Echo basics: Pulmonary Valve
Understand and identify the pulmonary valve. Learn how to identify and grade pulmonary regurgitation and quantify pulmonary stenosis. Basic management of pulmonary valve dysfunction.
Recognizing an Abnormal Pulmonary Valve
Overview
- Pulmonary valve abnormalities are most often due to congenital heart disease
- When identified in adults, they may reflect:
- Childhood surgical interventions
- Balloon dilatation procedures
- Less common adult causes include:
- Infective endocarditis
- Cardiac carcinoid disease
- Rheumatic disease
Echocardiographic Views for Pulmonary Valve Assessment
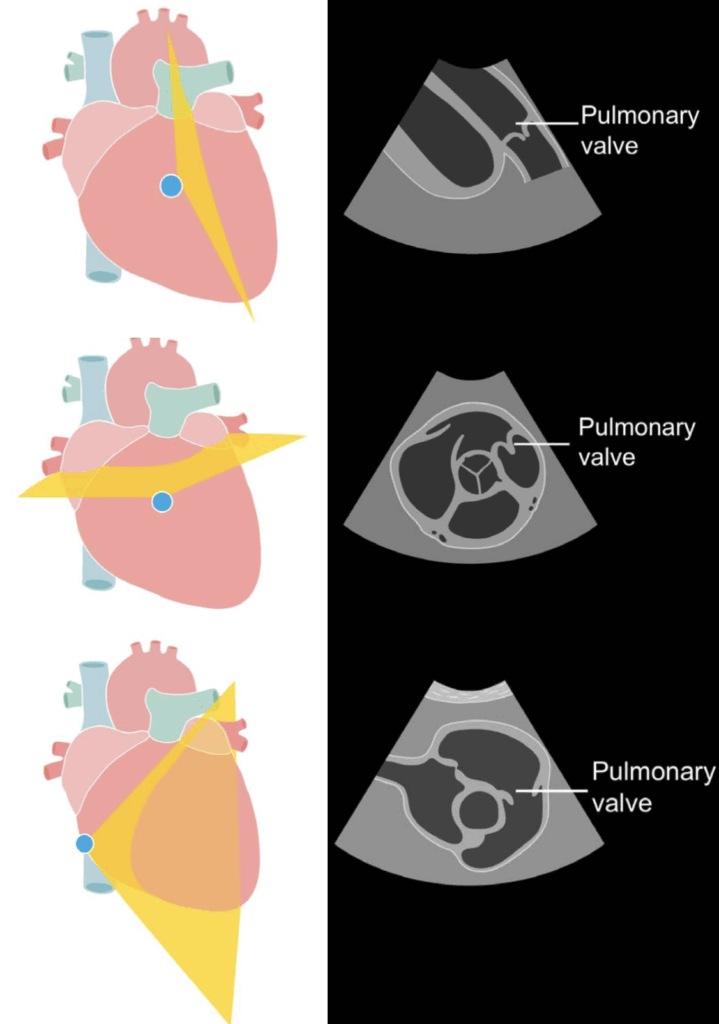
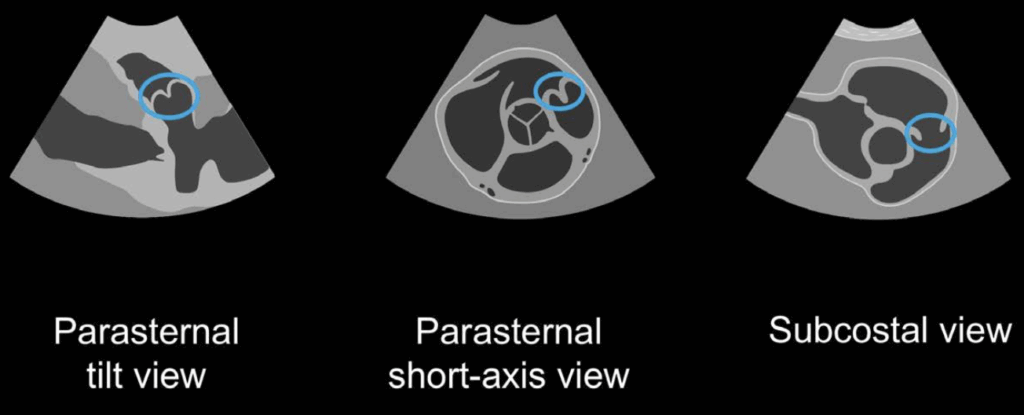
- Three standard transthoracic views:
- Parasternal long-axis right ventricular outflow tract (RVOT) view
- Parasternal short-axis view at the aortic valve level
- Subcostal short-axis approach
- Challenges:
- Only two valve leaflets typically visible on transthoracic echo
- Lung tissue interference limits imaging quality
- Valve anatomy difficult to confirm; leaflet identification often uncertain
Visual Features and Interpretation
- Pulmonary valve leaflets:
- Generally thinner than aortic valve leaflets (due to lower right-sided pressures)
- Visual inspection alone is unreliable, especially for:
- Determining the number of cusps
- Diagnosing mild forms of disease
Clues Suggestive of Pulmonary Valve Stenosis
- Thickened cusps seen on 2D echo may raise suspicion
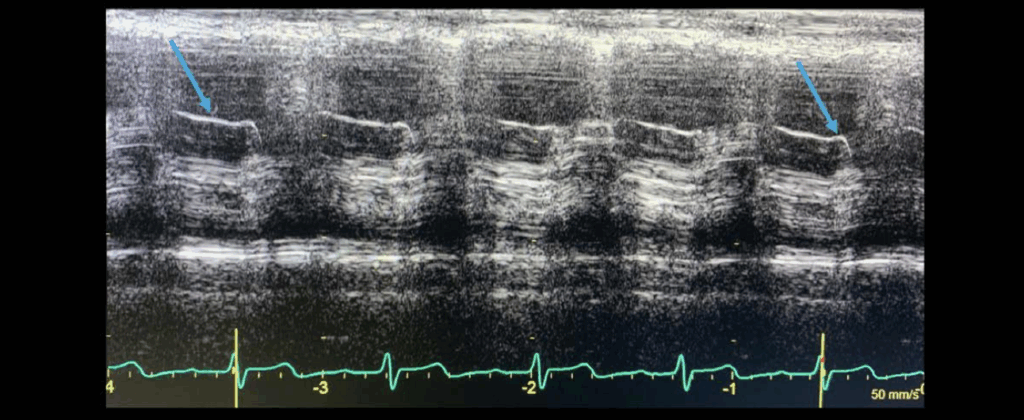
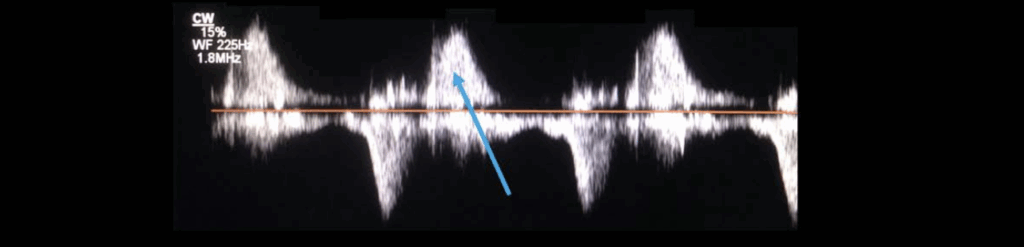
- M-mode echocardiography through the RVOT:
- May show increased signal density (brighter, thicker leaflet reflections)
- Increased ‘a wave’ notch may be visible:
- Occurs just before the QRS complex on ECG
- Suggests increased right atrial contraction force
- Indicates resistance from stenotic pulmonary valve
Grading Pulmonary Regurgitation
Doppler Assessment
- Use all three acoustic windows:
- Parasternal long-axis RVOT view
- Parasternal short-axis at aortic valve level
- Subcostal short-axis view
- Employ both:
