FFS: Wernicke Encephalopathy
Wernicke encephalopathy is an acute neurological emergency caused by thiamine (vitamin B1) deficiency.
- Characterised by a classic triad:
- Ocular abnormalities
- Ataxia
- Confusion or altered conscious state
- Most commonly occurs in chronic alcoholics
- Medical emergency: potentially lethal if untreated
- May progress to Korsakoff psychosis, which is often irreversible
History
- Described by Carl Wernicke in 1881 as a triad of confusion, ophthalmoplegia, gait ataxia, with punctate haemorrhages in the brainstem
- Sergei Korsakoff described a chronic amnestic syndrome in alcoholics in 1888–1889
- In teh 1930s Thiamine (vitamin B1) deficiency is experimentally shown to induce Wernicke-like pathology, confirming the metabolic basis of the syndrome.
Pathophysiology
- Caused by deficiency of thiamine, essential in:
- Carbohydrate metabolism
- Pentose-phosphate pathway
- Krebs cycle
Contributing factors:
- Alcohol inhibits GI absorption of thiamine
- Chronic liver disease impairs thiamine activation and storage
Untreated progression:
- Wernicke’s → Korsakoff’s psychosis:
- Retrograde and anterograde amnesia
- Confabulation
Causes
Thiamine deficiency may result from:
- Starvation (rare in Australia)
- Poor nutrition with vomiting:
- Chronic alcohol abuse (most common)
- Hyperemesis gravidarum
- Eating disorders
- Malabsorption syndromes
- Hyperalimentation
- Rare transketolase enzyme defects
Clinical features
Classic triad:
- Ophthalmoplegia
- Ataxia
- Confusion / altered conscious state
Only ~1/3 of patients present with all three features.
Detailed manifestations:
- Ophthalmoplegia:
- Horizontal nystagmus (most common)
- Bilateral lateral rectus palsies
- Conjugate gaze palsies
- Ataxia:
- Acute: vestibular dysfunction (normal hearing)
- Subacute/chronic: cerebellar or mixed dysfunction
- Wide-based, unsteady gait
- Altered mental state:
- Confusion, drowsiness
- Coma (rarely, sole presentation)
Other signs:
- Peripheral neuropathy (esp. lower limbs)
- Autonomic dysfunction:
- Hypothermia, hypotension
- Wet beri beri (heart failure)
Investigations
Diagnosis is clinical, but imaging may support.
Blood tests:
- FBC
- U&Es, glucose
- Magnesium, calcium, phosphate
- LFTs
- Blood alcohol
- Coagulation profile
Other tests:
- CXR: screen for infection
- ECG: as in any unwell patient
- CT brain: rule out structural causes (e.g. haemorrhage)
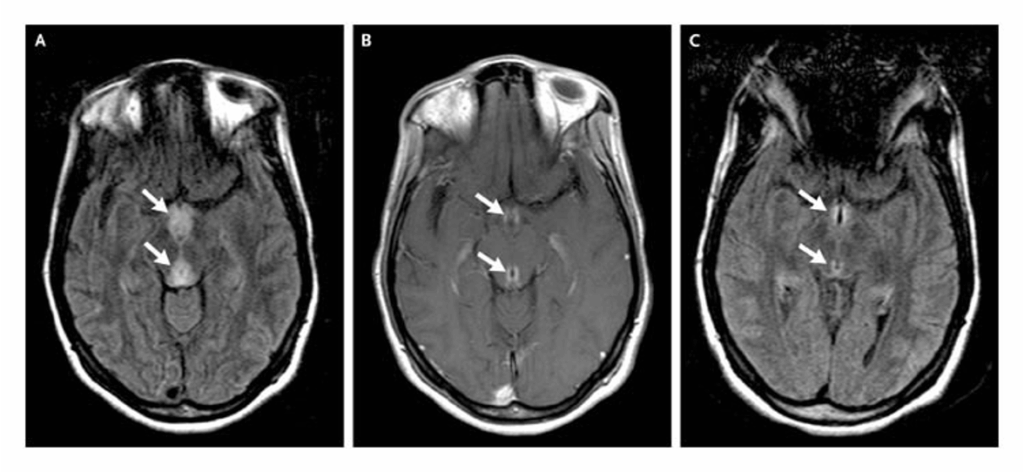
- MRI brain: most sensitive
- Pathognomonic: enhanced mammillary bodies on T1 with gadolinium
- Also peri-aqueductal and periventricular lesions
Management
- IV fluids
- Rehydrate and stabilise
- Sedation (if needed)
- Diazepam / droperidol for agitation or DTs
- Thiamine therapy
- Give before any glucose administration
- Thiamine 500 mg IV over 30 min, TDS for 5–7 days
- Then 100 mg IV/IM daily for 1–2 weeks or until clinical improvement ceases
- Follow with 100 mg daily orally, plus multivitamin
- Correct electrolytes
- Magnesium (required for thiamine function)
- Potassium
- Glucose
- Monitor for alcohol withdrawal syndromes
Disposition
- All suspected cases must be admitted
- Mortality without treatment is ~10%
References
Publications
- Ota Y, Capizzano AA, Moritani T, Naganawa S, Kurokawa R, Srinivasan A. Comprehensive review of Wernicke encephalopathy: pathophysiology, clinical symptoms and imaging findings. Jpn J Radiol. 2020 Sep;38(9):809-820.
FOAMed
- Cadogan M. Wernicke encephalopathy. LITFL
- Cadogan M. Carl Wernicke (1848–1905). LITFL
- Cadogan M. Sergei Sergeivich Korsakoff (1854–1900). LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


