Eponymous Hernia
A hernia is the protrusion of a viscus or tissue through the wall of the cavity that normally contains it. Clinically we separate external (e.g., inguinal, femoral, umbilical, ventral/incisional, Spigelian) from internal/diaphragmatic (e.g., hiatal, para-oesophageal, Bochdalek, Morgagni), then describe site, sac contents, and status (reducible, incarcerated, strangulated).
Eponymous hernias capture what’s inside the sac (e.g., Amyand (appendix: inguinal hernia); de Garengeot (appendix: femoral hernia); Littre (Meckel’s diverticulum)) or where the defect lies (e.g., Spigelian, Bochdalek, Morgagni). The eponym is a convenient label; the safe description is anatomical: state the location, contents, and complications, then add the eponym if it adds clarity.
Etymology: hernia from Latin hernia (“rupture”); inguinal from Latin inguen (“groin”); femoral from Latin femur (“thigh”).
Amyand’s hernia (1735)
Amyand’s hernia describes the presence of the vermiform appendix within an inguinal hernia sac, whether inflamed or not. Case reports range from incidental finding to incarcerated hernia with appendicitis or perforation. Management depends on appendix status (normal vs inflamed) and degree of contamination; mesh is avoided in infected fields.
Reported prevalence of Amyand’s hernia is 0.4–0.6% of all inguinal hernias, with appendicitis within an Amyand hernia in ~0.07–0.13%. In children, prevalence may reach ~1%. There is a male predominance (≈90% in reviews) and often right-sided due to anatomical predisposition.
At operation, Amyand found a perforated appendix (penetrated by a swallowed pin); within the inguinal canal which he excised, making this the first documented appendicectomy.
- Claudius Amyand (c.1680-1740) was a French-born English surgeon
- Amyand C. Of an inguinal rupture, with a pin in the appendix caeci, incrusted with stone; and some observations on wounds in the guts. Phil. Trans. R. Soc., 1736, 39: 329-336
Bochdalek hernia (1848)
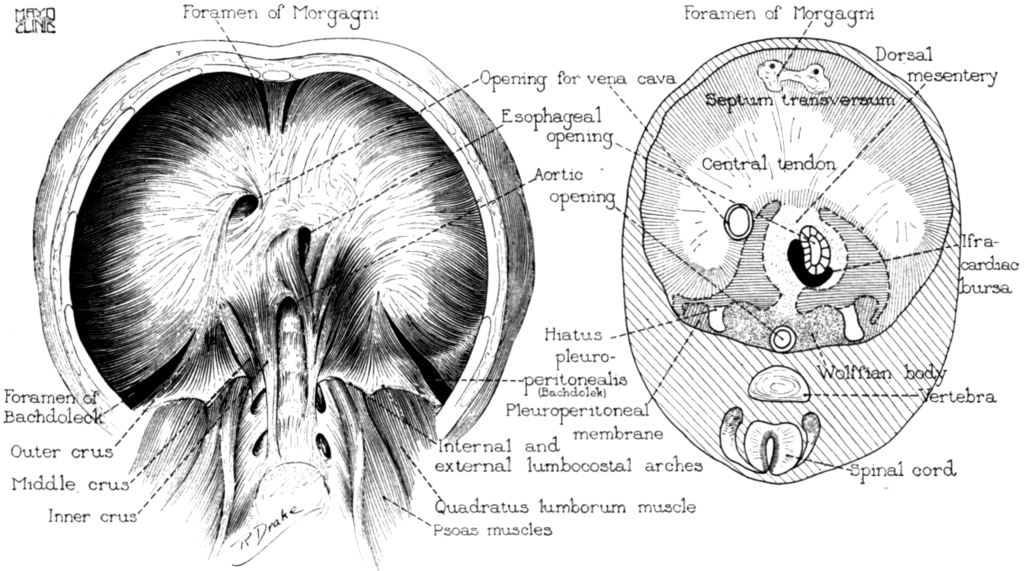
A Bochdalek hernia is a congenital, posterolateral diaphragmatic defect that allows abdominal viscera to herniate into the thorax, compressing the developing lung and leading to pulmonary hypoplasia and neonatal respiratory compromise. The defect reflects failed closure of the pleuroperitoneal canal during embryogenesis.
