Frothing Mad
aka Tropical Travel Trouble 002
A 19 year old gap year student has returned from India to your emergency department reporting she was bitten by a monkey at a temple. A selfie gone wrong but it scored 1000+ likes on Facebook…
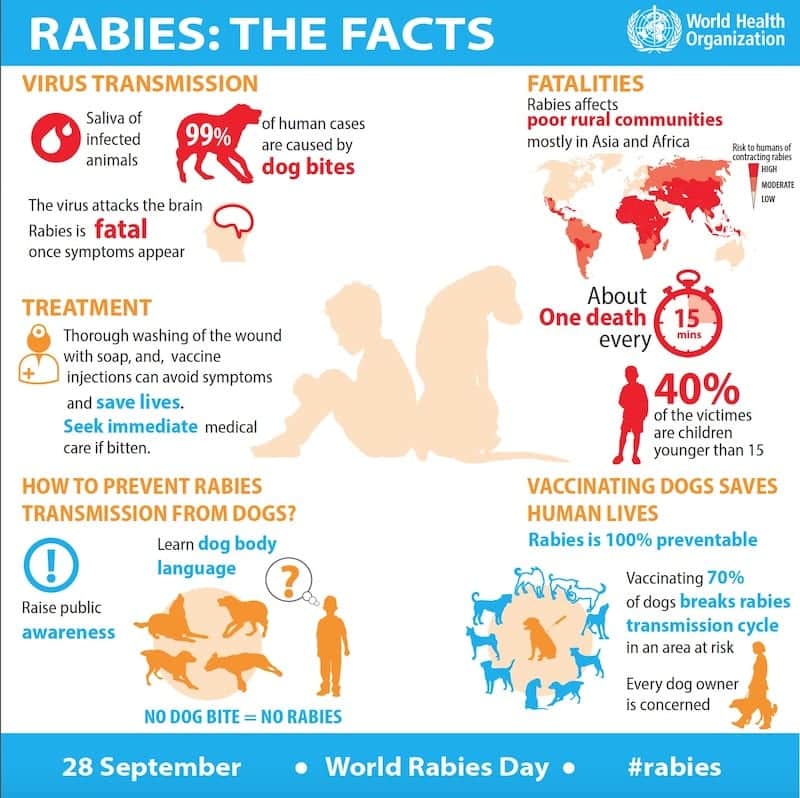
She is concerned because one of the Facebook comments suggested she may have rabies! A quick Google search suggested 60,000 people a year DIE from rabies.
Should she be worried? Should you be worried?
Q1. What other questions should you ask in regards to an animal bite to evaluate her risk of contracting rabies?
Answer and interpretation
- Was there a bite or a lick to a mucous membrane or open wound (therefore a chance of transmission)?
- How proximal to the brain is the bite? Neck bites are higher risk – reduced length of time between exposure and clinical disease.
- Could the animal have the disease, either due to location, type of animal, unvaccinated or clinically unwell? A vaccinated well looking dog in France is very low risk, a stray dog that is frothing at the mouth in India is very high risk
- Can the animal be observed or tested? Usually by 15 days a diseased animal will die, it will most certainly be unwell. This either gives us a clue to potential disease or if the brain tissue is tested for a confirmed diagnosis.
- Has the patient been vaccinated previously? No one has died from rabies who has had the full vaccine course prior and received post-exposure immunisations within 24 hours.
Q2. Which animals transmit rabies?
Answer and interpretation
- Bats
- Dogs
- Cats
- Raccoons
- Foxes
- Skunks
- Wolves
- Jackals
Typically dogs are thought of as the main culprits, accounting for 99% of all human cases. Once they become unwell they typically die within 15 days. Typical symptoms include hydrophobia; hypersalivation; inability to swallow; excessivie excitability/irritability and paralysis. See the excerpt below from ‘To Kill a Mockingbird’:
“I thought mad dogs foamed at the mouth, galloped, leaped and lunged at throats, and I thought they did it in August. Had Tim Johnson behaved thus, I would have been less frightened.”
