparison in serial studies.
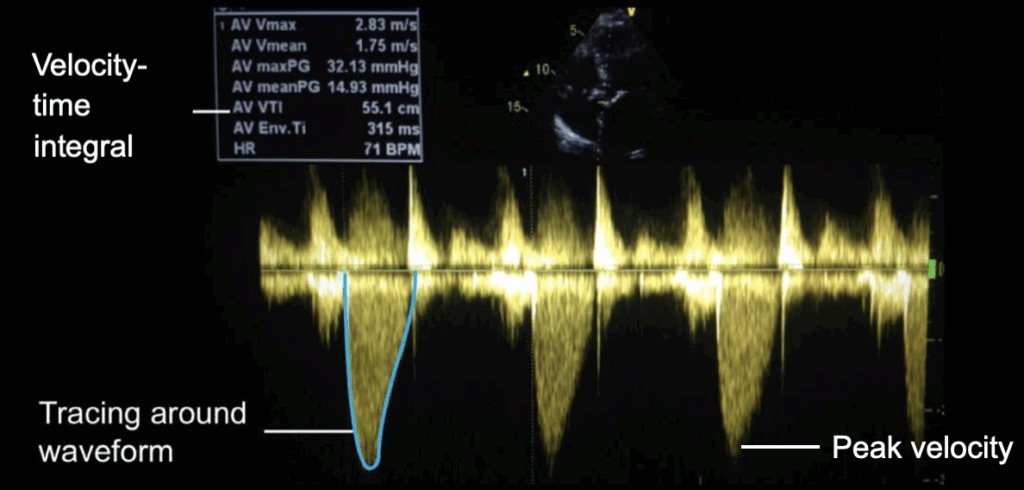
Optimizing the Doppler Signal
- The spectral display should:
- Fill the vertical axis of the display.
- Be recorded with a sweep speed of 50–100 mm/s.
- Show a smooth, dense-edged signal with a well-defined peak.
- Measurements:
- Peak velocity should be measured at the top of the Doppler curve.
- Mean gradient is calculated by tracing the curve (using the outer edge to generate the velocity-time integral or VTI).
Calculating the Aortic Valve Area
The Continuity Equation
The effective aortic valve area (AVA) is calculated using the continuity equation, based on the principle that flow through the left ventricular outflow tract (LVOT) equals flow through the aortic valve.
Three Essential Measurements
- Aortic valve VTI (Velocity Time Integral)
- Use continuous wave (CW) Doppler to trace the velocity curve across the aortic valve and obtain the VTI.
- LVOT VTI
- Use pulsed wave (PW) Doppler, typically from the apical five-chamber view.
- Place the sample volume just before the aortic valve.
- A correct position will show a smooth, peaked Doppler waveform—trace this to calculate the LVOT VTI.
- LVOT Diameter
- Measure at the annular level from a zoomed parasternal long-axis view.
- Use inner-edge to inner-edge caliper placement during mid-systole.
- Ensure consistency and precision, as errors are exponentially magnified (since area = πr²).
- The LVOT area is calculated as:

Calculation Principles
- The continuity equation:

- Measure 3 or more cardiac cycles in sinus rhythm and more in atrial fibrillation to improve accuracy.
- Remember:
- The LVOT is often elliptical, not perfectly circular.
- Inaccurate LVOT diameter measurements will disproportionately affect the final AVA due to squaring.
Dimensionless Index (Velocity Ratio)
- This is an alternative method to estimate stenosis severity without using LVOT diameter:

- Interpretation:
- ≈ 1.0 = Normal (no stenosis)
- < 1.0 = Stenosis present
- ≤ 0.25 = Severe aortic stenosis
Diagnosing Low-Flow States
Importance of Left Ventricular Function
Assessment of left ventricular (LV) function is essential because it:
- Provides important prognostic information
- Guides clinical management
- Influences the assessment of aortic stenosis severity
The Effect of Low Flow on Aortic Valve Assessment
When LV function is impaired:
- Transvalvular flow is reduced
- Cusp opening of the aortic valve is limited
- Continuity equation–based AVA (aortic valve area) may appear reduced, even if true severe aortic stenosis is not present
Diagnosing Paradoxical Low Flow
Understanding Paradoxical Low-Flow, Low-Gradient Aortic Stenosis
In some cases, discordant echocardiographic findings may be observed:
- Low transvalvular gradient
- Small aortic valve area (AVA)
- Low calculated stroke volume
- Normal left ventricular ejection fraction (LVEF)
This scenario is known as paradoxical low-flow, low-gradient aortic stenosis (AS) with preserved ejection fraction.
Mechanism Behind Paradoxical Low Flow
- The low-flow state is typically due to left ventricular concentric hypertrophy, which:
- Reduces ventricular cavity size
- Results in lower total stroke volume, even with normal ejection fraction
- Leads to reduced forward flow across the stenotic aortic valve
Key Considerations
- Recheck all measurements before making the diagnosis
- Rule out measurement error and severe systemic hypertension, both of which can mimic this picture
- Elevated blood pressure is often present and may contribute to reduced forward flow
Next Steps in Evaluation
- Once technical and physiological confounders are excluded, further evaluation should include:
- Clinical correlation
- Additional imaging (e.g., CT calcium scoring, cardiac MRI)
- Integration of all findings to determine if true severe AS is present
Managing a Patient with Aortic Valve Disease
General Principles
- Management decisions should be individualized and based on a risk–benefit assessment.
- Ideally coordinated through a multidisciplinary heart valve team with expertise in:
- Structural heart interventions
- Cardiac surgery
- Imaging
- Heart failure
Aortic Stenosis (AS) Monitoring Guidelines
| Severity | Symptoms | Echo Surveillance |
|---|---|---|
| Mild AS | Asymptomatic | Every 3–5 years |
| Moderate AS | Asymptomatic | Every 1–2 years |
| Severe AS | Asymptomatic with peak velocity > 4 m/s | Every 6 months |
- If maximum jet velocity increases > 0.3 m/s per year, surgery should be considered.
Indications for Intervention in Aortic Stenosis
- Symptomatic severe AS → Urgent valve intervention (surgical AVR preferred; TAVI if high risk).
- Asymptomatic severe AS with reduced LV ejection fraction (<50%) → Surgical valve replacement.
- Asymptomatic patients undergoing CABG or other valve surgery → Concomitant AVR recommended.
Follow-Up Considerations
- Consistency in serial echocardiography is essential.
- Use standardized imaging windows and measurement techniques across time points.
- Inconsistency can lead to false interpretation and inappropriate management.
This is an edited excerpt from the Medmastery course Echo Masterclass – The Valves by Chris Eggett, PhD. Acknowledgement and attribution to Medmastery for providing course transcripts.
Additional echocardiography resources:
- Na, M. Echo Masterclass: Left Ventricular Strain. Medmastery
- Monteiro, C. Echo Masterclass: The Right Heart. Medmastery
- West, C. Echo Masterclass: Adult Congenital Heart Disease. Medmastery
- Naderi, H. Echo Masterclass: The Power of 3D Imaging. Medmastery
Radiology Library: Echocardiography basics
- Eggett C. Echo basics: Valve Views. LITFL
- Eggett C. Echo basics: Valves, Measurements and Reports. LITFL
- Eggett C. Echo basics: Mitral valve. LITFL
- Eggett C. Echo basics: Mitral Regurgitation. LITFL
- Eggett C. Echo basics: Mitral Stenosis. LITFL
- Eggett C. Echo basics: Aortic Valve. LITFL
- Eggett C. Echo basics: Aortic Stenosis. LITFL
- Eggett C. Echo basics: Aortic Regurgitation. LITFL
- Eggett C. Echo basics: Tricuspid Valve. LITFL
- Eggett C. Echo basics: Pulmonary Valve. LITFL
- Eggett C. Echo basics: Prosthetic Valves. LITFL
Further reading
- Robbins A, Zhang G, Cadogan M. Eponymic Cardiac Murmurs. LITFL
- Otto CM. Textbook of Clinical Echocardiography. Elsevier. 7e, 2023.
- Houghton AR. Making Sense of Echocardiography: A Hands-on Guide. 3e 2023
- Kanwar A, Thaden JJ, Nkomo VT. Management of Patients With Aortic Valve Stenosis. Mayo Clin Proc. 2018 Apr;93(4):488-508.
- Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-e227.
Echocardiography Essentials
Cardiac physiologist, echocardiographer, and Professor of Healthcare Science Education, Faculty of Medical Sciences at the University of Newcastle, UK. I direct post-grad programs at the Faculty of Medical Sciences, run an echo clinic at the Freeman Hospital, and teach transthoracic echocardiography to specialists in critical and emergency care and anaesthetic settings

