Bringing Home the Bacon
In addition to some good suggestions for the removal of tar, there was at least one important food item missing from Food for Emergencies…. A food, that for anyone who needs it, must surely rank as a truly essential emergency remedy.
Bacon is the food.
What is bacon used for? If you need to ask you’ve probably never suffered from furuncular myiasis.
Furuncular myiasis
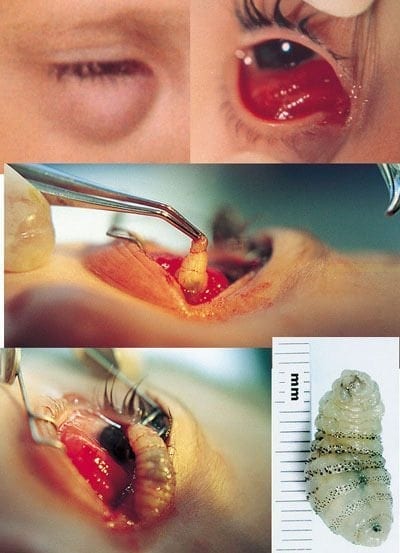
Myiasis is tissue infestation by fly larvae (Order Diptera). There are different types of cutaneous myiasis, including wound-infestation, migratory and furuncular. Furuncular myiasis results from the fly larvae penetrating the skin where they feed in the subcutaneous tissue. The larvae still need to pop up for air now and then, so seeing a wriggling white thing with black “eyes” (respiratory spiracles) poking out of a skin lump is a dead give away. If the diagnosis is in doubt, bedside ultrasonography may help.
There are two important types of fly that cause furuncular myiasis. The human Bot fly (Dermatobia hominis), found in Central and South America, and the Tumbu or Putsi fly (Cordylobia anthropophagia) from Central and Southern Africa (plus at least one case from Portugal!).
The Bot Fly
The Bot fly is particularly devious. The adult female attaches her eggs to day-flying mosquitoes (sometimes other flies or ticks) who unwittingly carry the eggs to potential hosts (a strategy called “hitch hiking” or phoresy). The eggs hatch in response to body warmth and the larvae (or ‘bots’) burrow through the skin painlessly and develop over about 5 to 10 weeks resulting in painful, and sometimes suppurative, boils. Sometimes antibiotics are needed, and tetanus immunization should be updated as required. The prolonged larval stage means that infested travelers may turn up at Emergency Departments anywhere in the world.
I also recommend watching the Animal Planet Video: “Monsters Inside Me – Invasion of the Botfly“
The Tumbu Fly
The Tumbu fly larvae generally comes into contact with human skin after the adult female fly has laid eggs on clothing (e.g. hanging outside). Again the eggs hatch in response to body warmth. The larvae develop under the skin over 8-12 days forming a boil that is painful and prickles with movement. Ironing clothes is a good idea in endemic areas as it kills eggs and larvae.
Bacon Therapy
Many methods for extracting the larvae have been described for the treatment of furuncular myiasis. I think using bacon fat is a good idea. It doesn’t take too long (about three hours), doesn’t leave dead larvae under the skin (as oil occlusion, lignocaine infiltration or larvacide treatment may), it’s non-invasive (avoids the need for incision and drainage) and is cheap. However, it may not be suitable for extreme cases of Tumbu larva infestation as the female fly lays 100-300 eggs in several batches – that would need a lot of bacon.
Procedure: The furuncles are left covered with bacon fat. This encourages the larvae to exit the skin, either due to suffocation or an attraction to bacon. After about 3 hours the bacon fat is carefully removed with forceps at the ready to help fully extricate the larvae.
What you do with the bacon and the larvae afterward is your business. And if you’ve got myiasis, try to look on the bright side, things could always be worse…
References
- Brewer TF, Wilson ME, Gonzalez E, Felsenstein D. Bacon therapy and furuncular myiasis. JAMA. 1993 Nov 3;270(17):2087-8. PMID: 8411575
- McGraw TA, Turiansky GW. Cutaneous myiasis. J Am Acad Dermatol. 2008 Jun;58(6):907-26; quiz 927-9. PMID: 18485982
- Nickson C. Look on the Bright side. LITFL 2018
- Nickson C. The Candirú. LITFL 2018
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC