Ernst Mørch
Ernst Trier Mørch (1908-1996) was a Danish-American anesthesiologist, inventor, geneticist and humanitarian
Mørch was the innovator behind the Mueller-Mørch piston ventilator, one of the first ventilators to deliver positive pressure ventilation and offer an alternative to the then iron lung in polio patients.
To encourage the uptake of mechanical ventilators in clinical practice, Mørch designed a ventilator that was “so simple even a doctor could operate it”. Indeed, the forerunner of his piston respirator was a discarded sewer pipe rigged to a cast off piston and motor! He later designed a laryngoscope and tracheostomy tube for use with his ventilator that bear his name.
Mørch is considered a pioneer of anaesthesiology. He campaigned strongly for anaesthesia to be recognised as its own speciality but encountered much resistance, causing him to leave his native Denmark for America in 1949. His groundwork however was not wasted and an Anaesthesia department did eventuate 2 years after his departure.
Notwithstanding his contributions to anaesthesiology, Mørch was a member of the Danish Resistance during WW2 which is credited for saving 500 Jews from German persecution. He helped to develop a powder from rabbit’s blood and cocaine that anaesthetised the noses of Gestapo dogs and prevented them from finding the Jews hidden under the false bottoms of fishing boats.
Mørch lead a long multi-faceted career and worked as an anaesthetist well into his 80’s, the last decade of which he spent on Amelia Island as both the chief anaesthesiologist and Deputy Sheriff. His ingenuity to find solutions to any problem is a testimony to his favourite motto: “Nothing is impossible”
Biography
- Born on May 14, 1908 in Slagelse, Denmark
- 1913 – Aged 5 he was traumatized by a tonsillectomy without anaesthesia which later prompted him to pursue a medical career with an interest in alleviating painful medical treatment
- 1935 – Doctor of Medicine, University Copenhagen; subsequent residency in psychiatry, radiology, obstetrics-gynaecology and post-mortem pathology
- 1937 – Lieutenant in the Royal Danish Army Medical Corps; initial interest in surgery and is tasked with reattaching ears of horses incidentally severed by officers drawing long swords whilst galloping
- 1938 – Returns to civilian life as an assistant at the University Institute for Human Genetics. Undertakes a thesis on the genetic makeup of chrondodystrophic dwarfs, an interest that stems from a family he knew that conceived only dwarf offspring
- 1941 – Publishes his thesis in which he identifies the gene responsible for dwarfism, a spontaneous point mutation earning the moniker ‘Mørch Unit’; awarded Doctor of Philosophy, University Copenhagen in 1942
- 1942 – Commences work at Copenhagen’s Rigshospitalet and becomes involved in the field of anaesthesia.
- 1943 – Studies anaesthesiology at Stockholm’s Karolinska Institute under famous anaesthesiologist Torsten Gordh (1907-2010); witnesses the use of an early ventilator and later develops his own rudimentary ventilator. He remarked (after watching the primitive ventilator in use by Gordh):
It was very complicated. I decided to build one so simple that even a doctor could understand it…because of the war and the German occupation, I had to make the cylinder and piston from an old, dirty piece of broken sewer pipe. It worked very well
Chicago Tribune 1985
During these years of Nazi occupation in Denmark, Mørch becomes involved with the Danish Resistance. He begins writing and dispersing underground newspapers and conceals Jewish people in hospital by admitting them under German names
Together with a pharmacist friend, Mørch develops a rabbit-blood and cocaine powder which he uses to dull the sense of smell of the Gestapo bloodhounds used to detect Jewish people hidden underneath the wooden floorings of boats
We discovered that if we took rabbit’s blood and dried it, this created a lovely brownish powder that Oluf’ cocker spaniel couldn’t resist…we added cocaine, a 10 percent mixture….then sprinkled on the decks of our fishing boats. The next Gestapo dog that came along loved and sniffed and licked and reported back to his master that he couldn’t smell anything….His nose had a good local anaesthetic
Chicago Tribune 1985
Mørch publishes a book with Kaj Kjerulf-Jensen titled “Saadan kom de Hjem” [How they got home] about his experiences during WW2
- 1946 – Studies anaesthesiology at Oxford University under renowned anaesthetists Sir Robert MacIntosh and William Mushin
- 1947 – Presents a paper to the Royal Society of Medicine in London titled ‘Controlled Respiration by Means of Special Automatic Machines as Used in Sweden and Denmark’. Here he advocates for the use of mechanical ventilation.
