First Cranial Nerve Lesions
Cranial Nerve I is also known as the Olfactory nerve. Olfactory nerve lesions are uncommon.
If suspected, a mass lesion within the anterior cranial fossa needs to be ruled out.
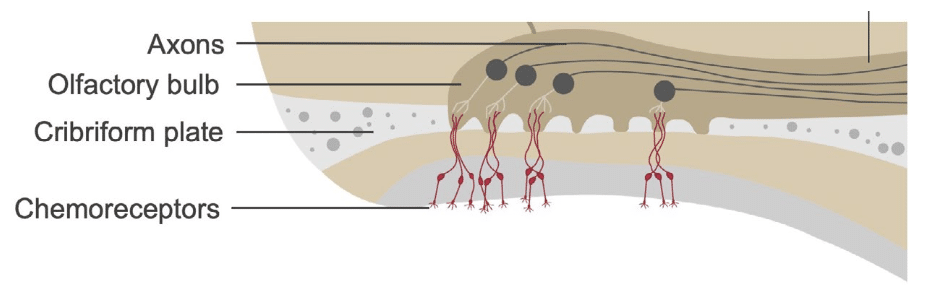
Anatomy
Course of the Olfactory Nerve
The olfactory nerves are paired structures.
Olfactory nerve fibres pass from the mucous membranes of the nasal cavity upward through the cribriform plate of the ethmoid bone, to join the olfactory bulb within the anterior cranial fossa.
The olfactory bulb, lying on the cribriform plate, passes backwards to form the olfactory tract, which runs beneath the frontal lobes to enter the cerebrum via medial and lateral olfactory stria.
Olfactory Nerve Innervations
The olfactory nerves carry sensory fibres to the brain, which convey the sense of smell.
Pathology
| Cause | Comments |
|---|---|
| Trauma | Most common cause. Direct injury to olfactory nerves, often from trauma to the anterior cranial fossa. |
| Space-occupying lesions | Tumours, rarely aneurysms or abscesses affecting the nasal cavity or anterior cranial fossa. |
| Mononeuritis | Various causes, e.g. diabetes, toxins, microvascular disease, paraneoplastic disease, connective tissue disease, infections (HIV, Lyme disease, syphilis). |
| Idiopathic | In some cases, no clear cause is found. |
Differential Diagnoses of Loss of Sense of Smell
| Condition | Comments |
|---|---|
| Seizure activity | May result in altered perception of smell. |
| Upper respiratory tract infections | Common cause of transient anosmia due to inflammation and excess mucus affecting olfactory function. |
Factors That Reduce Sensitivity of Smell
| Factor | Comments |
|---|---|
| Relationship of smell to taste | Flavour perception is largely olfactory; this explains why food tastes bland during a cold. |
| Adaptation | Prolonged exposure to strong odours can reduce perception. |
| Age | Sensitivity declines with age. |
| Smoking | Reduces olfactory function. |
| Some drugs | Certain medications can reduce smell sensitivity in some individuals. |
Clinical Assessment
- Anosmia = complete loss of smell.
- Hyposmia = reduced sensitivity to smell.
Most cases of anosmia are bilateral.
- The First Cranial Nerve is not routinely tested when examining cranial nerves.
- If anosmia is reported, a neurologist may perform formal testing with familiar smells (coffee, vanilla, peppermint).
- Pungent odours (e.g. ammonia) are avoided as they stimulate Trigeminal nerve (CN V) fibres.
If anosmia is suspected, clinicians should look for:
- Signs of intracranial mass lesions.
- Signs of frontal lobe dysfunction.
Investigations
Blood Tests
According to clinical suspicion, consider:
| Test | Purpose |
|---|---|
| FBC | General screen. |
| U&Es / Glucose | Assess metabolic causes. |
| CRP | Inflammation. |
| ESR | Inflammation. |
| Other tests as indicated | e.g. blood lead levels. |
Imaging
| Modality | Purpose |
|---|---|
| CT / CT angiogram | Good initial screening for mass lesions; CT angiogram for suspected aneurysms. |
| MRI | Most sensitive for detecting lesions affecting the olfactory nerve and for visualising the nerve itself. |
Management
Management is directed at the underlying cause, where identified.
Olfactory Neuron Regeneration
The olfactory neurons are unique in that they can regenerate after injury.
- This provides potential for temporary rather than permanent anosmia in some cases.
References
Publications
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Cranial Nerves. LITFL
- Nickson C. Cranial nerve lesions DDx. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