“Tim Johnson was advancing at a snail’s pace, but he was not playing or sniffing at foliage: he seemed dedicated to one course and motivated by an invisible force that was inching him toward us. We could see him shiver like a horse shedding flies; his jaw opened and shut; he was alist, but he was being pulled gradually toward us.”
“Tim Johnson reached the side street that ran in front of the Radley Place, and what remained of his poor mind made him pause and seem to consider which road he would take. He made a few hesitant steps and stopped in front of the Radley gate; then he tried to turn around, but was having difficulty.”
“In front of the Radley gate, Tim Johnson had made up what was left of his mind. He had finally turned himself around, to pursue his original course up our street. He made two steps forward, then stopped and raised his head. We saw his body go rigid.”
[after Sheriff Tate and Atticus have arrived on the scene] “With movements so swift they seemed simultaneous, Atticus’s hand yanked a balltipped lever as he brought the gun to his shoulder. The rifle cracked. Tim Johnson leaped, flopped over and crumpled on the sidewalk in a brown-and-white heap. He didn’t know what hit him.”
The natural cycle starts with insectivorous bats (up to 8% of some populations are seropositive), this then filters down to wild mammals such as skunks, raccoons, foxes, that get bitten and finally to domestic animals (cats and dogs). The virus on reaching the brain of an infected animal spreads to the peripheral nerves to reach the skin, the lacrimal and salivary glands. Hence these fluids are highly contagious.
There has also been rare cases of transmission through a corneal transplant or other solid organ transplants when the cause of death was not diagnosed as rabies.
Q3. Which countries have rabies?
Answer and interpretation
All of them.

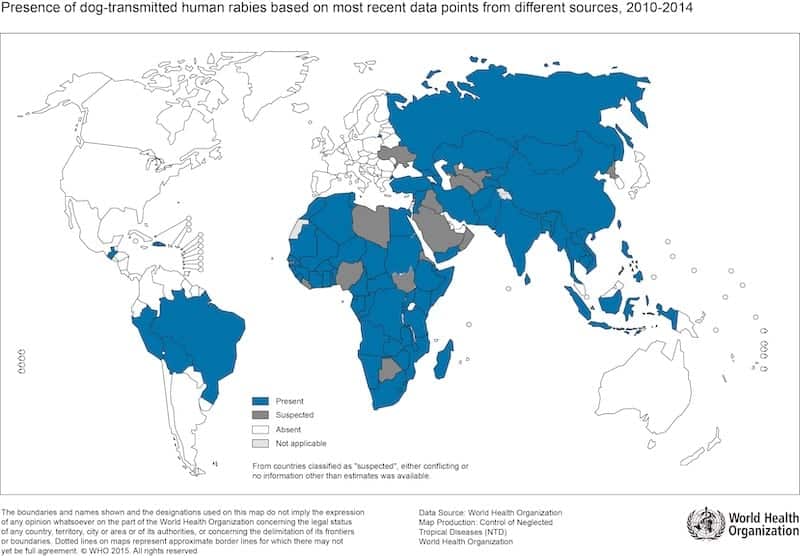
Although, technically the WHO reported the following countries for data on dog related rabies infection (shown below). This excludes the bat transmitted rabies seen in Europe, North America and Australia that can manifest with a similar clinical course and cause fatalities. Not to mention a disease that is likely to be seriously under reported due to diagnostic limitations. So, unfortunately wherever you are in the world there is a potential risk, except maybe Antartica.
Q4. So if we hypothesise that the monkey has rabies, how long before our patient develops clinical signs?
Answer and interpretation
Generally 2 – 8 weeks
More proximal wounds for example, on the neck can take 4 days and there have been reports of people manifesting rabies 19 years after a bite. However, 93% of patients will manifest the disease within 1 year if not treated.
Once inoculated the virus travels centripetally along the peripheral nerves to reach the spinal cord and eventually the brain.
