Echo basics: Prosthetic Valve
Understand and identify prosthetic valves. Learn what can go wrong with prosthetic valves; how to assess their function and examine transcatheter valves
Recognizing the Variety of Prosthetic Valves
Overview of Valve Replacement Types
Valve replacement options can be categorized by construction into three primary types:
- Bioprosthetic valves
- Mechanical valves
- Homografts
Bioprosthetic (Tissue) Valves
- Constructed from animal tissue (xenografts), most commonly:
- Porcine aortic valves
- Bovine pericardial tissue
- Mimic native valve anatomy:
- Leaflets shaped like normal valve leaflets
- Attached to a support ring
- Stented designs have supporting struts at commissures
- Stentless options are available but less common
- Most widely used in valve replacement
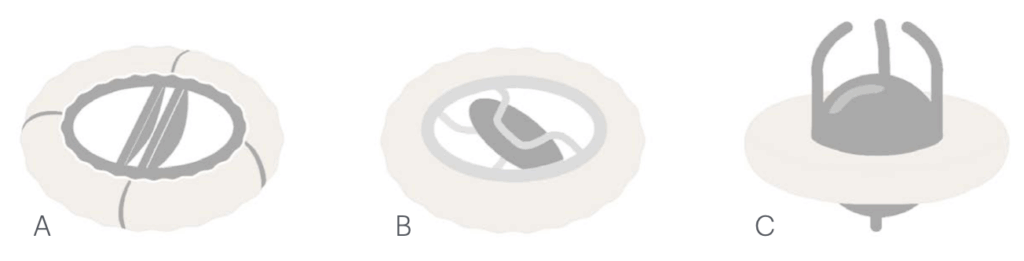
Mechanical Valves
- Durable, long-lasting valves with varied historical designs
- Most common type in use today: bileaflet mechanical valve
- Composed of two hinged semicircular discs
- Blood flows through three orifices:
- Two outer crescent-shaped openings
- One smaller central passage
- Older models may still be encountered:
- Tilting disc valves
- Ball and cage valves
Homograft Valves
- Constructed from cryopreserved human valves
- Donor-derived tissue post-mortem
- Typically used for semilunar valve replacement (e.g., aortic or pulmonary)
- Offer good hemodynamic performance and resistance to infection
Advances in Valve Implantation Techniques
- Open-heart surgery was historically the only option for valve replacement
- Transcatheter Aortic Valve Implantation/Replacement (TAVI/TAVR) is now widely used in eligible patients
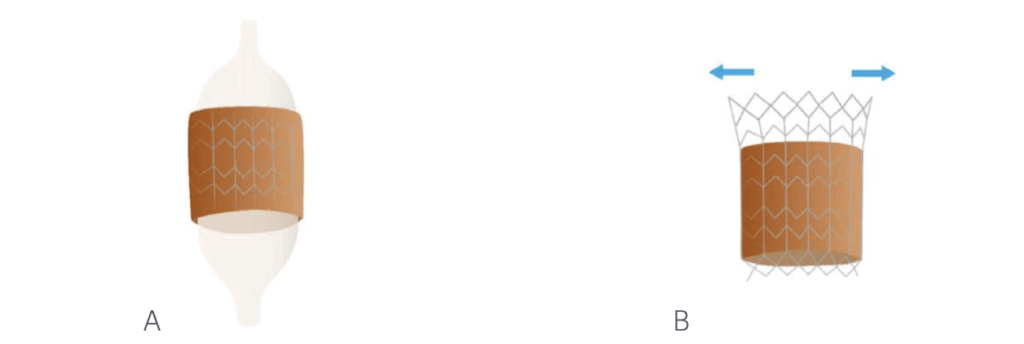
Types of Transcatheter Valves
- Balloon-expandable valves:
- Made from bovine tissue
- Mounted on a cobalt-chromium metal frame
- Self-expanding valves:
- Constructed from porcine or bovine pericardial tissue
- Contained within a nitinol (nickel-titanium) wire mesh frame
What Can Go Wrong with Prosthetic Valves?
Structural Valve Deterioration
- Mechanical valve failure is rare due to robust design.
- Bioprosthetic valves:
- Gradual degeneration of leaflet tissue can occur.