- Colour flow Doppler
- Spectral (continuous wave) Doppler
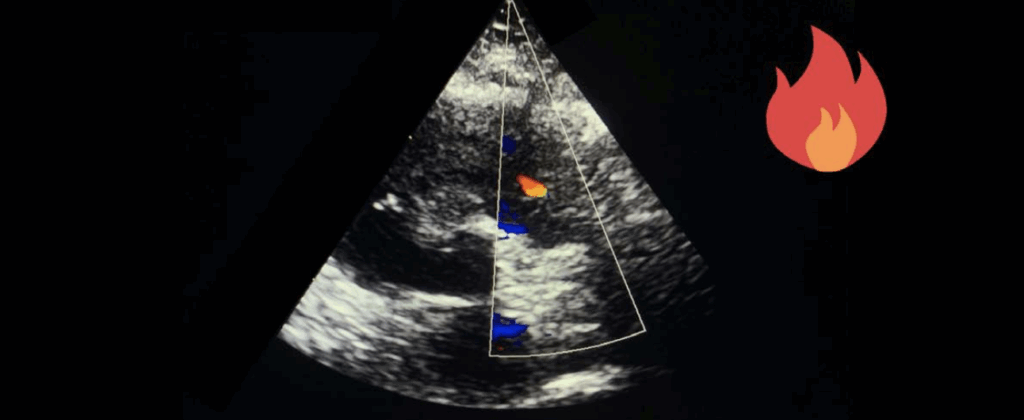
Normal vs Pathological Pulmonary Regurgitation
- Physiological/Functional regurgitation (common in healthy subjects):
- Narrow, short jet (< 10 mm)
- Red flame-like appearance
- Directed from pulmonary valve toward the right ventricle during diastole
- Pathologic regurgitation is often associated with:
- Pulmonary hypertension
- Valve or outflow tract abnormalities
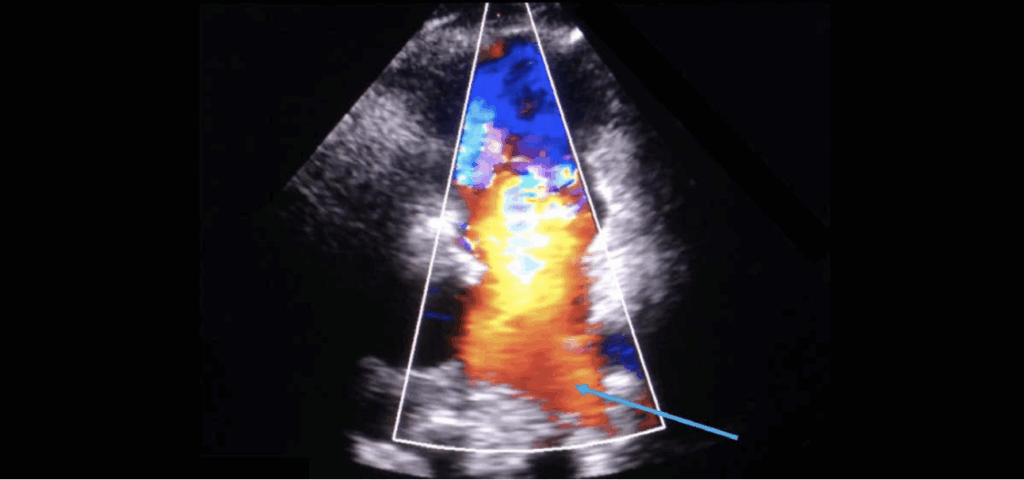
Colour Doppler Finding
- Key indicators of significant regurgitation:
- Wide jet origin just below the pulmonary valve
- Jet width covering ≥ 60% of the right ventricular outflow tract
- Colour flow reversal in pulmonary arteries (suggests severe regurgitation)
- Caution:
- Jet width may be artifactually increased due to viewing angle
- Severe regurgitation may show a short-duration jet due to rapid pressure equalization
Spectral Doppler Interpretation
- Parasternal short-axis view provides best alignment for continuous wave Doppler
- Waveform characteristics:
- Mild regurgitation:
- Weak, faint Doppler signal
- Long pressure half-time
- Severe regurgitation:
- Dense signal with steep deceleration slope
- Pressure half-time < 100 ms (especially in congenital heart disease)
- Mild regurgitation:
Limitations of Quantification
- Vena contracta and PISA (flow convergence) methods:
- Not validated for pulmonary valve assessment
- Rely primarily on:
- Qualitative Doppler analysis
- Jet width proportions
- Flow reversal patterns
Assessing Pulmonary Valve Stenosis
Imaging Approach
- Use all available transthoracic views to assess the pulmonary valve and right ventricular outflow tract (RVOT)
- Employ both:
- Continuous wave Doppler: to capture maximum antegrade velocities
- Pulsed wave Doppler: to localize the site of obstruction
- Colour Doppler: to visualize flow acceleration and narrowing
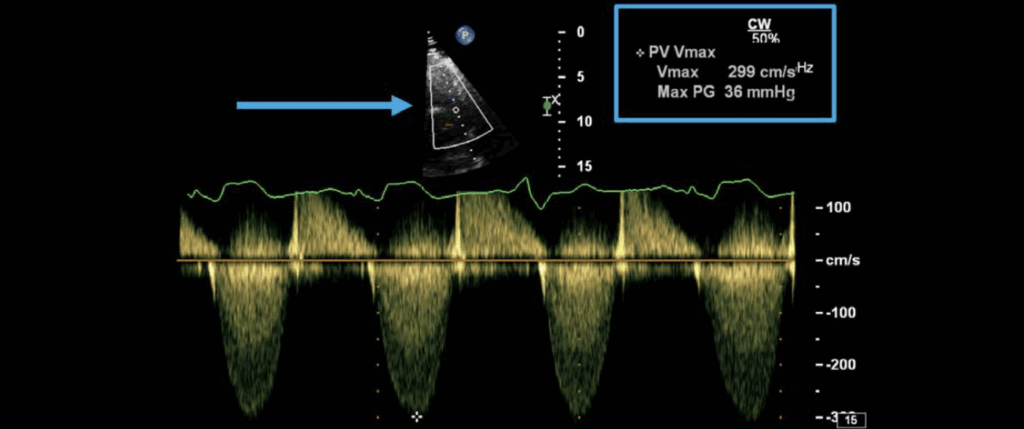
Doppler Velocity Thresholds
- Normal pulmonary valve velocity: ~ 1.0 m/s
- Mild stenosis: Peak velocity < 3.0 m/s
