Echo basics: Mitral Valve
Normal mitral valve echo anatomy
The mitral valve is a dominant structure in most standard echocardiographic views. Understanding its anatomy in each window is essential for accurate assessment.
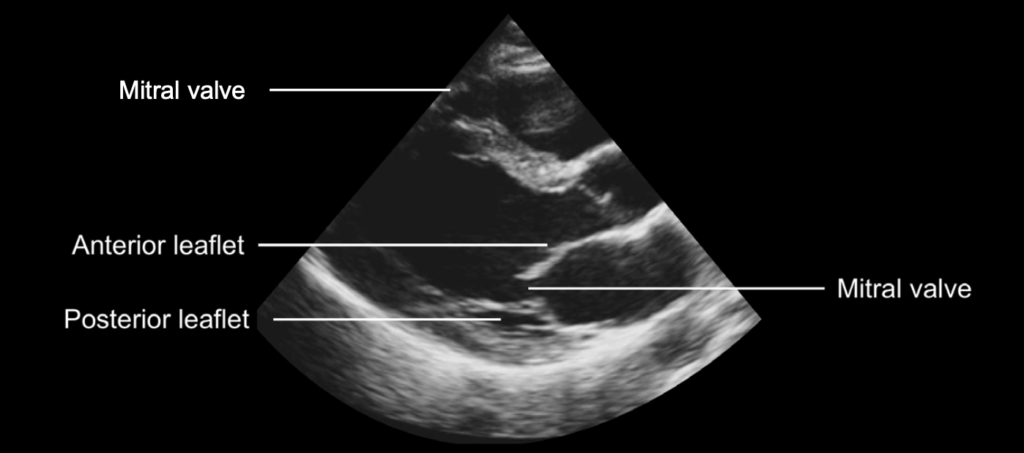
Parasternal Long-Axis View
- The mitral valve leaflets are thin and echogenic, appearing similar in brightness.
- The anterior leaflet is longer and nearly contacts the ventricular septum during diastole.
- During systole, both leaflets coapt at their tips, forming the zone of apposition.
- This view typically shows A2 and P2 scallops when aligned correctly.
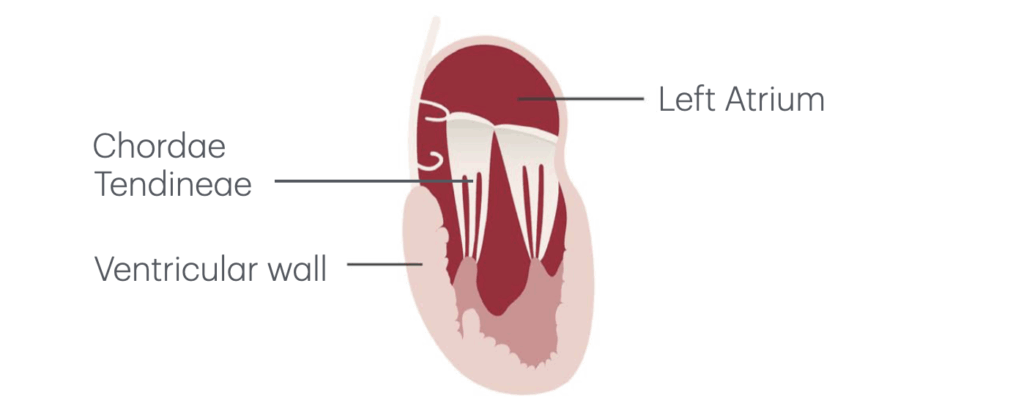
- Chordae tendineae are seen extending from leaflet tips to posteromedial papillary muscles.
