Echo basics: Mitral Regurgitation
Identifying mitral valve regurgitation
Mitral regurgitation (MR) is a common pathology detected during echocardiography. Accurate identification and grading rely heavily on colour and spectral Doppler imaging across multiple standard views.
Use of Colour Doppler Imaging
Routine Practice:
- Colour Doppler should be applied in almost every view when assessing the mitral valve.
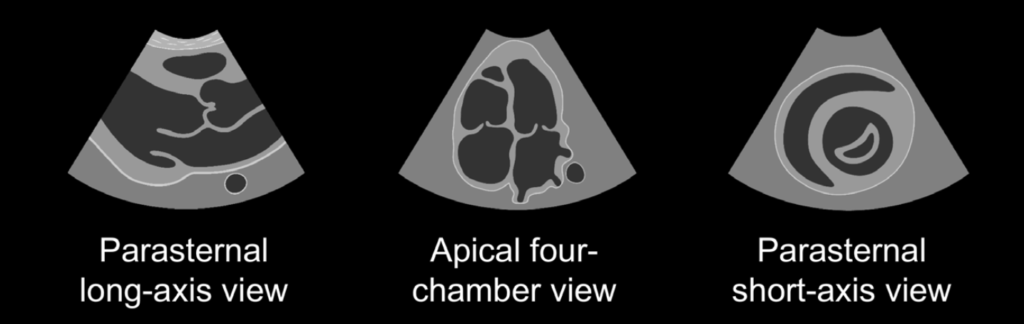
- Particularly useful views:
- Parasternal long-axis
- Apical four-chamber
- Apical two-chamber
- Parasternal short-axis
Colour Box Optimization:
- Size the colour box to capture the region above and below the valve, but keep it as small as possible for optimal frame rate.
Jet Identification:
- Mitral regurgitation appears as a predominantly blue jet (away from the probe) in standard imaging orientation.
- Determine whether the jet is:
- Central (directly into the atrium)
- Eccentric (directed towards atrial walls)
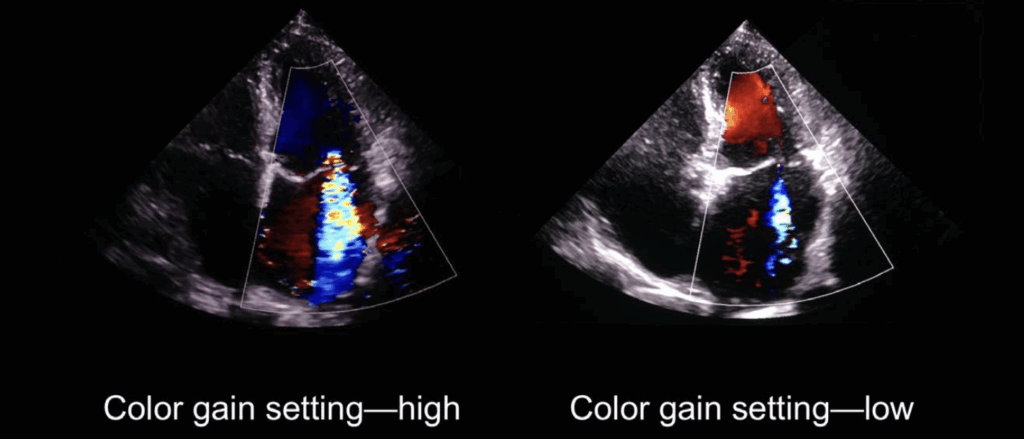
Caution in Visual Interpretation:
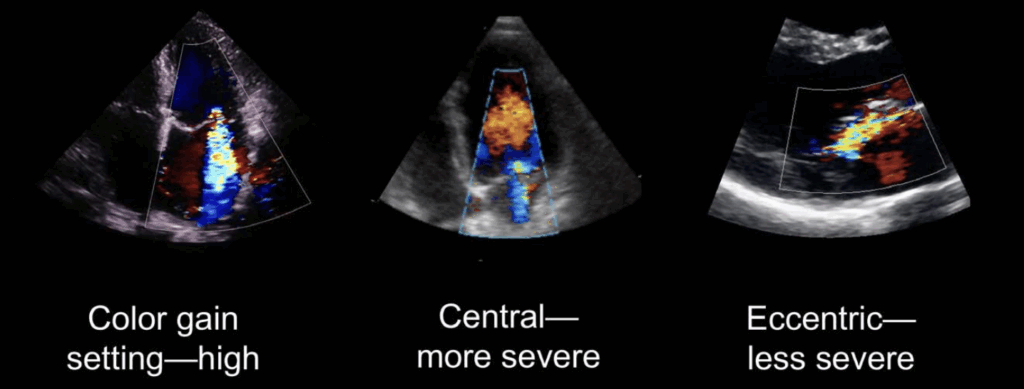
- High gain settings may overestimate MR severity.
