Fingertip Injury
aka Bone and Joint Bamboozler 011
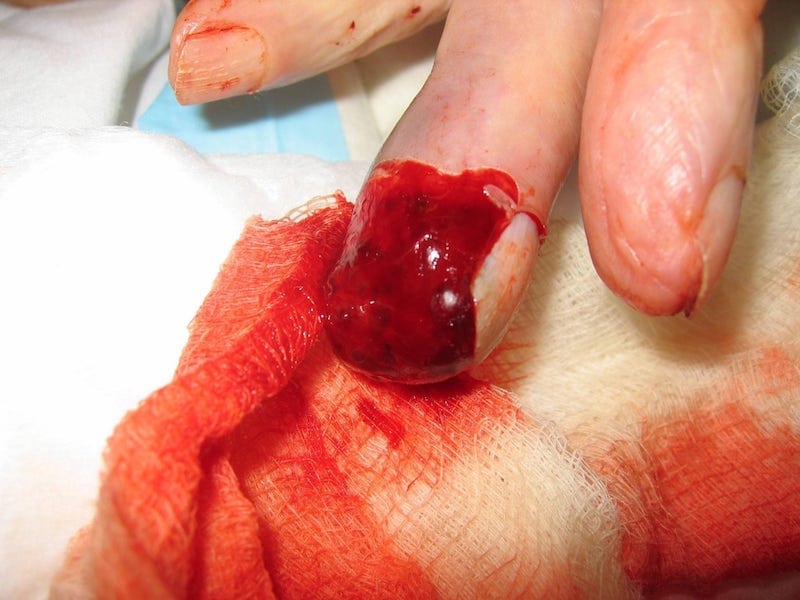
A 56 year old women presents to your minor injuries room, holding a blood soaked tea towel around her middle finger. She reports her blender got jammed, and as she was attempting to fix it…the blender blades whirred into motion…
Fingers sliced, she wrapped her fingers in a tea towel and headed into emergency…
Questions
Q1. What is a fingertip injury?
Answer and interpretation
A fingertip injury is defined as any soft tissue, nail or bony injury distal to the dorsal and volar skin creases at the distal interphalangeal joint and insertions of long flexor and extensor tendons of a finger or thumb
Q2. Describe the anatomy of the fingertip.
Answer and interpretation
The finger tip can be broken up into 3 parts anatomically:
- The Pulp: a dense thick fibrous layer under the epidermis of the entire finger tip. Theses fibrous layers holds the pulp in place to support the distal phalanx.
- The Nail: acts a a protective plate to the nail bed, and provides support to the fingertip during pincer grasp and its sensate function.
- The Distal Phalangeal Bone: provide a firm structure for the pulp and nail to surround.

Q3. How are fingertip injuries classified?
Answer and interpretation
The PNB classification was developed by Evans and Bernardis in 2000, and describes fingertip injures based on injury to the three main components of the finger tip: pulp(P), nail(N), and bone(B). A score is give according to the extent of the damage to each component.
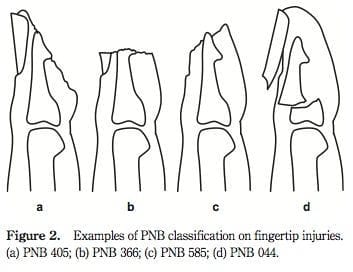
The PNB classification system allows for precise description of the injury which may be of use in the emergency department environment for working out which patients require admission vs discharge, however the system in yet to be validated in this setting.

