Echo basics: Tricuspid Valve
Understand and identify the tricuspid valves. Learn how to identify and grade tricuspid regurgitation and quantify tricuspid stenosis. Basic management of tricuspid valve dysfunction.
Recognizing Abnormal Tricuspid Valves
Initial Visualization
- The parasternal tilt view (from the parasternal long-axis position) is typically the first opportunity to visualize the tricuspid valve:
- Angle the probe inferiorly and rightward (towards the patient’s right hip).
- Brings into view: right atrium, tricuspid valve, and right ventricle.
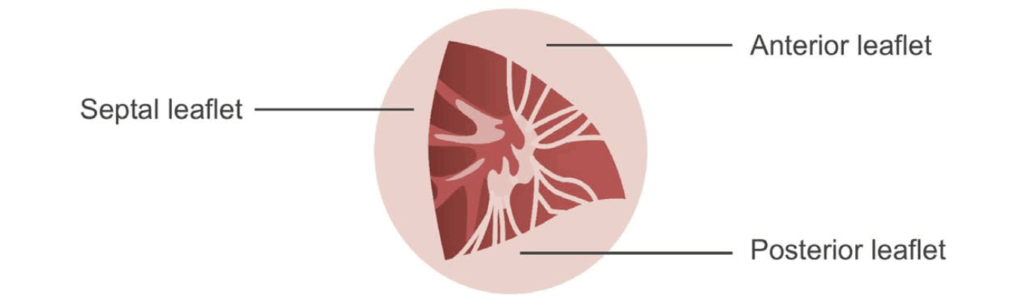
Valve Anatomy Overview
- Largest of the four valves, with three leaflets:
- Anterior
- Septal
- Posterior
- Subvalvular apparatus includes:
- Fibrous annulus
- Chordae tendineae
- Papillary muscles
🧠 Note: Leaflet identification is variable between views and highly dependent on transducer angulation.
Parasternal Tilt View
- Most commonly shows:
- Anterior and septal leaflets
- Inferior angulation may reveal:
- Anterior and posterior leaflets
- Two papillary muscles may be seen.
- The moderator band often attaches near the anterior papillary muscle.

Parasternal Short-Axis View (at Aortic Valve Level)
- Typically shows:
- Posterior and septal leaflets
- May occasionally show:
- Anterior leaflet, depending on probe orientation
Apical Four-Chamber View
- Provides a clear image of:
- Septal leaflet (adjacent to interventricular septum)
- Free wall-attached leaflet may be anterior or posterior, depending on:
- Probe angulation
- Probe rotation
- The tricuspid valve annulus is:
- Closer to the apex than the mitral valve annulus
- Normal offset from mitral valve ≤ 10 mm

Subcostal View
- Challenging but valuable view.
- Technique:
- Start from the subcostal four-chamber view
- Rotate the probe 90° counterclockwise
- Center on the right ventricle
- Goal: Short-axis “enface” view showing all three leaflets
Doppler Assessment
- Best views for Doppler interrogation:
- Apical four-chamber
- Parasternal tilt
- Spectral Doppler:
- Similar pattern to mitral inflow
- Lower peak velocities due to:
- Lower pressure gradient between the right atrium and right ventricle

Identifying and Grading Tricuspid Regurgitation
Pathophysiology
- Normal tricuspid valve function depends on the integrity of:
- Valve leaflets
- Subvalvular apparatus
- Tricuspid annulus
- Right atrium and ventricle
- Regurgitation results when one or more components are dysfunctional.
Types of Tricuspid Regurgitation
- Trivial/mild regurgitation is common and usually appears as a small, central jet.