- Central jets appear more severe due to beam alignment.
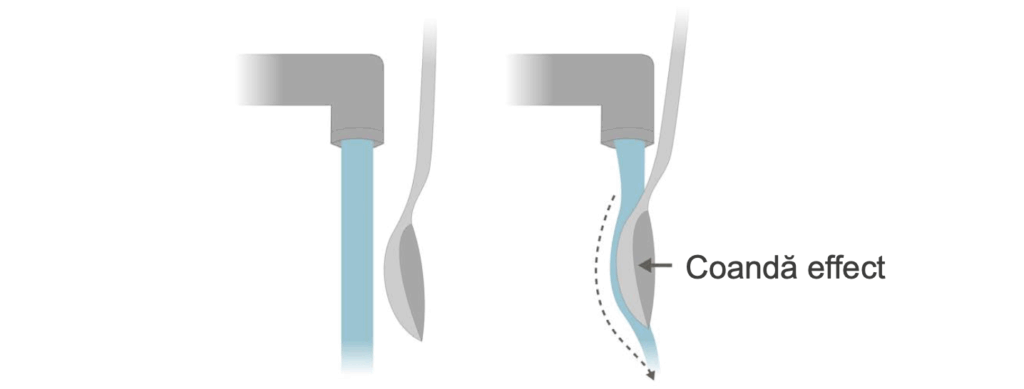
- Eccentric jets may be underestimated due to the Coandă effect, where the jet clings to the atrial wall, appearing smaller than it is.
Doppler Assessment of Mitral Regurgitation
Preferred View:
- The apical four-chamber view provides the best alignment with regurgitant flow for Doppler analysis.
Spectral Doppler Features:
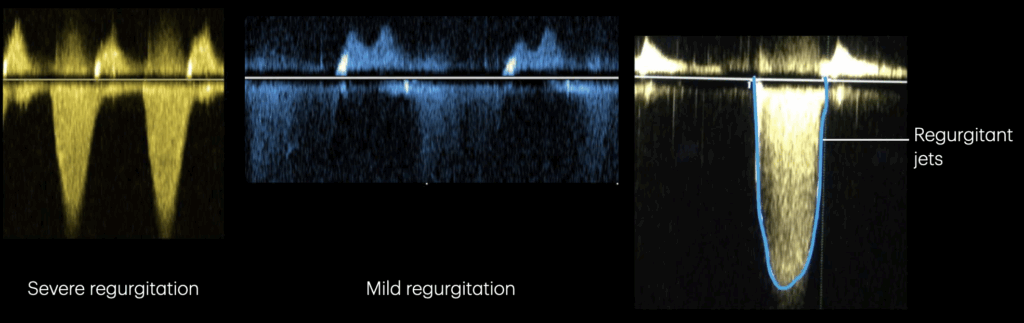
- MR jets appear as high-velocity systolic signals below the baseline.
- Signal density helps gauge severity:
- Bright, dense signal = moderate to severe MR
- Faint, low-density signal = mild MR
Comparison Strategy:
- Compare regurgitant jet density with the mitral inflow signal:
- If similar, MR is likely severe.