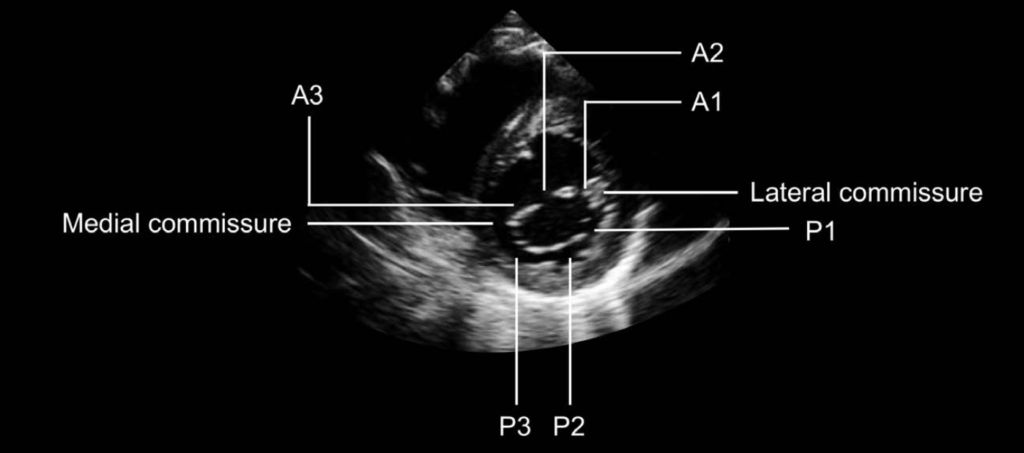
Parasternal Short-Axis View
- Excellent for identifying leaflet subdivisions.
- The posterior leaflet has three scallops: P1, P2, and P3.
- These appear in reverse order on the image:
- P3 = medial (left side)
- P2 = central
- P1 = lateral (right side)
- These appear in reverse order on the image:
- The anterior leaflet corresponds to A1, A2, A3, arranged to match posterior scallops.
- Mitral commissures (lateral and medial) mark junctions between anterior and posterior leaflets.
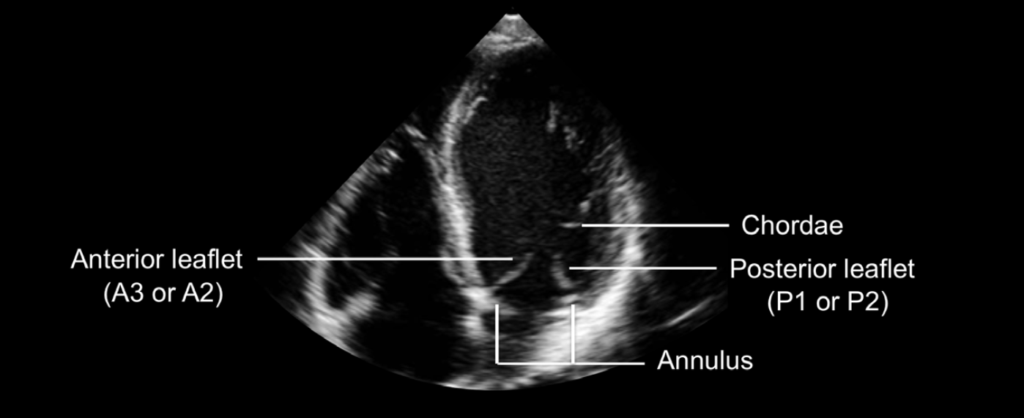
Apical Four-Chamber View
- Anterior leaflet appears on the septal (left) side, posterior leaflet on the lateral (right) side.
- Commonly visualized scallops:
- Anterior: A2 or A3
- Posterior: P1 or P2
- Chordae can be traced to the anterolateral papillary muscle.
- The mitral annulus shows its major dimension, with its saddle shape apparent.