Q5. What are the possible complications of this condition?
Answer and interpretation
Once clinical disease is present, death.
This is a vaccine preventable disease but once clinical signs develop without prior vaccine exposure, death is inevitable.
Q6. Didn’t someone survive Rabies in Wisconsin?
Answer and interpretation

Yes, although the exact reason behind this is not clear.
- Jeanna Giese was bitten by a bat and never had any prior vaccination.
- It is possible she had some prior exposure.
- If we know that not all bats die, it is possible that not all humans die if given a minimal exposure and she therefore already had some rabies antibodies.
- It is also possible that because this was a bat bite instead of a dog her survival was increased.
At the time Jeanna was the first person ever to survive rabies on an experimental protocol called the Milwaukee Protocol:
- High levels of sedation with ketamine
- Amantadine is given because of its use in the original protocol. (There is biochemical evidence of high quinolinic acid in CSF in human rabies, an agonist of the NMDA glutamate receptor. Amantadine in neuroprotective by this mechanism.)
- Ribavirin was originally given but then later changed because of its immunosuppressive effects.
- Vasospasm and clinical exacerbations are regularly encountered on days 6-8 and 13-15 of first hospitalization
- Nimodipine is recommended at half to full dose for prophylaxis against vasospasm.
- Vitamin C (250 mg daily for child and 500 mg for adult, IV or enterally)
- Sapropterin (5 mg/kg/day enterally) and L-arginine (0.5 gm/kg/day IV or enterally) are preferred over nimodipine when available.
Repeated attempts at the Milwaukee protocol have failed and are no longer recommended.
Q7. What are the clinical signs of rabies?
Answer and interpretation
Initially:Pain, paraesthesia or pruritis in the bitten area (30-80% 0f cases). Often reported as intense itching at a previous bite site.
Followed by: Fever, malaise, weakness, headache and neuropsychiatric symptoms.
The disease then either develops into a Furious (brain) rabies or a Paralytic/dumb (spine) rabies. Both result in death:
Furious rabies
- Hydrophobia
- Inspiratory muscle spasm and laryngeal spasm (aerophobia)
- Terrors
- Convulsions
- Involuntary movements
- Autonomic changes
- Hypersalivation and lacrimation
Often patients can be well in-between their spasms and the slightest stimulation can provoke an attack.
Paralytic/dumb rabies
- Flaccid paralysis that ascends either symmetrically or asymmetrically
- Pain
- Fasciculations
- Sensory disturbances
- Paraplegia
- Loss of sphincter control
- Paralysis of the muscles of respiration and swallowing
Q8. How do you diagnose rabies?
Answer and interpretation
Most cases are clinical for a history of dog bite and the above clinical findings.
Immunofluorescence of viral antigen in the base of hair roots from a skin biopsy (typically in the nape of the neck).
Isolation of bodily fluids during the first week of CSF and saliva for culture may work but as the patient develops antibodies the sensitivity is reduced. Although tests are being developed for viral RNA amplification but are not currently available.
Need to repeat testing daily until the diagnosis is confirmed.
Post-mortum from brain biopsy (this should only be performed if absolutely necessary due to the risks of further transmission). Immunofluorescence, tissue culture, PCR and histology can be used. Histology is rarely used but classically the neurones show Negri inclusion bodies.
Q9. How do you manage a suspected case of rabies?
Answer and interpretation
First Aid:
- Wash and flush the wound with soap and water
- Then apply ethanol (700ml/L) tincture or aqueous solution of iodine or 0.1% quaternary ammonium compounds (with no traces of soap in this instance)
- Do not suture the wound as this can increase the risk of inoculation
- Anti-tetanus and antibiotics should be used as per your usual assessment
Clinical signs:
- Supportive care. Rabies is inevitably fatal once any clinical signs are present and patients suffer if not heavily sedated.