- Note: Off-axis jets can result in underestimation of severity.
Structural and Functional Assessment
Left Ventricular Dimensions:
- Chronic MR leads to volume overload and progressive LV dilatation.
- Measure:
- LV end-systolic dimension (LVESD)
- LV end-diastolic dimension (LVEDD)
- Prolonged volume overload can lead to LV systolic dysfunction.
Left Atrial Size:
- Significant MR causes LA dilation.
- However, LA dilation may also result from hypertension, diastolic dysfunction, or atrial arrhythmias.
- A normal LA size generally excludes severe chronic MR.
Pulmonary Venous and Right Heart Assessmen
Pulmonary Venous Flow:
- Severe MR may result in retrograde flow into pulmonary veins.
- Can occasionally be demonstrated with Doppler.
Pulmonary Hypertension:
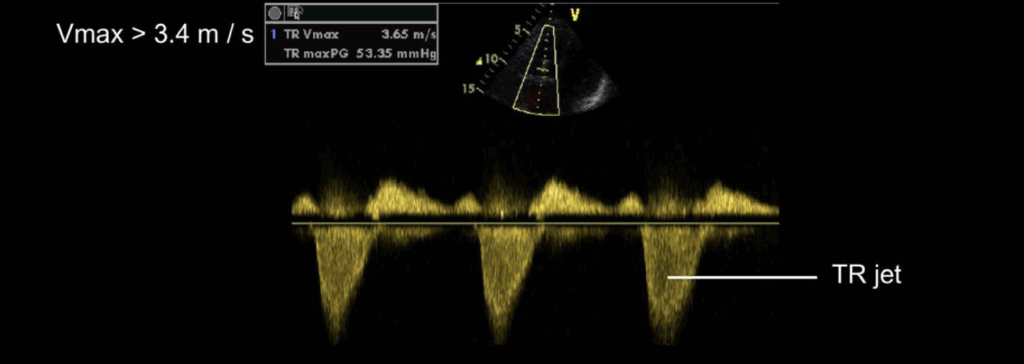
- Chronic MR may elevate pulmonary artery pressures.
- Assess tricuspid regurgitation jet via continuous wave Doppler.
- TR jet velocity > 3.4 m/s suggests pulmonary hypertension.
RV Function:
- Always assess right ventricular size and function, particularly in the presence of elevated pulmonary pressures.
Summary Approach to MR Evaluation
Always consider clinical context and integrate findings from multiple views for a comprehensive report.
- Use colour Doppler in all key views.
- Localize and characterize the regurgitant jet (central vs. eccentric).
- Analyze spectral Doppler signal density and timing.
- Measure LV and LA dimensions and assess global function.
- Evaluate pulmonary pressures and coexistent tricuspid regurgitation.
Quantifying mitral regurgitation based on colour imaging
Once mitral regurgitation (MR) is identified, the next step is to determine severity using a grading scale of mild, moderate, or severe. An integrated approach is essential—no single technique is perfect.