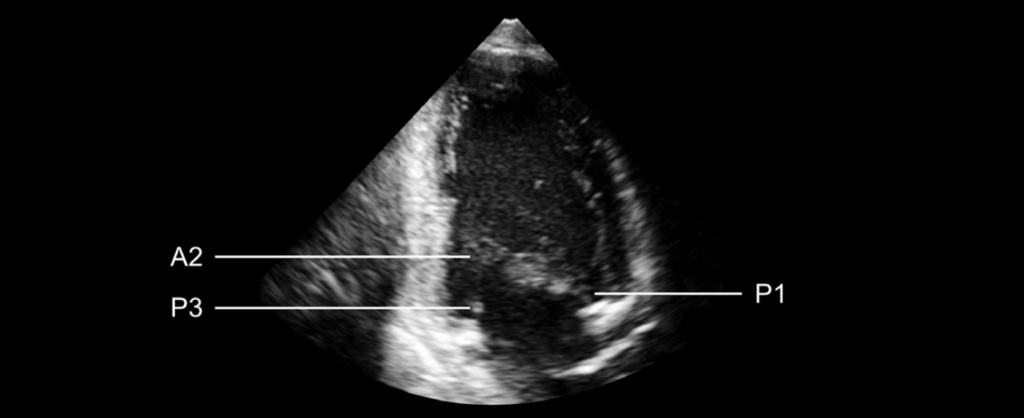
Apical Two-Chamber View
- Predominantly shows posterior leaflet (especially P1 and P3).
- The anterior leaflet is viewed en face (flat-on).
- In a true two-chamber image:
- Left side = P3
- Middle = A2
- Right side = P1
- This view is useful for both structural and color Doppler flow assessment.
Apical Long-Axis (Three-Chamber) View
- Similar to parasternal long-axis view, but with slightly deeper visualization.
- May have lower resolution but is well-suited for:
- Doppler alignment
- Color flow interrogation
Recognising an abnormal mitral valve
A detailed and accurate assessment of the mitral valve requires a methodical, step-by-step approach that evaluates each component of the valve apparatus and its surrounding structures.
Stepwise Valve Inspection
Leaflets:
- Are the anterior and posterior leaflets thin and pliable?
- Or do they appear thickened with restricted movement?
Annulus:
- Is the annulus echogenic (bright)?
- Is the calcification localized or diffuse?
- View in multiple windows for a comprehensive assessment.
Chordae tendineae:
- Do they appear thicker or brighter than usual (suggesting calcification)?
- Are they shortened, fused, or ruptured?
Surrounding myocardium:
- Assess for thinning or scarring, particularly in patients with coronary artery disease.
Left atrium:
- Check for thrombus, especially in atrial fibrillation.
- Evaluate for atrial dilatation, commonly associated with valve dysfunction.
Left ventricle:
- Assess for dilatation, which may enlarge the annulus and impair coaptation.
Characteristic Pathological Patterns
Rheumatic Heart Disease:
- Thickened leaflet tips, possible calcification.
- Restricted motion, leading to doming or “hockey stick” appearance in diastole.
- Often involves shortened or calcified chordae.
Degenerative Mitral Valve Disease:
- Diffuse thickening of the entire leaflet.
- May range from:
- Fibroelastic deficiency: localized prolapse, thinner valve structure.
- Barlow syndrome: excess leaflet tissue, myxomatous degeneration, elongated and ruptured chordae, leaflet prolapse.
Mitral Valve Prolapse:
- Leaflets move >2 mm above annulus into the LA.
- Symmetric prolapse: both leaflets involved.
- Asymmetric prolapse: single leaflet—higher risk of rupture and flail.
Barlow Valve (Extreme Degeneration):
- Excess leaflet tissue, diffuse myxomatous change, and chordal elongation or rupture.
Other Notable Pathologies
Mitral Annular Calcification:
- Common in elderly and renal patients.
- Typically begins in the posterior annulus.
- May impair leaflet motion if calcification is extensive.
- Best visualized in parasternal long-axis and short-axis views.
Infective Endocarditis:
- Mobile echodensities (vegetations) attached to leaflets.
- Possible leaflet perforation, flail leaflet due to chordal rupture.
Infiltrative Cardiomyopathy:
- Valve leaflets may appear thickened due to tissue infiltration.
- Coaptation is often impaired.