- Experimental treatments have been tried in the past and only ever had a handful of successful cases with the bat lyssavirus. We do not know if this is treatment success or vaccine failure.
- The patient’s saliva is infectious and everyone in contact with the patient should use barrier nursing. All staff should receive rabies immunisation (4 intradermal infections of 0.1ml of human diploid cell vaccine, each given into a different limb on the same day)
No clinical signs:
- Vaccinate +/- Rabies Immunoglobulin (RIG)
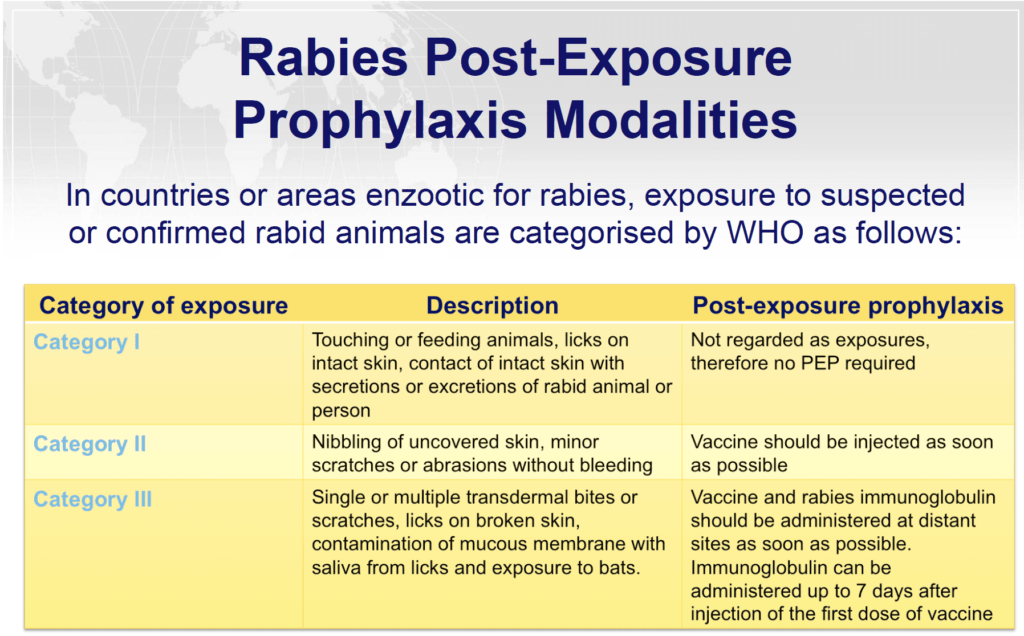

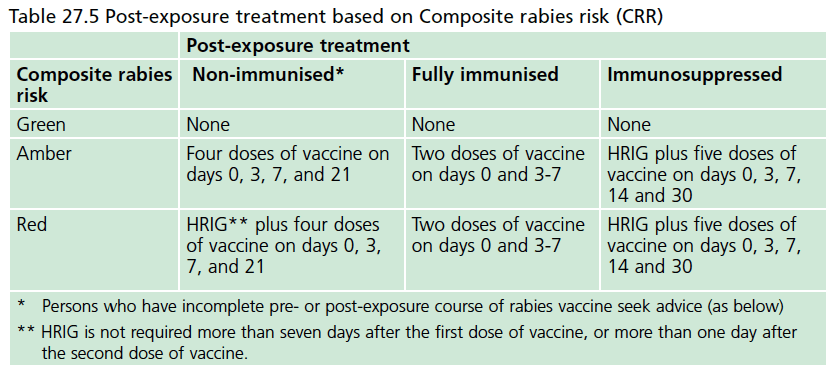
Risk has also been categorised as low in those animals that are healthy and can be observed versus high risk in those that are wild, unwell or can not be observed.