- Severe stenosis: Peak velocity > 4.0 m/s
Use the simplified Bernoulli equation to calculate the pressure gradient from peak velocity
ΔP = 4 × (V²)
Differentiating Valve vs. Outflow Tract Stenosis
- Be aware that increased velocity may not always originate from the valve itself:
- Subvalvular stenosis (e.g. RVOT narrowing)
- Supravalvular stenosis (e.g. pulmonary artery stenosis)
- Use pulsed wave Doppler to:
- Identify the point where velocity increases (“step-up” point)
- Help differentiate valve-level stenosis from other causes
- Colour Doppler can:
- Assist in localizing the anatomical level of the narrowing
- Demonstrate turbulent or accelerated flow across narrowed segments
Managing a Patient with Pulmonary Valve Disease
Intervention Options
- Balloon Pulmonary Valvuloplasty
- First-line treatment for moderate to severe isolated pulmonary stenosis
- Safe and effective for reducing valve gradient and improving symptoms
- Surgical Valvotomy
- Considered if balloon valvuloplasty is unsuitable
- Appropriate when valve and annulus are not significantly malformed
- Pulmonary Valve Replacement
- Required when:
- Severe malformation of valve or annulus
- Significant regurgitation or right ventricular dysfunction post-repair
- Required when:
Follow-Up and Monitoring
- Mild native pulmonary stenosis:
- Typically does not require intervention
- Regular echocardiographic follow-up is sufficient
- Post-intervention surveillance:
- Required for all patients who underwent:
- Balloon valvuloplasty
- Surgical repair
- Focus of follow-up:
- Pulmonary regurgitation
- Right ventricular size and function
- Required for all patients who underwent:
Pulmonary Regurgitation After Congenital Repair
- Tetralogy of Fallot repair:
- Pulmonary regurgitation is a common late complication
- May lead to:
- Right ventricular dilation
- Arrhythmias
- Tricuspid regurgitation
- Impaired exercise tolerance
- Surgical valve replacement should be considered when:
- Moderate/severe regurgitation is symptomatic
- Right ventricular dilation and dysfunction are present