Q4. Describe the general assessment of fingertip injuries.
Answer and interpretation
History
- What was the mechanism of injury?
- Ischaemic time in fingertip amputations
- Patients hand dominance
- Current occupation and hobbies
- Length of time since injury occurred
- Tetanus immunisation status
- Conditions affecting peripheral circulation, (Smoking, diabetes, Raynauds, atherosclerosis)
Physical Examination
- The size, location and obliquity of the pulp defect
- The type and extent of any nail bed injury
- The presence of exposed bone.
Laboratory Workup
- Laboratory studies are generally not indicated, in simple injuries.
Radiological Imaging
- Radiographs should be taken to assess for fractures, foreign bodies, and of amputated parts to assess the extent of bone loss.
Q5. Describe the general management of fingertip injuries.
Answer and interpretation
Analgesia
- The severity of the injury will determine the if oral or parenteral opioids will be required to manage pain.
- Digital Nerve Block is indicated when any minor surgery or procedure is required on the injured digit.
- The use of a digital nerve block can greatly increase patient compliance to achieve adequate irrigation and wound cleaning.
Haemostasis
- Haemostasis can be difficult, once the wound has been irrigated and cleaned, apply a non adherent dressing, with compression dressing and elevate the wound.
Having difficulty? Try the soaking method from Academic Life in Emergency Medicine
- Poor 10-20mls of 1% lignocaine with adrenaline into a specimen pot
- Have the patient then dip his finger into the pot for 5mins
- The lignocaine with assist with analgesia, and the adrenaline with assist with haemostasis.
Or maybe the Glove Tourniquet is the answer:
Irrigation and Washout
- All fingertip injures that have sustained loss of skin integrity need to be adequately irrigated and cleaned to minimise risk of infection developing, debride devitalised tissues and to ensure wound healing.
Dressings
- Dressing should be applied once the wound has been cleaned and irrigated, or closed.
- The dressing role is to aid in healing, prevent infection, and to provide the patient with comfort and support.
- A non adherent dressing is generally recommend (paraffin-impregnated gauze is my personal preference), and can be secured with either an adhesive tape or a splint.
Splintage
- Splint are generally recommended for most fingertip injures to aid in patient comfort and to support and assist healing fractures.
- Splints can be either made up of plastic or metal.
Tetanus prophylaxis
- Adults who have sustained injuries deemed to be tetanus prone should receive a ADT booster, if more than 5 years have elapsed since their last dose.
Antibiotics
- Infection generally has a low prevalence in fingertip injuries.
- Meticulous wound management early cleaning, irrigation and debridement has shown to be more effective at decreasing infection rates than antibiotics alone.
- Literature is currently conflicting on the use of prophylactic antibiotics in open fractures – however most guidelines currently recommend there use, and local and institutional guidelines should be referred to before prescribing antibiotics.
Q6. What are the common fingertip injuries emergency practitioners need to be aware of?
Answer and interpretation
- Distal Phalangeal Fracture (tuft fracture)
- Avulsion of Digit Pulp
- Nail avulsion and Nail Bed Laceration
- Subungual hematoma
- Digit amputation
Q7. What are the key aspects of the assessment and management of distal phalangeal fractures?
Answer and interpretation
- Fracture generally results from an underlying crushing force.
- 50% of nail bed injuries result in an underlying distal phalanx fracture.
- Provide analgesia, arrange X-ray, antibiotics are generally not recommended.
- Isolated tuft fractures can be managed conservatively with analgesia and application of a splint for 2-3weeks.
- Tuft fractures that are associated with a simple nail bed or pulp laceration, can be managed in the ED. The wound require’s thorough irrigation, the laceration sutured using a figure-of-eight suture with 4-0 or 5-0 nylon, the suturing of the laceration also provides some stability to the fracture and allows healing to occur. The patient can then be discharge home with sutures left in place for 2-3weeks, an external splint should be applied for fracture healing – with follow up arranged with local hand surgeon to ensure adequate healing within a week.
- Patients presenting with significant pulp or nail bed deformity require referral to the hand surgeon for further operative management.
Q8. Describe the assessment and management of digit pulp avulsion
Answer and interpretation
Avulsion of the digital pulp can occur as a result of a shearing force applied to the finger or thumb, or by direct laceration from a sharp edge with complete removal of overlying skin.
- Haemostasis can be difficult to achieve in these injuries due to pulp being a highly vascular area of the digit.
- Provide these patients with analgesia, ensure thorough irrigation then elevate the digit and apply a pressure dressing to help achieve haemostasis, antibiotics may be indicated.
- If this unsuccessful at gaining haemostasis try a compression dressing for 1-2 hours- use caution as prolonged use and excessive tightness can result in necrosis and re-bleeding when dressing removed. Alternatively you could try this Trick of the Trade.
- Once haemostasis is gained, these wounds are generally allowed to heal by secondary intention with meticulous wound care and appropriate dressing application.
- Patients presenting with extensive wounds or wounds that are failing to heal – should be refereed to hand surgeon for possible skin grafting.