- Leads to reduced pliability, resulting in:
- Stenosis
- Regurgitation
Annular and Sewing Ring Complications
- Changes in the valve annulus over time may affect the sewing ring.
- Suture dehiscence can occur, causing paravalvular regurgitation.
- Valve rocking on imaging is a serious sign, indicating potential dehiscence.
Thrombus Formation
- Mechanical valves are associated with a high risk of thrombus formation:
- Risk of embolic events
- Risk of valve dysfunction
- Recent evidence suggests bioprosthetic valves may also develop thrombi.
Infective Endocarditis
- A serious complication of prosthetic valves.
- May present with vegetations similar to native valves.
- Subtle infections may localize to the sewing ring:
- Vegetations may not be visible.
- Look for:
- Paravalvular regurgitation
- Loss of valve fixation (“rocking valve”)
Pannus Formation
- Overgrowth of fibrous and endothelial tissue around the valve.
- Can impair valve function similarly to thrombus.
- Occurs more commonly in mechanical valves.
Patient-Prosthesis Mismatch
- Occurs when the prosthetic valve is too small relative to patient body size.
- Even a normally functioning valve may:
- Fail to meet physiological demand
- Lead to increased transvalvular gradients
- Always a factor to some degree in mechanical and tissue valves due to:
- Sewing ring
- Occluders
- Stents
- Significant clinical impact only if mismatch is severe.
Assessing the Function of Prosthetic Valves
General Considerations
- Echocardiography is central to evaluating prosthetic valve function but is technically challenging.
- Artifact and acoustic shadowing commonly limit visualization.
- Knowledge of:
- Valve type and size
- Expected Doppler values
- Reference normal ranges
is essential for accurate interpretation.