WHO Recommendations for the un-immunised:
2 Intramuscular schedules (usually given in the deltoid or the anterograde-lateral thigh if <2 yrs of age. DO NOT inject into the gluteal region)
- 5 dose regimen (Days 0, 3, 7, 14 and 28)
- The 2-1-1 regimen (Days 0 both arms, 7 and 21)
1 Intradermal schedule (only uses 0.1ml of the 1ml vial, therefore cheaper and can be used in busy clinics or family immunisations to reduce cost). Only proven efficacious with PVRV (Verorab) and PCECV (Rabipur). The vaccine must raise a wheal under the skin or a repeat dose is needed.
- 2-site intradermal, usually in the deltoid area of both arms or supra scapular area. (Days 0, 3, 7 and 28)
Rabies Immunoglobulin (RIG):
- 20 IU/kg for human RIG or 40 IU/kg of Equine RIG (Equine has a higher risk of serum sickness and anaphylaxis)
- The RIG should be infiltrated around the wound, any left over should be given intramuscularly in the anterolateral thigh, remote from the vaccination site.
- If RIG is not available, it should be sourced within 7 days are starting the vaccinations.
WHO Recommendations for the immunised:
- Schedule 1: 1 dose on day 0 and 3 either IM or intradermal
- Schedule 2: A “4 site” intradermal consisting of 4 injections of 0.1ml over the left and right deltoids, thigh or supra scapular area in a single visit.
Q10. I’m travelling to India. What is the pre-exposure prophylaxis regimen recommended by WHO?
Answer and interpretation
Pre-exposure rabies prophylaxis regimens:
- 1-site IM dose on day 0 and 7
- 2 sites ID dose on days 0 and 7 (avoid this route if antimalarials are being used concurrently)
- Routine booster or serology for neutralizing antibody titres is recommended only if continued, high risk of exposure.
- Individuals with documented immunodeficiency should be evaluated on a case-by-case basis, and best receive an ID or IM PrEP schedule as above, plus a third vaccine administration between days 21 to 28
Q11. What public health measures are required to prevent this disease?
Answer and interpretation
Prevention of rabies:
- Those who are travelling to endemic areas, work with wild animals such as vets or people who hug bats. Health care professionals looking after patients with or suspected rabies should be vaccinated. Even those people who like exploring caves should be vaccinated due to reported cases of aerosolised transmission in caves.
- The most successful public health measure is vaccinating dogs. Once herd immunity in the canine population reaches 70% the rabies cycle can be broken. Unvaccinated dogs in some areas are caught and destroyed.
References
- Beeching N and Gill G. Lecture Notes – Tropical Medicine. 7e Wiley Blackwell 2014.
- Eddleston, Davidson, Brent, Wilkinson. Oxford Handbook of Tropical Medicine. Oxford Medical Handbooks. 4e 2014
- Matthews PC. Tropical Medicine Notebook. Oxford University Press, 2017
- The Green Book: Rabies
- World Health Organization (WHO). Human Rabies
CLINICAL CASES
Tropical Travel Trouble
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.

Thanks for the case! Any mammal can get rabies, including cows- an important one for vets and farmers, who are often exposed when they notice symptoms of drooling and attempt to relieve obstruction by reaching an arm in the mouth.
Your answer to the pre-exposure prophylaxis vaccination regimen (IM dose given on day 0, 7, and 21 or 28 or
Intradermal injection 0.1ml on day 0, 7, and 21 or 28) is actually the post-exposure guideline.
Since 2018 WHO recommendation for pre-exposure prophylaxis is:
2 sites ID or a 1-site IM vaccine administration on days 0 and 7
Routine booster or serology for neutralizing antibody titres recommended only if continued, high risk of exposure
Individuals with documented immunodeficiency should be evaluated on a case-by-case basis and best receive an ID or IM PrEP schedule as above, plus a third vaccine administration between days 21 to 28. Additionally, in the event of an exposure, a complete PEP course, including RIG, is recommended
Patients still require post-exposure prophylaxis if have received PrEP but no RIG is required except in immunodeficient patients
Thanks for the updated changes; much appreciated. Neil