- Organic (primary) causes:
- Endocarditis
- Carcinoid heart disease
- Trauma
- Radiation
- Pacemaker or defibrillator leads
- Functional (secondary) causes:
- Usually due to left-sided heart disease
- Associated with:
- Right-sided heart failure
- RV dilation
- RA dilation
- Pulmonary hypertension
- Tricuspid annular dilation
Imaging Evaluation Strategy
- Use multiple views (e.g., parasternal, apical, subcostal) with:
- Colour Doppler
- Spectral Doppler
- Pulsed wave Doppler (esp. in hepatic veins)
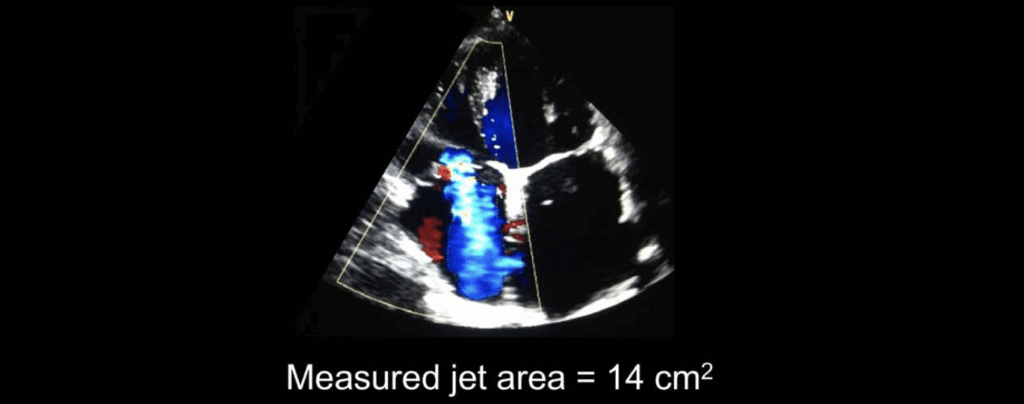
Semi-Quantitative Measures
- Regurgitant jet area:
- 10 cm² in RA suggests severe regurgitation
- ⚠ Note: May underestimate severity when RV–RA pressure gradient is low (e.g., in torrential TR)
- Vena contracta width:
- Measured in parasternal RV inflow or apical four-chamber view
- 7 mm indicates severe TR
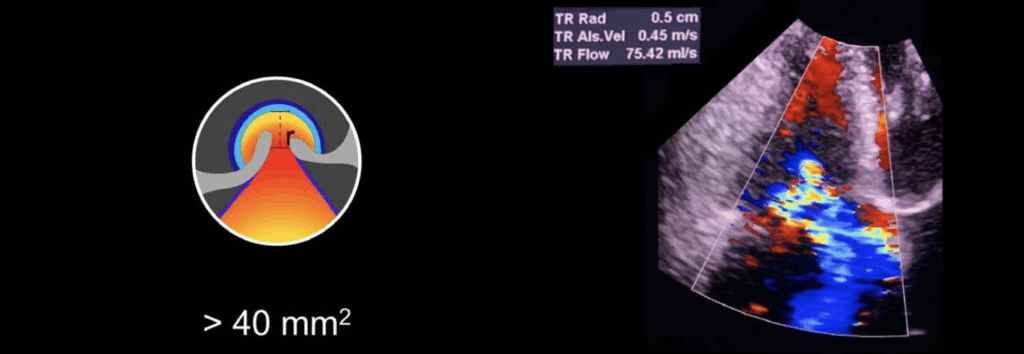
- Flow convergence (PISA):
- Limited by low flow and non-circular orifice shape
- EROA > 40 mm² is consistent with severe TR
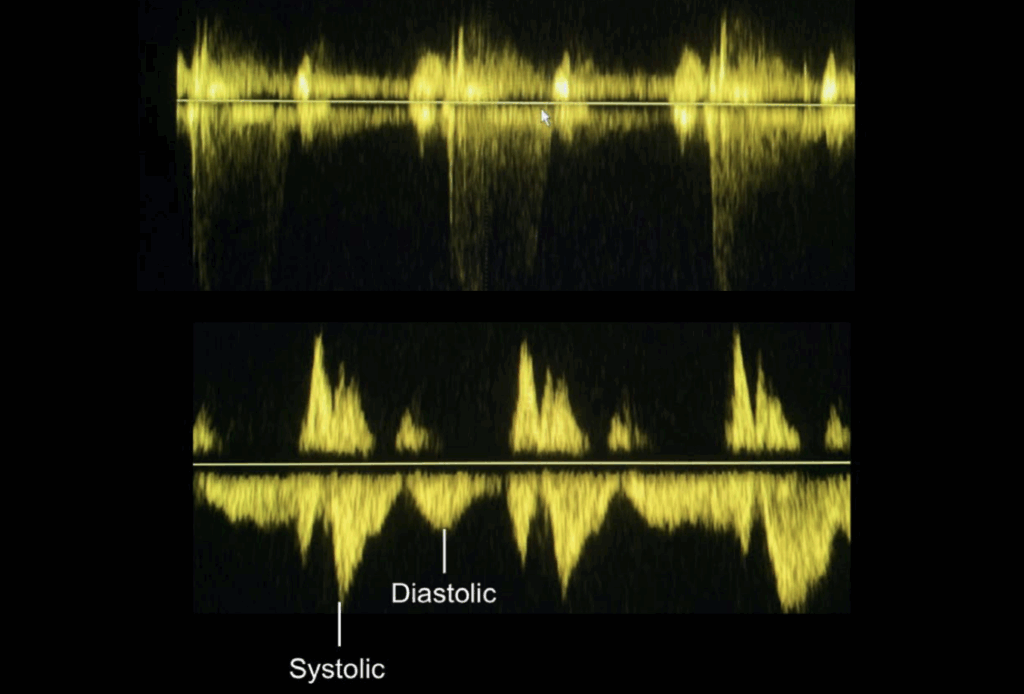
Spectral Doppler Evaluation
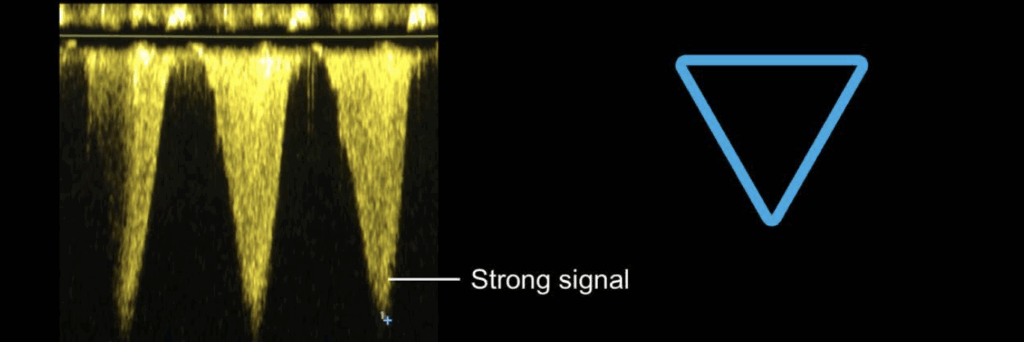
- Continuous wave Doppler:
- Dense, triangular-shaped jet implies severe TR
- Pulsed wave Doppler in hepatic veins:
- Systolic flow reversal is a hallmark of severe TR
Grading Summary
| Parameter | Mild TR | Severe TR |
|---|---|---|
| Colour jet area | Small, central | > 10 cm² (may underestimate) |
| Vena contracta | < 7 mm | > 7 mm |
| Effective regurgitant orifice (EROA) | — | > 40 mm² |
| CW Doppler waveform | Faint | Dense, triangular |
| Hepatic vein flow | Normal | Systolic flow reversal |
Clinical Integration
- Begin with semi-quantitative assessment
- If uncertainty remains, use quantitative methods
- Functional TR may progress; monitor with serial imaging if significant RV dilation or pulmonary hypertension is present
Assessing Tricuspid Valve Stenosis
Overview
- Organic tricuspid stenosis is rare but should be considered in:
- Patients with a history of rheumatic fever
- Especially when rheumatic mitral stenosis is also present
- Other causes of organic stenosis include:
- Carcinoid heart disease
- Antiphospholipid syndrome
- Ebstein’s anomaly
Functional Tricuspid Stenosis
- May result from intracardiac thrombus or masses
- Consider in patients with cardiac devices, including:
- Pacing leads across the tricuspid valve
- Septal closure devices (e.g., for PFO or ASD), especially if mispositioned
Visual Inspection
- Thickened tricuspid leaflets are often difficult to visualise reliably
- However, stenosis due to device interference may be detected visually