1848 – Bochdalek provided the first description of a posterior diaphragmatic defect (Bochdalek foramen) with herniation causing neonatal death. He proposed a mechanism for herniation and went on to predict that surgery would be able to repair the defect in the future.
Diese Lücke … welche ich die hintere Zwerchfelllücke nennen will, befindet sich zwischen dem äußeren oder dritten Schenkel des Lendenteils des Zwerchfells, der letzten fleischigen Zacke seines Rippenteils, und der letzten falschen Rippe. Sie hat meist die Gestalt eines Dreieckesder zwischen diesen Rändern eingeschlossene Raum
… ist mittelst eines Hautblattes verschlossen, welches aus zwei Schichten besteht. Die obere Schicht rührt vom Brustfelle her … die untere Schichte ist sehnicht, eine Fortsetzung der Fascia iliaca …Gewöhnlich ist die der linken Seite etwas umfangreicher als die der rechten.
Bei der … Tatsache, daß ein rein häutiges Gebilde weniger widerstandsfähig ist … geschieht es … daß die häutige Lücke dem Andrange der Baucheingeweide geringeren Widerstand … leistet; deshalb wird … [sie] ausgedehnt … in den Brusthöhlenraum erhoben und so zu einem förmlichen Bruchsack gestaltet. – Bochdalek 1848
This gap, which I propose to call the posterior diaphragmatic gap, lies between the outer (third) crus of the lumbar part of the diaphragm, the last muscular digitations of its costal part, and the last false rib. It is usually triangular in shape…
The space enclosed by these borders is closed by a membranous sheet composed of two layers: the upper derives from the pleura, the lower is tendinous, a continuation of the fascia iliaca…Usually the gap on the left side is somewhat larger than that on the right.
Because a purely membranous structure is less resistant, this membranous gap offers reduced opposition to the pressure of the abdominal viscera; it is therefore stretched, protrudes into the thoracic cavity, and becomes a true hernial sac. – Bochdalek 1848
- Vincenz Alexander Bochdalek (1801–1883) was a Czech anatomist and pathologist
- Bochdalek VA. Einige Betrachtungen über die Entstehung des angeborenen Zwerchfellbruches als Beitrag zur pathologischen Anatomie der Hernien. Vierteljahrschrift für die praktische Heilkunde. (Prag) 1848; 19: 89
De Garengeot’s Hernia (1731)
De Garengeot’s hernia refers to a femoral hernia containing the vermiform appendix
1731 – Garengeot described a 55-year-old woman who developed a painful right groin swelling after lifting bread. At operation, a femoral hernia was found containing the appendix, which was reduced and the patient recovered.
…Je trouvai dans le sac herniaire un petit corps allongé, adhérent, que je reconnus pour l’appendice du caecum. Je le remis dans le ventre, et après avoir pratiqué la cure ordinaire de la hernie, la malade se rétablit – de Garengeot, 1731
…I found in the hernial sac a small elongated body, adherent, which I recognised as the appendix of the caecum. I returned it into the abdomen, and after carrying out the usual cure of the hernia, the patient recovered – de Garengeot, 1731
- René-Jacques Croissant de Garengeot (1688-1759) was a French surgeon
- De Garengeot RJC. Traité des opérations de chirurgie, fondé sur la mécanique des organes de l’homme, et sur la théorie et la pratique la plus autorisée. 1731, 2e [Hernia: 369–371]
Littré’s Hernia (1700)
Littré’s hernia refers to the protrusion of a Meckel’s diverticulum into a hernial sac. Though very rare, it carries clinical importance because of its risk of strangulation, necrosis, and perforation. The condition has been reported in less than 0.1% of all strangulated or incarcerated hernias. Reported sites include inguinal (~50%), femoral (~20%), umbilical (~20%), and rare parastomal cases.
