Funtabulously Frivolous Friday Five 265
Just when you thought your brain could unwind on a Friday, you realise that it would rather be challenged with some good old fashioned medical trivia FFFF, introducing the Funtabulously Frivolous Friday Five 265
…someone has been reading too much Dr Seuss again. What strange diseases did they catch upon the way
Twas a warm Summer’s night, not long after Friday
Dr Mark Corden
When I walked out of town, down Fantabulous Way
Looking for some animals so I could make friends,
but their zoonotic buddies, spewing out both ends,
made it tricky for me, to try and see,
past their claws, spit, poo and wee.
How it could be, that I was so sick,
Couldn’t win a hand, couldn’t get a trick.
These frisky friends from the animal crew
Made me sick, sick, sick, sick. Far worse than man-flu!
Question 1
From what animal did I catch Psittacosis?
Reveal the funtabulous answer
Birds.
The name Psittacosis derives from the term Psittacine which describes any member of the Psittacidae family of birds which include all true parrots, parakeets and macaws.
Practically, besides poultry (turkeys and ducks), pet birds comprise the usual reservoirs (including parrots, cockatiels, macaws, and parakeets) for Chlamydia psittaci which is an obligate intracellular bacterium that can also be found in non-avian domestic animals, such as cattle, sheep, swine, horses, goats, cats, and wildlife. However, given that birds are the primary reservoir, exposure is greatest in owners of pet birds and workers in poultry-processing centers, pet-shops, aviaries, and veterinary facilities.
Psittacosis is also known as avian chlamydiosis, ornithosis, or parrot fever. Psittacosis is a systemic disease that can cause an atypical pneumonia. C. psittaci can be transmitted to humans by direct contact with the animals, avian nasal discharges, infectious avian fecal material, or inhalation of feather dust. It commonly presents in young to middle-aged males with complaints of chills, headache, myalgia, and dry cough. Symptoms vary from mild to severe systemic disease. In systemic involvement, the patient may present with hepatosplenomegaly and gastrointestinal symptoms.
A tetracycline such as doxycycline 100 mg PO or intravenously (IV) 2 times per day for 7 to 10 days is the treatment of choice. Macrolides are second-line agents. Azithromycin 250 to 500 mg PO once daily is favoured and is the treatment of choice for children.
Reference: Brady MF et al. Pneumonia, Psittacosis. NCBI Bookshelf
Question 2
How did I catch Bartonella henselae?
Reveal the funtabulous answer
A cat scratched me.
Cat Scratch Disease is commonly diagnosed in children but can easily present in adults as well with fever and tender localised lymphadenopathy in up to 90% of cases.
Cats are generally asymptomatic but bacteraemic (up to 50% cats harbour the bacterium in their erythrocytes) and can transmit Bartonella henselae to humans through either scratch or bite. Most cases of cat scratch disease are self limiting (lymphadenopathy lasts 2 to 8 weeks) and do require antibiotic therapy, however Azithromycin has been shown to hasten recovery with a 5 day course.
After contact with an infected cat (or kitten!), it is usual to develop a local primary vesicular lesion. Regional lymphadenopathy, usually but not always ipsilateral develops one to two weeks later. Usual sites of lymphadenopathy include arms/axillae, neck and jaw, groin and more rarely other sites such as peri-auricular, clavicular and chest.
Lymph nodes are swollen, tender and eventually suppurative. Up to three quarters of patients also develop more diffuse symptomatology such as ache, malaise, anorexia and fever. Over 10% of patients will develop myalgias, arthralgias and arthritis.
In immunocompromised patients, B. henselae can cause bacillary angiomatosis and peliosis.
Diagnosis can be made using titres of IgG to B. henselae.W
Reference:
Klotz SA et al. Cat-scratch Disease. Am Fam Physician 2011 Jan 15;83(2):152-155
Okaro U, Addisu A, Casanas B, Anderson B. Bartonella Species, an Emerging Cause of Blood-Culture-Negative Endocarditis. Clinical Microbiology Reviews May 2017, 30 (3) 709-746;
Question 3
What did I walk through to get Leptospirosis?
Reveal the funtabulous answer
Water contaminated with rat urine.
Leptospirosis is a widespread and potentially fatal bacterial (Leptospira interrogans) infection that is endemic in many tropical regions and causes large epidemics after heavy rainfall and flooding. Portals of entry include cuts and abrasions or mucous membranes such as the conjunctival, oral, or genital surfaces.