- Associated arrhythmias or significant tricuspid regurgitation occur
Timing of Valve Replacement
- Evidence for ideal timing is not definitive
- Goal: Prevent irreversible right ventricular dysfunction
- Valve replacement may stabilize or improve RV function if performed before advanced failure
This is an edited excerpt from the Medmastery course Echo Masterclass – The Valves by Chris Eggett, PhD. Acknowledgement and attribution to Medmastery for providing course transcripts.
Additional echocardiography resources:
- Na, M. Echo Masterclass: Left Ventricular Strain. Medmastery
- Monteiro, C. Echo Masterclass: The Right Heart. Medmastery
- West, C. Echo Masterclass: Adult Congenital Heart Disease. Medmastery
- Naderi, H. Echo Masterclass: The Power of 3D Imaging. Medmastery
Radiology Library: Echocardiography basics
- Eggett C. Echo basics: Valve Views. LITFL
- Eggett C. Echo basics: Valves, Measurements and Reports. LITFL
- Eggett C. Echo basics: Mitral valve. LITFL
- Eggett C. Echo basics: Mitral Regurgitation. LITFL
- Eggett C. Echo basics: Mitral Stenosis. LITFL
- Eggett C. Echo basics: Aortic Valve. LITFL
- Eggett C. Echo basics: Aortic Stenosis. LITFL
- Eggett C. Echo basics: Aortic Regurgitation. LITFL
- Eggett C. Echo basics: Tricuspid Valve. LITFL
- Eggett C. Echo basics: Pulmonary Valve. LITFL
- Eggett C. Echo basics: Prosthetic Valves. LITFL
Further reading
- Otto CM. Textbook of Clinical Echocardiography. Elsevier. 7e, 2023.
- Houghton AR. Making Sense of Echocardiography: A Hands-on Guide. 3e 2023
- Robbins A, Zhang G, Cadogan M. Eponymic Cardiac Murmurs. LITFL
- Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-e227.
Echocardiography Essentials
Cardiac physiologist, echocardiographer, and Professor of Healthcare Science Education, Faculty of Medical Sciences at the University of Newcastle, UK. I direct post-grad programs at the Faculty of Medical Sciences, run an echo clinic at the Freeman Hospital, and teach transthoracic echocardiography to specialists in critical and emergency care and anaesthetic settings