- Use multiple views, especially apical four-chamber and subcostal windows
Doppler Assessment
- Continuous wave Doppler is the primary modality for hemodynamic assessment
- Optimal imaging usually via the apical four-chamber view
- Use to assess forward flow velocities and waveform shape
Diagnostic Criteria
- Mean pressure gradient across the tricuspid valve:
- 5 mmHg is consistent with significant tricuspid stenosis
- Pressure half-time:
- 190 ms suggests severe tricuspid stenosis
Summary Table
| Parameter | Diagnostic Threshold |
|---|---|
| Mean pressure gradient | > 5 mmHg → Significant stenosis |
| Pressure half-time (PHT) | > 190 ms → Severe stenosis |
Patient Management: Tricuspid Valve Disease
Initial Echocardiographic Assessment
- Transthoracic echocardiography (TTE) is the first-line tool to:
- Assess valve anatomy
- Determine severity of tricuspid regurgitation
- Evaluate right atrial and ventricular size/function
- Measure inferior vena cava (IVC) dimensions
- Estimate pulmonary artery systolic pressure (PASP)
- Perform comprehensive left heart assessment, including the mitral valve
Prognosis and Recognition
- Severe tricuspid regurgitation (TR) carries a poor prognosis if left untreated
- Under-treatment is common due to:
- Lack of awareness about TR significance
- Limited understanding of intervention options
Surgical and Interventional Recommendations
Tricuspid Stenosis
- Class I indication for surgical intervention when:
- Severe tricuspid stenosis is present
- Patient is undergoing left-sided valve surgery
- Surgery is recommended for:
- Symptomatic patients with isolated severe tricuspid stenosis
- Percutaneous balloon commissurotomy may be considered if:
- Severe stenosis is present without significant TR
Tricuspid Regurgitation (TR) Management
Surgical Repair
- Repair is recommended in the following scenarios:
- Mild or greater functional TR during left-sided valve surgery, with:
- Tricuspid annular dilation
- Evidence of right heart failure
- Moderate functional TR with pulmonary hypertension during left-sided valve surgery
- Mild or greater functional TR during left-sided valve surgery, with:
- Repair may be considered for:
- Symptomatic patients with severe primary TR unresponsive to medical therapy
- Asymptomatic or minimally symptomatic patients with:
- Severe primary TR and
- Right ventricular dilation or dysfunction
Surgical and Transcatheter Techniques
Surgical Approaches
- Tricuspid valve repair:
- Typically involves annuloplasty ring insertion to restore annular size and shape
- Valve replacement:
- Bioprosthetic valves preferred over mechanical due to lower thromboembolic risk
- Limitations:
- High perioperative mortality rates associated with tricuspid valve surgery
Transcatheter Interventions
- Rapidly evolving field due to high surgical risk in many patients
- Current percutaneous approaches include:
- Valve replacement
- Annuloplasty techniques
- Coaptation devices
- Challenges:
- Anatomical complexity of tricuspid valve
- Lack of robust anchoring structures
- Large annular dimensions
This is an edited excerpt from the Medmastery course Echo Masterclass – The Valves by Chris Eggett, PhD. Acknowledgement and attribution to Medmastery for providing course transcripts.
Additional echocardiography resources:
- Na, M. Echo Masterclass: Left Ventricular Strain. Medmastery
- Monteiro, C. Echo Masterclass: The Right Heart. Medmastery
- West, C. Echo Masterclass: Adult Congenital Heart Disease. Medmastery
- Naderi, H. Echo Masterclass: The Power of 3D Imaging. Medmastery
Radiology Library: Echocardiography basics
- Eggett C. Echo basics: Valve Views. LITFL
- Eggett C. Echo basics: Valves, Measurements and Reports. LITFL
- Eggett C. Echo basics: Mitral valve. LITFL
- Eggett C. Echo basics: Mitral Regurgitation. LITFL
- Eggett C. Echo basics: Mitral Stenosis. LITFL
- Eggett C. Echo basics: Aortic Valve. LITFL
- Eggett C. Echo basics: Aortic Stenosis. LITFL
- Eggett C. Echo basics: Aortic Regurgitation. LITFL
- Eggett C. Echo basics: Tricuspid Valve. LITFL
- Eggett C. Echo basics: Pulmonary Valve. LITFL
- Eggett C. Echo basics: Prosthetic Valves. LITFL
Further reading
- Otto CM. Textbook of Clinical Echocardiography. Elsevier. 7e, 2023.
- Houghton AR. Making Sense of Echocardiography: A Hands-on Guide. 3e 2023
- Robbins A, Zhang G, Cadogan M. Eponymic Cardiac Murmurs. LITFL
- Huttin O, Voilliot D, Mandry D, Venner C, Juillière Y, Selton-Suty C. All you need to know about the tricuspid valve: Tricuspid valve imaging and tricuspid regurgitation analysis. Arch Cardiovasc Dis. 2016 Jan;109(1):67-80.
- Hahn RT. State-of-the-Art Review of Echocardiographic Imaging in the Evaluation and Treatment of Functional Tricuspid Regurgitation. Circ Cardiovasc Imaging. 2016 Dec;9(12):e005332.
- Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM 3rd, Thompson A, Toly C. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2021 Feb 2;143(5):e72-e227.
Echocardiography Essentials
Cardiac physiologist, echocardiographer, and Professor of Healthcare Science Education, Faculty of Medical Sciences at the University of Newcastle, UK. I direct post-grad programs at the Faculty of Medical Sciences, run an echo clinic at the Freeman Hospital, and teach transthoracic echocardiography to specialists in critical and emergency care and anaesthetic settings