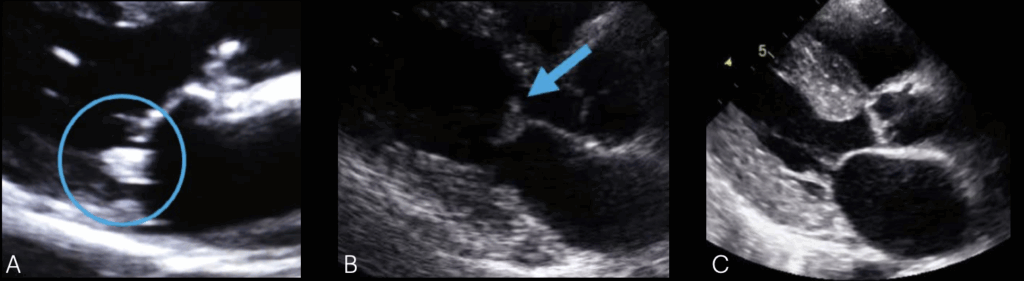
B. Infective Endocarditis with mobile structures (vegetations) attached to the valve leaflets
C. Infiltrative Cardiomyopathy with excessive thickening of the ventricular walls and the valve leaflets
Functional (Secondary) Mitral Valve Abnormalities
Ischemic Heart Disease:
- Papillary muscle dysfunction alters chordal tension.
- Results in leaflet tethering and poor apposition.
- May lead to mitral regurgitation despite normal leaflet morphology.
- Severe ischemia can cause papillary muscle rupture → flail leaflet.
Dilated Cardiomyopathy:
- Annular dilation and apical tethering of leaflets.
- Subvalvular distortion impairs leaflet coaptation.
- Functionally significant mitral regurgitation despite structurally normal leaflets.
Conclusion
A systematic echocardiographic inspection of the mitral valve and its surrounding structures—across multiple views—helps accurately determine the type and severity of valve disease. Recognising structural changes, mobility abnormalities, and associated functional changes is essential for a clinically useful report.
This is an edited excerpt from the Medmastery course Echo Masterclass – The Valves by Chris Eggett, PhD. Acknowledgement and attribution to Medmastery for providing course transcripts.
Additional echocardiography resources:
- Na, M. Echo Masterclass: Left Ventricular Strain. Medmastery
- Monteiro, C. Echo Masterclass: The Right Heart. Medmastery
- West, C. Echo Masterclass: Adult Congenital Heart Disease. Medmastery
- Naderi, H. Echo Masterclass: The Power of 3D Imaging. Medmastery
Radiology Library: Echocardiography basics
- Eggett C. Echo basics: Valve Views. LITFL
- Eggett C. Echo basics: Valves, Measurements and Reports. LITFL
- Eggett C. Echo basics: Mitral valve. LITFL
- Eggett C. Echo basics: Mitral Regurgitation. LITFL
- Eggett C. Echo basics: Mitral Stenosis. LITFL
- Eggett C. Echo basics: Aortic Valve. LITFL
- Eggett C. Echo basics: Aortic Stenosis. LITFL
- Eggett C. Echo basics: Aortic Regurgitation. LITFL
- Eggett C. Echo basics: Tricuspid Valve. LITFL
- Eggett C. Echo basics: Pulmonary Valve. LITFL
- Eggett C. Echo basics: Prosthetic Valves. LITFL
Further reading
- Otto CM. Textbook of Clinical Echocardiography. Elsevier. 7e, 2023.
- Houghton AR. Making Sense of Echocardiography: A Hands-on Guide. 3e 2023
- Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-e227.
- Irvine T, Li XK, Sahn DJ, Kenny A. Assessment of mitral regurgitation. Heart. 2002 Nov;88 Suppl 4(Suppl 4):iv11-9.
Echocardiography Essentials
Cardiac physiologist, echocardiographer, and Professor of Healthcare Science Education, Faculty of Medical Sciences at the University of Newcastle, UK. I direct post-grad programs at the Faculty of Medical Sciences, run an echo clinic at the Freeman Hospital, and teach transthoracic echocardiography to specialists in critical and emergency care and anaesthetic settings