Patients typically present with a painful hernial swelling, and diagnosis is often made intraoperatively. Surgical management consists of excision of the diverticulum and definitive hernia repair, with mesh repair avoided in contaminated fields.
1700 – Littré described his Observations sur une nouvelle espèce de hernie, which were published in the Histoire de l’Académie Royale des Sciences in 1719. He reported post-mortem cases where a small portion of ileum formed a diverticulum and extended into the hernia sac.
Une nouvelle espèce de hernie… formée par une petite portion de l’intestin grêle, prolongée en dehors du tube, comme une espèce de vessie, et tombant dans la poche herniaire – Littré, 1700
A new kind of hernia… formed by a small portion of the small intestine, prolonged outward from the tube like a kind of bladder, and falling into the hernial sac. – Littré, 1700
1809 – Johann Friedrich Meckel (the younger) (1781-1833) established the congenital nature of the outpouchings (Meckel’s diverticulum), recognising them as embryological remnants of the vitelline duct.
- Alexis Littré (1654-1726) was a French anatomist and surgeon
- Littre A. Observations sur une nouvelle espèce de hernie. Histoire de l’Académie royale des sciences avec les Mémoires de mathematique et de physique. 1700: 300-310
Maydl’s hernia (1898)
A rare form of strangulated internal hernia in which two adjacent bowel loops lie within the hernia sac, while the central intra-abdominal loop becomes strangulated, also known as the “W-shaped hernia”. Estimated to occur in 2–10% of strangulated hernias found more frequently in inguinal hernias, but also in femoral and incisional sites. Mortality in older case series was high (up to 40–50%), but outcomes improved with earlier recognition and resection.
High risk of missed diagnosis as the external hernia sac may appear viable while the intra-abdominal loop is necrotic. Recognising the “W-configuration” intraoperatively is crucial and resection of the central loop is required, not just reduction of the visible hernia.
1895–1898, Maydl described the condition and presented his cases in Prager medizinische Wochenschrift. He highlighted the clinical paradox that the strangulated, ischaemic loop lies within the abdominal cavity, while the hernia sac itself may appear only partially compromised. Failure to recognise this concealed intra-abdominal strangulation leads to delayed diagnosis and high mortality.
Ich habe unter meinen Bruchoperationen zwei Fälle beobachtet, in denen eine W-förmige Lage der Darmschlingen vorlag. Die beiden äußeren Schlingen lagen im Bruchsacke, die mittlere war im Abdomen zurückgeblieben, und gerade diese innere Schlinge verfiel zuerst der Gangrän – Maydl 1898
In my hernia operations I have observed two cases in which there was a W-shaped arrangement of the intestinal loops. The two outer loops lay in the hernia sac, the middle remained within the abdomen, and it was precisely this inner loop that first fell into gangrene – Maydl 1898
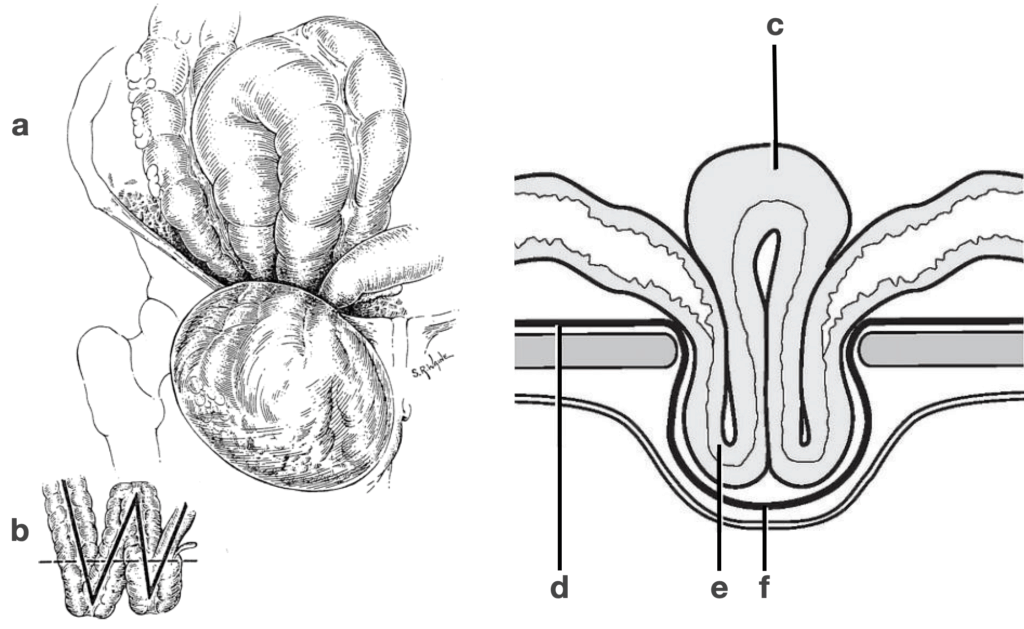