Infection results from direct or indirect exposure to infected reservoir host animals that carry the pathogen in their renal tubules and shed pathogenic leptospires in their urine. Although many wild and domestic animals can serve as reservoir hosts, the brown rat (Rattus norvegicus) is the most important source of human infections.
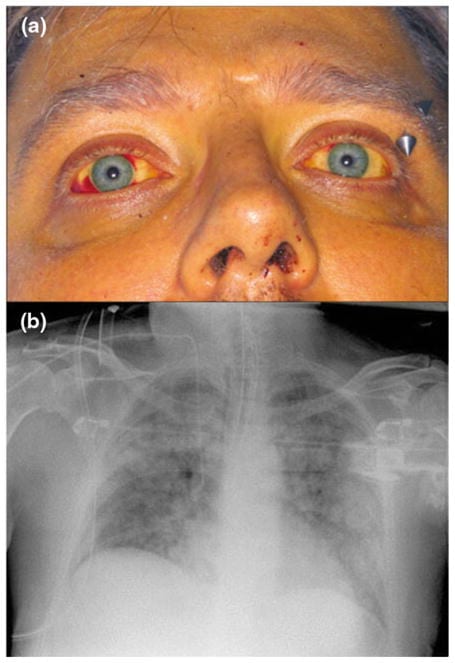
Patients typically present with sudden onset of fever, chills, and headache. The headache is often severe and has been described as a bitemporal, frontal throbbing headache accompanied by retro-orbital pain and photophobia. Muscle pain and tenderness is common and characteristically involves the calves and lower back. A unique sign in identification of leptospirosis is conjunctival suffusion. Additional ocular findings typically include subconjunctival hemorrhages and icterus.
Severe leptospirosis is characterized by dysfunction of multiple organs including the liver, kidneys, lungs, and brain. The combination of jaundice and renal failure, known as Weil’s disease, was first described in 1886 and remains one of the most clinically recognizable forms of leptospirosis.
Therapy for patients with leptospirosis severe enough to merit hospitalization usually involves intravenous penicillin (1.5 million units IV every 6 h), ampicillin (0.5–1 g IV every 6 h), ceftriaxone (1 g IV every 24 h), or cefotaxime (1 g IV every 6 h). Adult outpatients with early disease should receive either doxycycline 100 mg orally twice per day or azithromycin 500 mg orally once per day.
Reference: Haake DA and Levent PN. Leptosporosis in Humans. Curr Top Microbiol Immunol. 2015; 387: 65–97.
Question 4
Where on Earth did I catch Orf?
Reveal the funtabulous answer
From a Sheep.
Orf virus is a DNA virus that belongs to the Parapoxvirus genus which occurs mostly in sheep and goats (and sometimes cattle). Orf mainly infects young lambs and goats who contract the infection from one another or possibly other fomites. In the animal the disease is called contagious pustulardermatitis or scabby mouth due to crusts and scabs formed around the nose, mouth and teats. It is highly contagious, so several animals in a herd may be infected.
Orf is a risk for sheep farmers, shearers, freezing workers, or anyone that bottle-feeds lambs. Children may also acquire it from playing on infected pasture or in a sheep shed. Butchers, meat porters and home cooks are sometimes infected from carcasses, especially sheep heads.
No specific treatment is necessary as most cases have spontaneous resolution in approximately 6 weeks.
Dinc G et al. An Overview of ORF Virus Infection in Humans and Animals. Recent Pat Antiinfect Drug Discov. 2017;12(1):21-30
Winton J. Sheep Pox. LITFL 2018
Question 5
Finally I travelled through central and Southern Africa and didn’t iron my clothes. What fly has now hatched in my body that I can tempt out with bacon?
Reveal the funtabulous answer
The Tumbu Fly
It is caused by the larvae of Cordylobia anthropophaga. The fly lays its eggs on damp clothing (on the washing line) and these hatch with body warmth when the clothes are worn. The larvae develop over 2 weeks and cause a ‘blind boil’ with is ‘prickly’ as the larvae move. A small dark head is seen which is actually the respiratory spiracles of the larva.
Treatment is to partially suffocate the larva with petroleum jelly, once the larvae extrudes itself it can be pulled with forceps. Or… a novel treatment was to place bacon on the larvae to tempt it out. See ‘bringing home the bacon‘ for some gruesome videos.
Prevention is by hot ironing all clean clothes after drying.
…and finally

FFFF
Funtabulously Frivolous Friday Five
Dr Mark Corden BSc, MBBS, FRACP. Paediatric Emergency Physician working in Northern Hospital, Melbourne. Loves medical history and trivia...and assumes everyone around him feels the same...| LinkedIn |