- A baseline postoperative echocardiogram should be performed to:
- Confirm normal function
- Provide reference values for future comparison
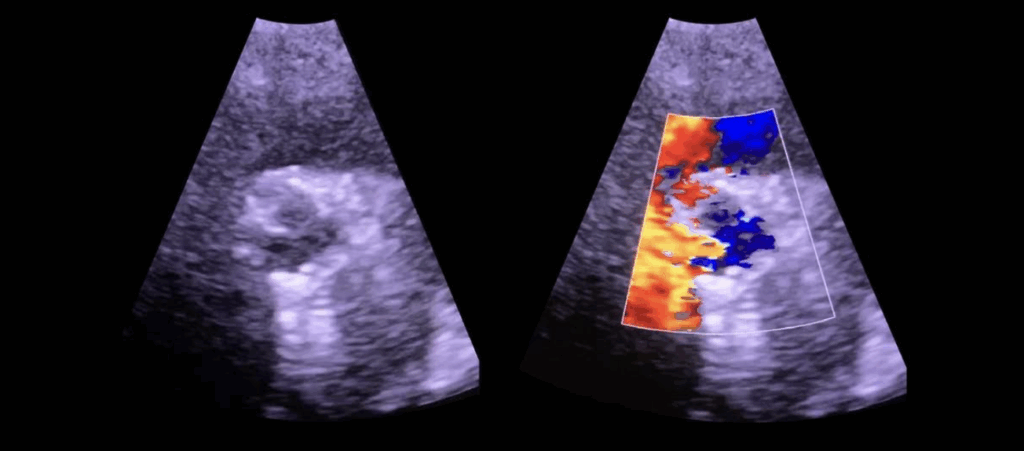
Visual Assessment
- Aortic prosthetic valves:
- Should appear stable with visible, full cusp/occluder motion
- Use color Doppler to confirm flow occupies the orifice during systole
- Abnormal findings may include:
- Thickened or immobile cusps/occluders
- Limited visualization due to acoustic interference
Doppler Assessment of Obstruction
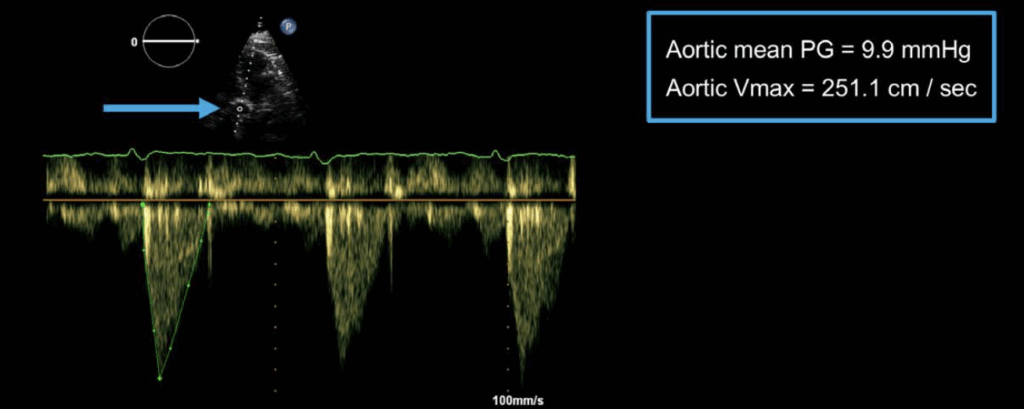
- Aortic valve prosthesis:
- Peak velocity ≥ 4.0 m/s suggests severe obstruction
- Mean gradient ≥ 35 mmHg suggests severe obstruction
- Mitral valve prosthesis:
- Peak velocity > 2.5 m/s is suspicious
- Pressure half-time > 200 ms suggests obstruction
- Tricuspid valve prosthesis:
- Peak velocity > 1.6 m/s indicates possible obstruction
- Pulmonary valve prosthesis:
- Peak velocity > 3.2 m/s indicates possible obstruction
Assessment of Regurgitation
- Mechanical valves:
- Regurgitation is common and expected
- Each valve has a distinct regurgitant jet pattern
- Bileaflet valves show multiple small jets on closure
- Bioprosthetic valves:
- Trivial regurgitation may be normal
- More than trivial regurgitation is suspicious
- Assess leaflet motion and origin of regurgitation:
- Intravalvular vs. paravalvular
- Clock face analogy (from short-axis view) is useful for:
- Describing paravalvular leak location
- Enhancing consistency in serial follow-up
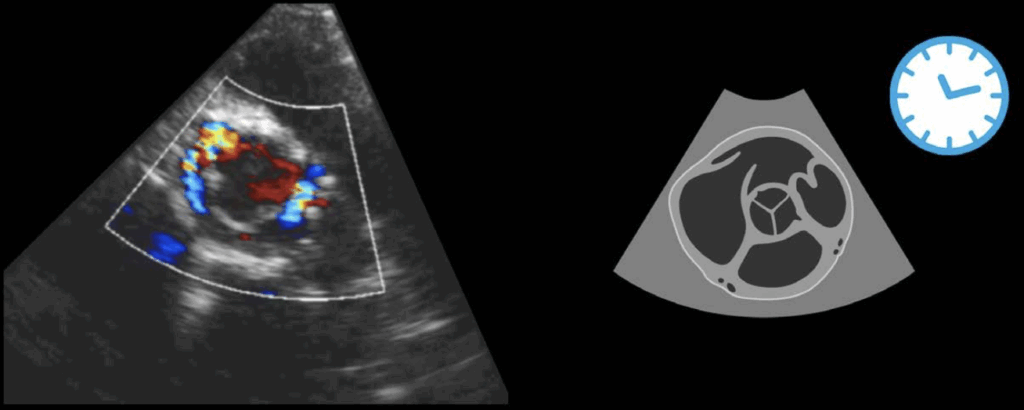
Examining Transcatheter Valves
Indications and Pre-Procedural Assessment
- TAVR (TAVI) is indicated in symptomatic patients with aortic stenosis who are unsuitable for surgery.
