Essential Tremor
Essential tremor is a neurological condition of action motor disturbance resulting in involuntary and rhythmic shaking.
The term “benign essential tremor” was used historically to distinguish essential tremor from Parkinson disease. However, the use of “benign” is discouraged as it trivialises what can be a severe, disabling, and distressing condition.
Essential tremor is the most common cause of action tremor in adults.
It is a slowly progressive condition, most commonly affecting the hands, especially during simple tasks such as drinking from a glass. Less commonly, it may affect the head, voice, and rarely the legs.
Symptoms can range from mild (requiring only reassurance) to severe, causing functional disability and psychological distress.
The exact cause of essential tremor remains unknown.
Primidone and propranolol are the two traditional agents used to suppress essential tremor.
Both are potentially life-threatening in deliberate overdose — this should be considered in patients with severe distress.
Botulinum toxin injections may be trialled if pharmacotherapy is not successful.
If drug therapy fails and symptoms are distressing, surgical options may be considered.
History
- The term “benign essential tremor” was used historically to distinguish essential tremor from Parkinson disease.
- The term “benign” should no longer be used.
Epidemiology
- Essential tremor is the most common cause of action tremor in adults.
- Incidence increases with age, though childhood and early adulthood presentations occur, especially in familial cases.
- ~1 in 5 people over age 65 affected to some degree (Better Health Channel, Victoria).
Pathophysiology
- Exact pathogenesis unknown.
- Likely a syndrome of related disorders, not a single disease.
- Strong genetic component:
- Family history present in 30–70% of cases.
- ~80% in those with onset ≤ 40 years.
- Likely autosomal dominant inheritance with reduced penetrance.
- Multiple suspected risk genes.
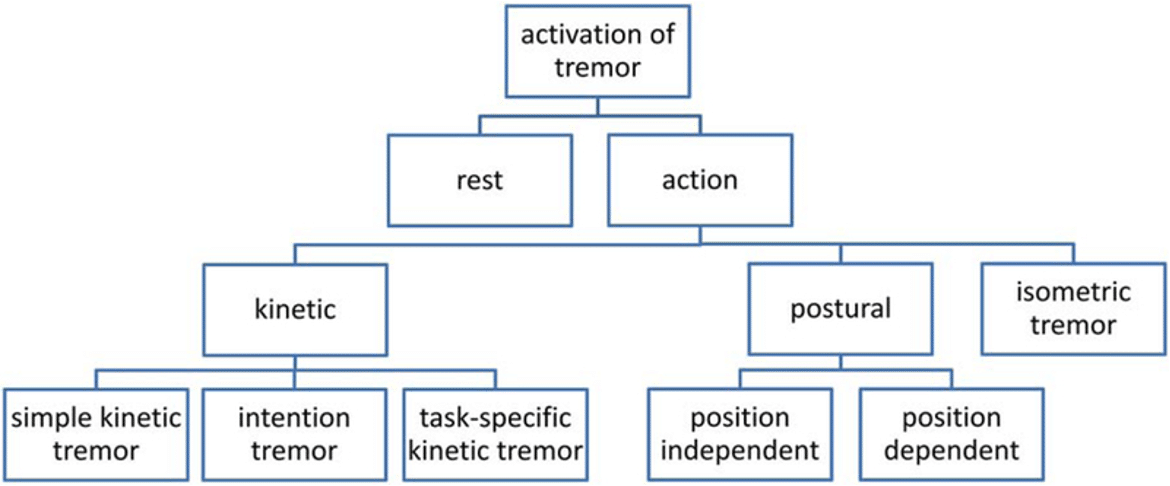
Classification
- Tremors classified as action tremor or rest tremor.
- Essential tremor is an action tremor — includes both kinetic and postural components.
- See Appendix 1 below.
Clinical Features
Distribution
- Hands (most common):
- Worsens during simple tasks.
- Less commonly:
- Head.
- Voice.
- Rarely:
- Legs.
Severity
- Varies:
- Mild → reassurance only.
- Severe → functional disability and psychological distress.
Characteristics
- Frequency: 4–12 Hz.
- Lower end of range in elderly.
Formal Criteria
- Isolated tremor syndrome of bilateral upper limb action tremor.
- Duration ≥ 3 years.
- With or without tremor in other locations.
- Absence of other neurological signs (e.g. dystonia, ataxia, parkinsonism).
“Essential tremor plus” may be used if additional neurological signs of uncertain significance are present.
Aggravating Factors
- Voluntary movement (“kinetic tremor”):
- Amplified during goal-directed movements (e.g. drinking, finger-to-nose).