Q9. Describe the assessment and management of nail bed lacerations
Answer and interpretation
Nail avulsions result from a shearing force applied to the distal digit, tearing the nail way from the nail bed or nail fold. These injuries often result from crush or shear/tearing forces.
- It is uncommon for a nail avulsion to occur without lacerating the nail bed.
- Its currently recommended to repair the nail bed lacerations to avoid infection, and to limit abnormal or problematic subsequent nail growth. The laceration should be repaired using fine, absorbable sutures.
- The original nail if still intact, should be splinted onto the nail fold to offer some protection to the healing nail bed.
- A soft paraffin gauze dressing should be applied to aid wound healing, give ADT if required and provided antibiotics if wound was dirty or contaminated.
- Patients should be counseled that new nail growth can take a period of months to develop, and may posses some cosmetic defects compared to the original nail.

Q10. Describe the assessment and management of subungual hematomas
Answer and interpretation
- Subungual haematomas occur when there is bleeding beneath the nail.
- Generally caused traumatically by getting it caught between two hard surfaces.
- Provide analgesia and arrange X-ray to rule out a fracture or crush injury.
- Patients not experiencing mild pain, can be managed conservatively with oral analgesia and a splint.
- Patients experience a moderate level of pain should receive trephination – this will give good cosmetic and functional result in both adults and children as long as no other fingertip injury is present- remember to provide an occlusive dressing once trephinated as you have created an open wound. Healing ime generally occurs in 5-7days.
- For more on subungual haematomas see Minor Injuries 001.

Q11. What are the key aspects of the assessment and management of digit amputation?
Answer and interpretation
- Digital amputation generally result by severe trauma and shearing forces to the digit.
- Irrigate the wound thoroughly and apply dressing.
- The amputated digit should be wrapped in sterile gauze that has been moisten with normal saline. Place the digit in a sealed water tight bag, and place the digit on ICE, making sure to note time digit went on ICE.
- Contact hand-surgeon immediately, to review and arrange for urgent re-implantation if digit is still viable.
- Provide analgesia, ADT and antibiotics, and fast the patient ready for theater.

References
- The Half Moon Nail
- Academic Life in EM — Trick of the Trade: Fingertip injuries
- Al-Nammari, S. (2007). Prophylactic antibiotics are not indicated in uncomplicated hand lacerations. BestBets: 1037
- Alwis, W. (2006). Fingertips Injuries. Emergency Medicine Australasia. PMID: 16712532
- Curtis, K. & Ramsden. (2011). Emergency and Trauma Care for nurses and paramedics. Publisher: Mosby: Elsevier.
- Evan, D. & Bernardis, C. (2000). A new classification for fingertip injuries. Journal of Hand Surgery. PMID: 10763726
- Wang, Q. & Johnson, B. (2001). Fingertip Injuries. American Family Physician. PMID 1388710
- Wilkinson, A. (2011). The Role of Prophylactic Antibiotics in Compound Fractures of the Distal Phalanges of the Hand. BestBets: 1297
CLINICAL CASES
Bone and Joint Bamboozler
Emergency nurse with ultra-keen interest in the realms of toxicology, sepsis, eLearning and the management of critical care in the Emergency Department | LinkedIn |