Limitations of Jet Area Measurement
- Regurgitant jet area (absolute or indexed to LA size) is not recommended due to:
- High dependence on machine settings
- Influence of jet direction and regurgitation mechanism
- Inaccuracy with colour gain adjustments
Recommended Quantitative and Semi-Quantitative Methods
Two widely used and relatively accessible techniques:
- Vena Contracta Width – Semi-quantitative
- PISA Method (Proximal Isovelocity Surface Area) – Quantitative
1. Vena Contracta Measurement
Overview:
- Simple and quick
- Useful in differentiating mild from significant MR
- Performed in parasternal long-axis view
Imaging Setup:
- Zoom in on the mitral valve
- Colour Doppler Nyquist limit: ~50–60 cm/s
- Colour box small, centred on leaflet tips
Measurement Technique:
- Identify narrowest diameter of flow on atrial side of the valve
- Measure using calipers on a frame-by-frame loop review
Interpretation:
- < 3 mm → Mild MR
- > 7 mm → Severe MR
- 3–7 mm → Requires further quantification (e.g., PISA)
2. PISA (Proximal Isovelocity Surface Area) Method
Principle:
- Based on hemispheric convergence of flow proximal to the regurgitant orifice
- Uses aliasing velocity and radius to calculate regurgitant flow rate, ROA, and regurgitant volume
Imaging Technique:
- Zoomed view of MR flow convergence
- Adjust colour Doppler scale to ~15–40 cm/s to create aliasing hemisphere
- Measure radius (r) of first aliasing shell
Key Equation:
- Flow rate at aliasing hemisphere:

Use Doppler to measure:
- vMR = peak MR jet velocity (from CW Doppler)
- VTIMR = velocity-time integral of the MR jet
Calculated Parameters
A. Regurgitant Orifice Area (ROA):

Interpretation:
- < 20 mm² → Mild MR
- ≥ 40 mm² → Severe MR
B. Regurgitant Volume (RV):

Interpretation:
- < 30 mL/beat → Mild MR
- ≥ 60 mL/beat → Severe MR
Summary Table
| Parameter | Mild MR | Severe MR |
|---|---|---|
| Vena Contracta Width | < 3 mm | ≥ 7 mm |
| ROA | < 20 mm² | ≥ 40 mm² |
| Regurgitant Volume (per beat) | < 30 mL | ≥ 60 mL |
Practical Notes
- Image optimization (zoom, gain, colour scale) is crucial for accurate measurement.
- Use multiple techniques for confirmation—especially important in:
- Eccentric jets
- Poor image quality
- Confounding atrial or ventricular abnormalities
This is an edited excerpt from the Medmastery course Echo Masterclass – The Valves by Chris Eggett, PhD. Acknowledgement and attribution to Medmastery for providing course transcripts.
Additional echocardiography resources:
- Na, M. Echo Masterclass: Left Ventricular Strain. Medmastery
- Monteiro, C. Echo Masterclass: The Right Heart. Medmastery
- West, C. Echo Masterclass: Adult Congenital Heart Disease. Medmastery
- Naderi, H. Echo Masterclass: The Power of 3D Imaging. Medmastery
Radiology Library: Echocardiography basics
- Eggett C. Echo basics: Valve Views. LITFL
- Eggett C. Echo basics: Valves, Measurements and Reports. LITFL
- Eggett C. Echo basics: Mitral valve. LITFL
- Eggett C. Echo basics: Mitral Regurgitation. LITFL
- Eggett C. Echo basics: Mitral Stenosis. LITFL
- Eggett C. Echo basics: Aortic Valve. LITFL
- Eggett C. Echo basics: Aortic Stenosis. LITFL
- Eggett C. Echo basics: Aortic Regurgitation. LITFL
- Eggett C. Echo basics: Tricuspid Valve. LITFL
- Eggett C. Echo basics: Pulmonary Valve. LITFL
- Eggett C. Echo basics: Prosthetic Valves. LITFL
Further reading
- Otto CM. Textbook of Clinical Echocardiography. Elsevier. 7e, 2023.
- Houghton AR. Making Sense of Echocardiography: A Hands-on Guide. 3e 2023
- Robbins A, Zhang G, Cadogan M. Eponymic Cardiac Murmurs. LITFL
- Irvine T, Li XK, Sahn DJ, Kenny A. Assessment of mitral regurgitation. Heart. 2002;88 (4):iv11-9.
- Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-e227.
- Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, Crumb SR, Dearani JA, Fuller S, Gurvitz M, Khairy P, Landzberg MJ, Saidi A, Valente AM, Van Hare GF. 2018 AHA/ACC Guideline for the Management of Adults With Congenital Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Apr 2;139(14):e637-e697
Echocardiography Essentials
Cardiac physiologist, echocardiographer, and Professor of Healthcare Science Education, Faculty of Medical Sciences at the University of Newcastle, UK. I direct post-grad programs at the Faculty of Medical Sciences, run an echo clinic at the Freeman Hospital, and teach transthoracic echocardiography to specialists in critical and emergency care and anaesthetic settings