Obstructed loop of intestine within peritoneal cavity d) Peritoneum e) Hernia contents f) Hernia sac
- Karel Maydl (1853-1903) was a Czech surgeon
Morgagni hernia (1761)
Morgagni hernia is a congenital diaphragmatic hernia (CDH) accounting for 2–5% of CDH. An anterior, retrosternal congenital diaphragmatic defect through the sternocostal (parasternal) triangle (foramen of Morgagni). In comparison to Bochdalek hernia, a Morgagni hernia is more anterior and more often right-sided (~90%) and often discovered later in childhood or adulthood. Associated congenital anomalies are reported in 34–50%, especially cardiac defects (25–60%) and trisomy 21 (15–71%).
Frequently associated with a hernia sac, contents commonly include omentum and transverse colon, occasionally stomach, small bowel, or liver. Most patients are asymptomatic. Symptomatic cases present with chest/abdominal pain, dyspnoea, nausea/vomiting, or features of incarceration/volvulus.
Chest XR may show a paracardiac mass/air–fluid level at the right cardiophrenic angle. CT accurately defines the retrosternal defect and contents and can reach near-100% detection.
Repair is recommended for all due to incarceration risk; approach (open/laparoscopic; abdominal vs thoracic) is tailored to patient and contamination.
1761 – Morgagni first described the sternocostal gap in Tomus III, Liber IV, Epistola LIV, Article XI (“De vulneribus et contusionibus abdominis, lumborum, & membrorum”. he describes an anterior parasternal interval between xiphoid and adjacent fibres as a route for abdominal viscera into the thorax and also notes congenital diaphragmatic defects
Yet whenever the stomach is carried up through the diaphragm into the thorax, … there certainly are places in the diaphragm, through which… [a viscus] may pass over from the belly into the thorax… Thus also, anteriorly, betwixt the fibres that come from the xiphoid cartilage and the neighbouring fibres, there generally is an interval through which something similar may happen; and I even suspected this to have happen’d in a husbandman…
What symptoms an infant of two months old was troubled with… in whom, after death, almost all the intestines… were carried up into the thorax, through a foramen formed by nature in the diaphragm, on the left side of the foramen of the gullet…
Morgagni, 1761
- Giovanni Battista Morgagni (1682-1771) was an Italian physician, anatomist and pathologist.
- Morgagni GB. De vulneribus et contusionibus abdominis, lumborum, & membrorum Tomus III, Liber IV, Epistola LIV, Article XI 1761
Richter’s Hernia (1778)
Richter’s hernia is an abdominal hernia in which only a portion of the bowel wall is trapped at a small, rigid defect and may strangulate without full obstruction. It most often involves the distal ileum, but any segment from stomach to colon may be involved. The prerequisite is a defect large enough to nip the bowel wall yet too small to admit an entire loop, with a firm rim.
Accounts for 5–15% of strangulated hernias overall occurring more commonly in older adults (but any age possible). Most frequent sites are the femoral ring, then inguinal and incisional sites.