- Transthoracic echocardiography (TTE) is the primary tool for:
- Pre-procedural assessment
- Post-procedural follow-up
Pre-Procedural Echo Requirements:
- Determine whether the native valve is bicuspid or tricuspid
- Bicuspid valves are associated with higher risk of post-procedural aortic regurgitation
- Identify calcification in:
- The valve
- LVOT
- Proximal aorta (risk: dissection)
- Measure:
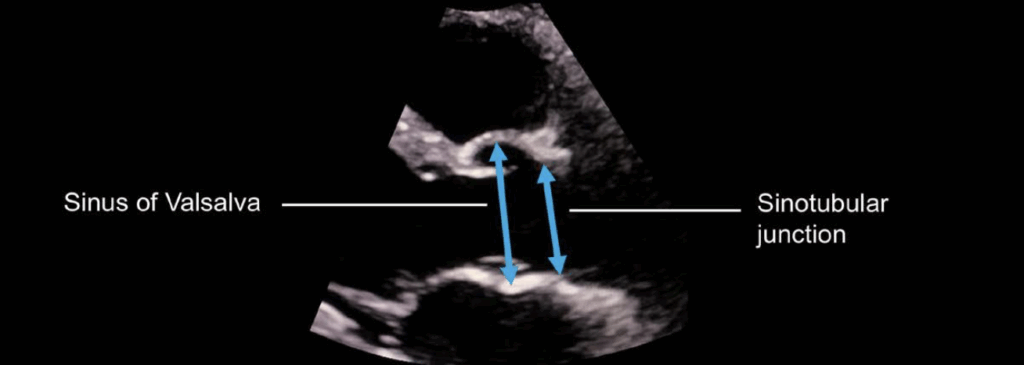
- Sinus of Valsalva and sinotubular junction diameters (in diastole)
- Basal septal thickness (important for valve positioning)
- Assess:
- Left ventricular function (even severe dysfunction is not a contraindication)
- Mitral regurgitation (may improve post-TAVR, but persistent MR increases mortality)
- Tricuspid regurgitation and right heart function (unlikely to improve and linked to worse prognosis)
Post-TAVR Follow-Up
- Routine surveillance imaging recommended at:
- 30 days post-implant
- 1 year post-implant
- Annually thereafter
Follow-Up Echo Focus:
- Visual inspection of:
- Valve position and stability
- Leaflet appearance and movement
- Assessment of:
- Left ventricular function
- Severity of mitral regurgitation
- Doppler interrogation to:
- Record peak velocity and mean pressure gradient
- Calculate effective orifice area
- Ensure pulsed wave Doppler sample is placed below the valve stent (not within it) to avoid underestimation
Complications and Regurgitation
- Device migration: must confirm stable position
- Structural failure: rare with current TAVR devices
- Paravalvular regurgitation:
- Common and associated with long-term outcomes
- Often multiple jets, difficult to quantify due to acoustic shielding
- Assess using:
- Number of jets
- Vena contracta width
- Jet width as % of LVOT
- Flow reversal in the aortic arch
This is an edited excerpt from the Medmastery course Echo Masterclass – The Valves by Chris Eggett, PhD. Acknowledgement and attribution to Medmastery for providing course transcripts.
Additional echocardiography resources:
- Na, M. Echo Masterclass: Left Ventricular Strain. Medmastery
- Monteiro, C. Echo Masterclass: The Right Heart. Medmastery
- West, C. Echo Masterclass: Adult Congenital Heart Disease. Medmastery
- Naderi, H. Echo Masterclass: The Power of 3D Imaging. Medmastery
Radiology Library: Echocardiography basics
- Eggett C. Echo basics: Valve Views. LITFL
- Eggett C. Echo basics: Valves, Measurements and Reports. LITFL
- Eggett C. Echo basics: Mitral valve. LITFL
- Eggett C. Echo basics: Mitral Regurgitation. LITFL
- Eggett C. Echo basics: Mitral Stenosis. LITFL
- Eggett C. Echo basics: Aortic Valve. LITFL
- Eggett C. Echo basics: Aortic Stenosis. LITFL
- Eggett C. Echo basics: Aortic Regurgitation. LITFL
- Eggett C. Echo basics: Tricuspid Valve. LITFL
- Eggett C. Echo basics: Pulmonary Valve. LITFL
- Eggett C. Echo basics: Prosthetic Valves. LITFL
Further reading
- Otto CM. Textbook of Clinical Echocardiography. Elsevier. 7e, 2023.
- Houghton AR. Making Sense of Echocardiography: A Hands-on Guide. 3e 2023
- Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-e227.
Echocardiography Essentials
Cardiac physiologist, echocardiographer, and Professor of Healthcare Science Education, Faculty of Medical Sciences at the University of Newcastle, UK. I direct post-grad programs at the Faculty of Medical Sciences, run an echo clinic at the Freeman Hospital, and teach transthoracic echocardiography to specialists in critical and emergency care and anaesthetic settings