- Returns to Copenhagen and attempts to set up a separate anaesthesiology department however is met with great resistance from the surgical department. Despite support from the Danish King, Mørch is ignored and eventually leaves Denmark
- 1948 – Develops a new laryngoscope, but it is not formally introduced to the medical scene until 1951 in America
- 1949 – Mørch moves to the United States and begins practicing as an anaesthesiologist at Doctor’s Hospital in Washington. His departure causes a media frenzy in Denmark drawing attention for the importance of a separate department of anaesthesiology. This is finally achieved in 1951, 2 years after his departure, with support from the World Health Organisation.
- 1950-1953 Attending anaesthesiologist at the University of Kansas Medical centre (KUMC). Develops the Mørch ventilator which is used on colleague Dr Alon P. Winnie who describes the ventilator as:
extremely reliable…the most innovate gadget in the system…was the Mørch tracheostomy tube that used a swivel adaptor to connect the rubber tubing from the valve to the tracheostomy cannula…because of the loose fitting swivel connector of the Mørch tube, movement of either the patient or the rubber tubing is not transmitted to the cannula or the person on the proximal end of the tube…
The air leak resulting from the uncuffed tube allowed me to talk, albeit during inspiration. The ability to communicate while paralyzed and conscious is extremely comforting.
Anesthesia and Analgesia. 2000
- 1953-1959 Director of Anaesthesia at Billings Hospital, University of Chicago and spends the next 6 years modernizing the department. One ‘innovation’ was to encourage the practice of intubation in elective cases (prior to his arrival, intubation was not permitted except in emergencies)
- 1956 – Publishes on ‘Critically crushed chests; a new method of treatment with continuous mechanical hyperventilation to produce alkalotic apnea and internal pneumatic stabilization’. He describes the landmark case of a patient with severe chest injuries treated by Mørch ventilator:
A 51 year old man was slowly rolled, like pie dough, into an 8 inch space between a diesel locomotive and a steel furnace. He was admitted moribund, in deep shock, with multiple bilateral fractures of all ribs, costochondral separations, bilateral hemopneumothoraces….although paradoxical movement (of ribs) was partially corrected, respiratory acidosis continued due to inadequate ventilation….various (…) respirators were tried. These machines did not ventilate the patient adequately…the piston type intermittent positive pressure respirator developed by Morch was then applied.
The patients condition then improved from a semicomatose state of respiratory acidosis to a more comfortable and alert state of alkalotic apnea…lung inflation and deflation were mechanically maintained…with loss of all paradoxical motion…mechanical ventilation was maintained for thirty days….the patient was discharged from hospital fifty-one days after the injury and has returned to his work
Mørch. J Thoracic Surg, 1956
- 1959-1961 Director of Anaesthesia at Cook County Hospital
- 1967-1978 Anaesthesiologist at Presbyterian St Luke Hospital, Chicago until he is forced to retire at the age of 70.
- 1978-1988 Mørch, however, continued working as an anaesthesiologist into his 80s finding a position at Nassau General Hospital on Amelia Island in North Florida. He is appointed the town’s deputy sheriff after he treats a prisoner at the local detention facility because he did not want to disturb the peace should the patient be brought to hospital
- Died on January 13, 1996 from lung cancer in New York
Medical Eponyms
Mueller-Mørch ventilator (1954)
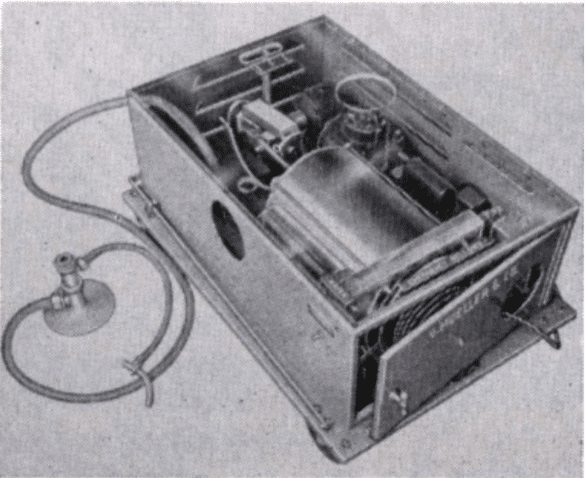
Introduced in 1956 and produced by V.Mueller & co in Chicago, the Mueller-Mørch ventilator was one of the first modern ventilators to provide positive pressure ventilation and an alternate respirator to the iron lung in Polio patients. The prototype design was the combination of a discarded Nazi sewer pipe, a cast off piston and a small electric motor which later evolved to become the Mørch Piston Respirator.
The Mørch ventilator was an intermittent positive pressure ventilator. It was the first of its kind to have concertina-shaped bellows to read tidal volumes and to carry the option for volume controlled or pressure sensitive ventilation. Inspired air could be both humidified and oxygenated. Gas was driven by a piston pump powered by an electric motor and a hand pump incorporated to allow for manual ventilation in case of power failure. Controls were mostly operated by foot and allowed the ventilator to be stowed out of the way under the bed when in use. The stroke volume ranged between 0 to 3600ml with a ‘check-valve’ at the tracheostomy end to ensure exhalation occurred immediately after delivery of the set stroke volume.
It was recommended for use with an uncuffed tracheostomy tube because of ease of insertion compared to a cuffed tube and avoidance of tracheal pressure necrosis (although later case reports would report this as a complication from use of the Mørch respirator). The high volumes of air delivered by the piston compensated for the leakage around the larynx. Mørch later developed his own tracheostomy tube which was marketed by Mueller as an accessory to the Piston Respirator. It incorporated a plastic swivel attachment which minimized transmission of motion to the tracheostomy tube from either patient movement or from movement generated by the administration of air/anaesthesia.
Whilst hailed as a reliable and effective ventilator, there were a number of criticisms that arose with its use. The major disadvantage of the Mørch respirator was that it only allowed for controlled ventilation and was otherwise poorly tolerated in conscious patients.
Then, there was the inadequate humidification system which lead to airway obstruction from dried bronchial secretions. Modifications involved removal of the original humidification chamber and attachment of alternative nebulisers, introduction of a saline solution directly via a drip method into the tracheostomy cannula and heating of the inflow chamber to increase water content of the gas.
There is no nebulization or passage of air through water. The addition of dry oxygen further reduces water content…The excess air flow…tends to dry tracheobronchial secretions. It is obvious from a critical study of this device that the design for humidification is basically inadequate.
J Thoracic Surg 1962
There was the lack of a warning system to indicate airway obstruction. Whilst the Mørch respirator incorporated a ‘check-valve’ to prevent delivery of excessive tidal volumes and pressures, the sound emitted by the functioning respirator caused the valve signal to be inaudible.
Lastly, was tracheal wall erosion caused by the pressure exerted on the mucosa by the uncuffed tracheostomy tube. This was exacerbated by the swivel mechanism of the tube and the vibrations caused from the jet effect of the forced airflow. Use of a larger tracheostomy tube and/or semi-rigid plastic tracheostomy tube mitigated this risk.
A 67-year old white man manifested marked ventilatory insufficiency….The Mørch respirator was attached to the tracheostomy tube. Immediate improvement and relief of symptoms were apparent. On the tenth post-operative day the patient suddenly manifested acute haemorrhage….autopsy revealed that the tracheostomy tube had eroded through the anterior wall of the trachea and into the innominate artery
J Thoracic Surg 1962
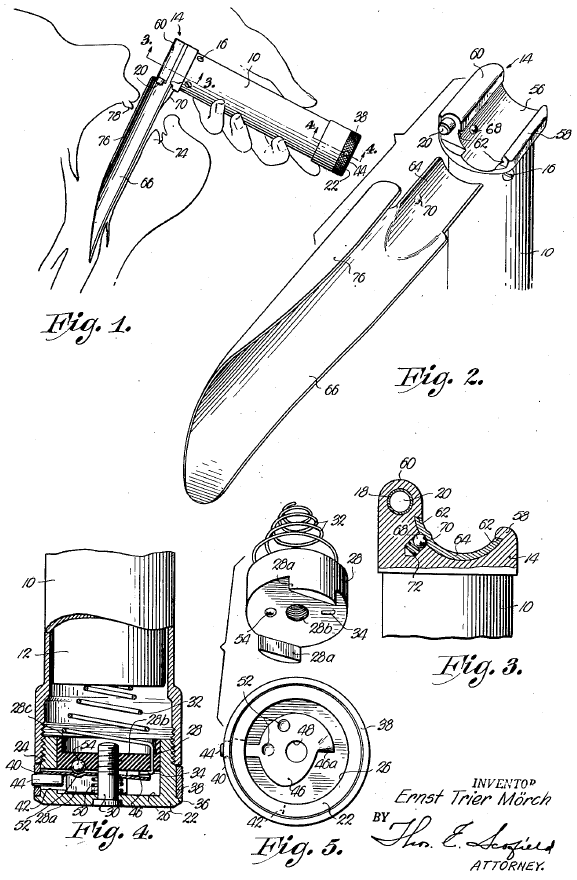
Mørch Laryngoscope (1951)
First appeared in the Foregger Company catalogues between 1952 to 1960; Mørch’s adaptation of the traditional laryngoscope at the time included a battery powered light source incorporated in the handle and a pair of grooves on the handle that allowed the blade to quickly slide in and out.
A feature of the invention resides in providing a handle capable of receiving a variety of interchangeable blades for use in laryngoscopy… (it) lies in the arrangement I provide for detachably mounting the blades on the handle
Another object is to provide a laryngoscope having a novel means for illuminating the interior of the throat and larynx…the blade carries no lamp bulbs or other electrical components…obviates the difficulties which heretofore have attended the sterilization of such blades
Mørch, US patent Office 1951
Major Publications
- Mørch ET. Chondrodystrophic Dwarfs in Denmark-supplemented with investigations from Sweden and Norway-with special reference to the inheritance of chondrodystrophy Thesis (Translated by Hans Andersen, M.D.) 1941
- Mørch ET. Vejledning til Anlæggelse af Forbindinger: For medicinske Studenter. 1943
- Mørch ET. Saadan kom de Hjem: fra tyske koncentrationslejre. København : Munksgaard, 1945
- Helwg-Larsen HF, Morch ET. Genetic aspects of osteochondrodystrophy; Silfverskiöld’s and Morquio’s syndromes. Acta Pathol Microbiol Scand. 1945;22(4):335-57.
- Moerch ET. Controlled Respiration by Means of Special Automatic Machines as Used in Sweden and Denmark [Abstract]. Proc R Soc Med. 1947 Aug;40(10):603-7.
- Mørch ET. Anæsthesi. 1949
- Mørch ET. Laryngoscope US2648329A. United States Patent Office. 1951, SN 251,883
- Mørch ET. A new laryngoscope. Curr Res Anesth Analg. 1951 Nov-Dec;30(6):358-9.
- Morch ET. A new instrument for vaginoscopy and anoscopy. Am Surg. 1952 Feb;18(2):160-1
- Mörch ET, Major RH. “Anaesthesia” (Early Uses of This Word), Curr Res Anesth Analg. 1954; 33(1): 64-68
- Morch ET, Saxton GA Jr, Gish G. Artificial respiration via the uncuffed tracheostomy tube. J Am Med Assoc. 1956 Mar 10;160(10):864-7
- Avery EE, Benson DW, Mørch ET. Critically crushed chests; a new method of treatment with continuous mechanical hyperventilation to produce alkalotic apnea and internal pneumatic stabilization. J Thorac Surg. 1956 Sep;32(3):291-311.
Interesting trivia
Mørch’s creativity and passion for mechanical ventilation also led him to develop a ventilator for a horse – a favourite of the Danish King and a fervent support of Mørch – by fixing a large balloon to a garden hose to effect a seal. The horse was intubated with a pre-made laryngoscope and Mørch then manually ventilated the horse by jumping up and down on its side. The operation was successful and the horse survived
References
Biography
- Thomas Jr RM. Ernst Morch, 87, an Inventor And Leading Anesthesiologist. New York Times, Jan. 18, 1996
- Gorner P. A mind for mankind. Chicago Tribune. 1985
- Rosenberg H, Axelrod JK. Ernst Trier Mørch: inventor, medical pioneer, heroic freedom fighter. Anesth Analg. 2000; 90(1): 218-21.
- Ernst Mörch, MD. History of the Department of Anesthesiology. KUMC
- Morch, Ernst Trier. University of Chicago Library, Special Collections Research Center
- Bibliography. Mørch, Ernst Trier. WorldCat Identities
Eponymous terms
- Hood R, Rush C. Lethal hazards of the Morch respirator. J Thorac Cardiovasc Surg. 1962; 43: 338-42
- Bryant L, Lexington K. A technique for adequate humidification with mechanical respirators. The Journal of Thoracic and Cardiovascular Surgery. 1963; 46(3): 404-407
- Early ICU Ventilators. American Association for Respiratory Care. Virtual Museum
- Morch Laryngoscope. Wood Library-Museum of Anesthesiology
- Morch Surgical Respirator. Wood Library-Museum of Anesthesiology
- Mueller-Morch Piston Respirator. Wood Library-Museum of Anesthesiology
[cite]
Emergency registrar at Sir Charles Gairdner Hospital, Perth