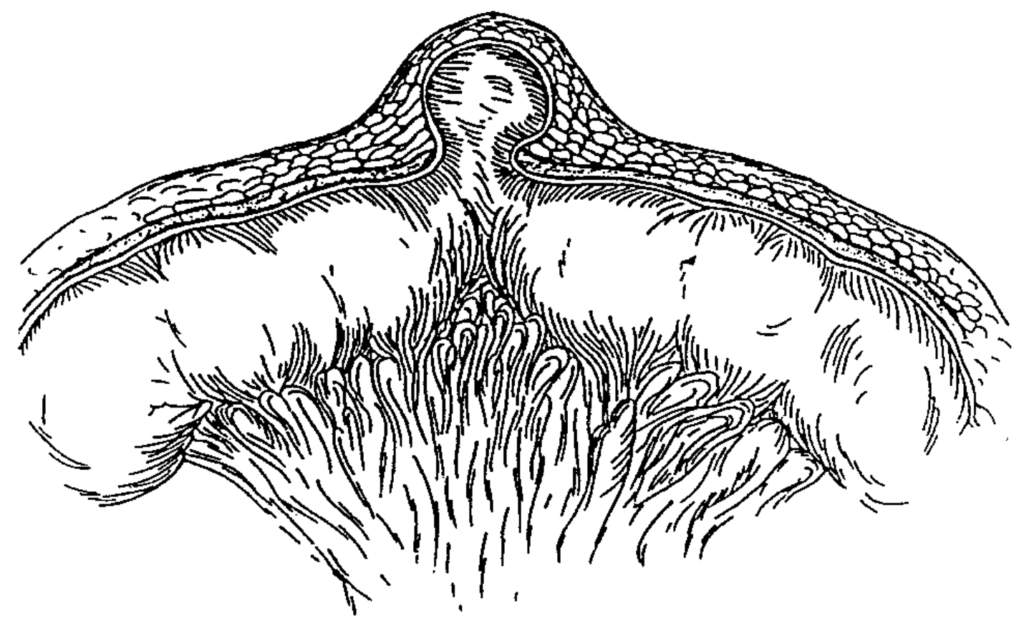
Richter’s Hernia. Steinke, 2000
Because <2/3 of the circumference is usually involved, complete obstruction is often absent, and presentation may be deceptively mild (localized tenderness, nausea/vomiting, ±low-grade symptoms) until strangulation/ischaemia evolves. Segmental necrosis is common (up to 69% at operation in one series).
1778 – Richter described a type of strangulated hernia in which only part of the circumference of the intestinal wall is entrapped in the hernia ring, leaving the lumen partially patent. This often led to subtle clinical signs but high risk of strangulation and gangrene.
Nur ein Theil des Darmumfanges wird eingeklemmt, der Stuhlgang bleibt möglich, und doch verfällt das eingeklemmte Stück in die Brandigkeit. – Richter 1785
Only a part of the intestinal circumference is constricted; stool may still pass, yet the constricted portion falls into gangrene – Richter 1785
- August Gottlieb Richter (1742-1812) was a German surgeon
- Richter AG. Einklemmung des Darms In: Abhandlung von den Brüchen. 1778
Spigelian Hernia
A Spigelian hernia is protrusion of peritoneum/abdominal contents through a defect in the Spigelian fascia (between the internal oblique and transversus abdominis aponeuroses) along the linea semilunaris. Most defects occur near or below the arcuate line within the so-called Spigelian belt (6 cm band above the interspinous line), where the posterior rectus sheath thins and creates a physiologic weak zone.
1627 – Spiegel first described the anatomy of the linea semilunaris (Spigelian Line) and Spigelian fascia, based on the plates of his predecessor Giulio Casseri (1552–1616), in Liber III, Caput IV–VI of De humani corporis fabrica libri decem (1627).