- Postural maintenance against gravity.
- Anxiety, stress, adrenergic stimulation.
- Not typically worsened by caffeine.
Relieving Factors
- Reduced or absent when body part is relaxed and supported.
- Temporary relief reported with alcohol (not recommended as treatment).
Differential Diagnosis
Parkinson’s Disease
- Rest tremor → typical of Parkinson’s disease.
- Parkinson tremor usually unilateral at onset → helps distinguish from essential tremor.
- Essential tremor may coexist with Parkinson’s.
Normal Physiological Tremor
- Present in healthy people:
- Symmetrical, low-amplitude, high-frequency (8–12 Hz).
- Physiologic tremor can be amplified by adrenergic stimulation.
Related Variants
- Task-specific tremors, isolated tremor, orthostatic tremor:
- Require specialist diagnosis by movement disorder neurologist.
Investigations
General Principle
- Essential tremor is a clinical diagnosis.
- Investigations are used to exclude differential diagnoses.
Blood Tests
- FBE.
- CRP.
- U&Es.
- LFTs (baseline before some treatments).
- TFTs (exclude hyperthyroidism).
Imaging
- CT brain.
- MRI brain/spinal cord.
Electromyography (EMG)
- Document tremor:
- Frequency.
- Burst morphology.
- Differentiate from myoclonus or asterixis.
Management
General Principles
- No cure.
- Treatment aims to suppress tremor to reduce distress and disability.
- Mild cases → reassurance.
- All treatments carry potential adverse effects.
Treatment Modalities
- Pharmacotherapy.
- Botulinum toxin.
- Surgical options.
Factors Influencing Choice
- Tremor severity.
- Degree of functional disability.
- Anatomical location of tremor.
- Medical comorbidities.
- Patient’s subjective distress.
Pharmacotherapy
Propranolol
- Starting dose: 10 mg orally twice daily.
- Titrate up to 160 mg/day in 2–3 divided doses.
Primidone
- Starting dose: 62.5 mg orally at night.
- Titrate up to 250 mg at night if needed.
- Note: Both propranolol and primidone → life-threatening in overdose — caution in patients with psychological distress.
Other Agents
- Atenolol, sotalol.
- Benzodiazepines.
- Gabapentin.
- Topiramate.
Botulinum Toxin
- Trialled if pharmacotherapy unsuccessful.
- Modest benefit, dose-dependent muscle weakness risk.
- Useful for:
- Head tremor.
- Vocal tremor.
- Selected upper extremity tremor.
Surgical Options
Deep Brain Stimulation (DBS)
- Preferred for bilateral moderate-severe limb tremor + midline tremor.
- Electrode implanted in thalamic VIM nucleus.
- Connected to pulse generator implanted in chest wall.
- Improves tremor by 60–90% contralaterally within 1 year.
Thalamotomy
- Creates lesion in VIM nucleus.
- Types:
- Radiofrequency thalamotomy.
- Gamma-knife thalamotomy.
- MRI-guided focused ultrasound:
- High-intensity ultrasound creates lesion.
- Marketed as “non-invasive”, but it is effectively invasive (brain tissue destruction).
- Effective unilaterally.
- Bilateral thalamotomy not recommended → high risk of side effects, esp. speech impairment.
Disposition
- Refer to neurologist with expertise in movement disorders if:
- Symptoms are distressing.
- Diagnosis is unclear.
Appendix 1 — Classification of Tremor
1. Action Tremor
Occurs with voluntary movement.
Subtypes
- Kinetic tremor:
- Simple kinetic tremor: constant during movement.
- Intention tremor: increases as target approached.
- Task-specific kinetic tremor: occurs during specific task (e.g. writing).
- Postural tremor:
- Occurs when maintaining specific posture.
- Isometric tremor:
- Occurs during muscle contraction against stationary object.
2. Rest Tremor
Occurs when body part is at rest and supported against gravity.
Common examples:
- Parkinson’s disease.
- Drug-induced tremor.
References
Publications
- Bhatia KP, Bain P, Bajaj N, Elble RJ, Hallett M, Louis ED, Raethjen J, Stamelou M, Testa CM, Deuschl G; Tremor Task Force of the International Parkinson and Movement Disorder Society. Consensus Statement on the classification of tremors. from the task force on tremor of the International Parkinson and Movement Disorder Society. Mov Disord. 2018 Jan;33(1):75-87.
FOAMed
- Nickson C. Tremor DDx. CCC
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