1764 – Joseph Thaddaeus Klinkosch (1735-1778), a Flemish anatomist and lecturer at the University of Padua defines ventral hernia and its sites. He identified the semilunar line as a weak/aponeurotic zone and explicitly lists hernias occurring in “linea semilunari.”. He does not cite Spiegel and was not the first to use the name Spigelian hernia
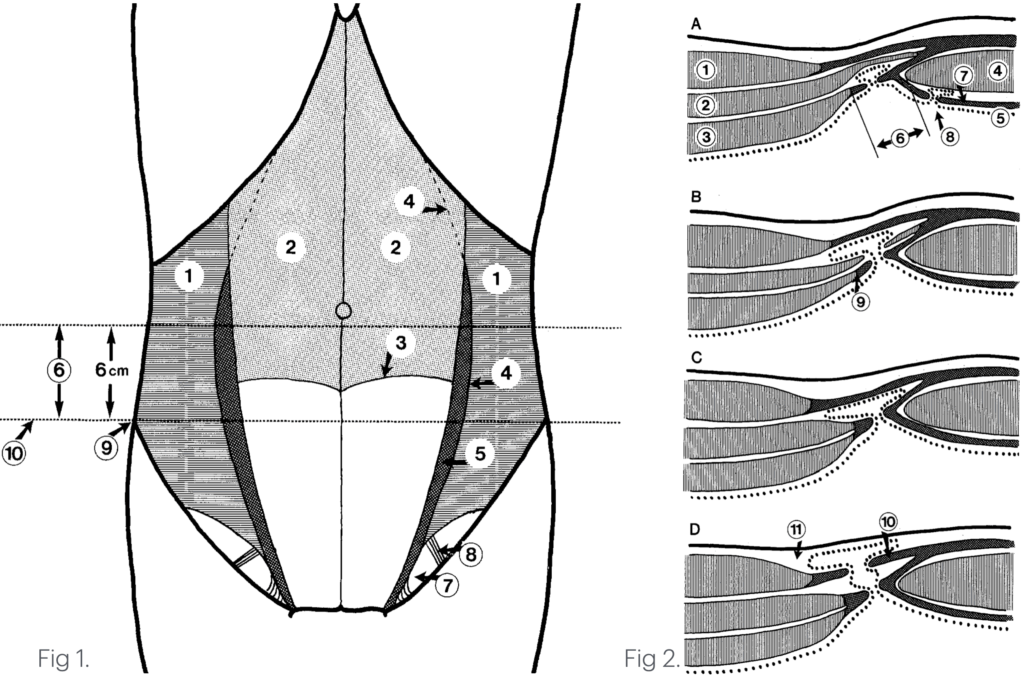
Fig. 1. A ventral view of the abdominal wall showing the topographic anatomy. The external and internal oblique and rectus abdominis muscles are cut away. 1: Transversus abdominis muscle, 2: Dorsal lamella of the rectus sheath, 3: The semicircular line (of Douglas), 4: The semilunar line (Spigelii), 5: Spigelian aponeurosis, 6: Spigelian hernia belt, 7: Hesselbach triangle, 8: Inferior epigastric vessels, 9: Anterior superior iliac spine, 10: Interspinal plane.
Fig. 2. Schematic cross-section of ventral abdominal wall cranial to the semicircular line, indicating the possible location of the hernial sac in spigelian hernias. 1: External oblique muscle, 2: Internal oblique muscle, 3: Transversus abdominis muscle, 4: Rectus abdominis muscle, 5: Peritoneum, 6: Spigelian aponeurosis, 7: Dorsal lamella of the rectus sheath, 8: Intravaginal hernia, 9: Semilunar line (Spigelii), 10: External oblique aponeurosis, 11 : Subcutaneous tissue. Spangen, 1989
- Adriaan van den Spiegel (1578-1625) was a Flemish anatomist and botanist.
- Joseph Thaddaeus Klinkosch (1735-1778), a Flemish anatomist
- Spiegel A. De humani corporis fabrica libri decem. 1627 [Liber III, Caput IV–VI, Spigelian line]
- Klinkosch JT. Programma quo divisionem herniarum, novamque herniae ventralis speciem proponit, nec non anatomicas sectiones, et demonstrationes publicas hyemales anni MDCCLXIV… Pragae. 1764
eponymythology
the myths behind the names
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |
