Funtabulously Frivolous Friday Five 329
Just when you thought your brain could unwind on a Friday, you realise that it would rather be challenged with some good old fashioned medical trivia FFFF, introducing the Funtabulously Frivolous Friday Five 329
Question 1
Where is your pain if you experience Texidor’s twinge?
Reveal the funtabulous answer
Chest
The Texidor twinge, better known is precordial catch syndrome, is a benign and quite common yet underrecognized cause of chest pain in children and adolescents. The syndrome has a remarkably consistent, characteristic presentation and is therefore easily diagnosed.
Texidor’s twinge begins suddenly, without provocation, and is characteristically exacerbated by deep inspiration. It may be worsened or partially relieved by change of position. Episodes last between 30 seconds and 3 minutes, occasionally resolve after a breath or two but may rarely last up to 30 minutes. The pain resolves spontaneously, and typically the child is uncertain of its disappearance until consciously attempting to take a deep breath. Physical examination, both during episode and in subsequent evaluation, are usually normal.
The syndrome was first described and named in 1892 by Henri Huchard (1844 – 1910), a French cardiologist, who called it “précordialgie” (from the latin “praecordia” meaning “before the heart”), or “Syndrôme de Huchard” (“Huchard syndrome”).
En général, à de rares exceptions près, chaque fois qu’un malade vient se plaindre au médecin, d’une douleur dans la région cardiaque, il n’a pas d’affection organique du cœur
Huchard 1893
1955 – The Huchard syndrome was studied in greater depth by Albert J. Miller (1922-2020) and Teodoro A. Texidor (1913-1998), cardiologists at the Cardiovascular Department and the Department of Medicine at the Michael Reese Hospital in Chicago. Miller himself also suffered from the syndrome:
The pain is sudden in onset, is severe, and is localised above the cardiac apex. It has always occurred at rest or during mild activity and invariably has been associated with a “slouched” posture”. The immediate reaction to the pain is a suspension of breathing in mid-respiration or in expiration… breathing is then confined to shallow chest excursions.
Miller, Texidor 1955
Reference:
- Huchard H. Les précordialgies. Revue générale de clinique et de thérapeutique 1893; 7: 1-2
- Chevillot P. Les précordialgies: étude séméiologique sur les douleurs de la région du coeur. 1893
- Millar AJ, Texidor TA. Precordial catch, a neglected syndrome of precordial pain. JAMA 1955; 159(14): 1364-1365.
- Gumbiner CH. Precordial catch syndrome. South Med J. 2003 Jan;96(1):38-41.
Question 2
How many of the inventors of the Wade-Dahl-Till (WDT) cerebral shunt valve were doctors?
Reveal the funtabulous answer
One
- Stanley Charles WADE (1899-1986) was a British toymaker and precision hydraulic engineer who ran a factory that produced hydraulic pumps. He was an acquaintance of Dahl’s sharing a passion for flying model aircraft
- Roald DAHL (1916-1990) the eminent children’s author.
- Kenneth TILL (1920–2008) was an English neurosurgeon.
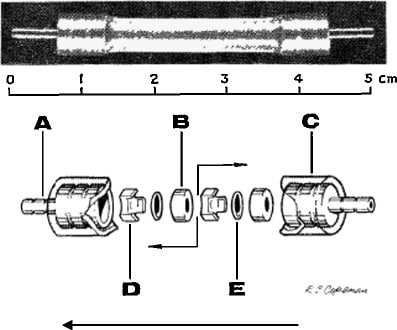
In 1960, Dahl’s 4 month old son was struck by a taxi and suffered traumatic brain injury with multiple skull fractures and cerebral damage. He survived, but developed secondary hydrocephalus. After moving back to the UK, Theo suffered multiple shunt obstructions with debris clogging the silicone slits of his Holter valve.
Dahl became determined to find a solution and contacted Wade. Theo’s treatment was taken over by pediatric neurosurgeon Kenneth Till at the Hospital for Sick Children at Great Ormond Street in London, who invited both Dahl and Wade in his operating room so they could see how the shunts were used in clinical practice. The trio designed a new introducer device for the ventricular catheter and a valve for the treatment of hydrocephalus in young children. The WDT valve was estimated to have been used in two to 3,000 children worldwide from 1962 for two to three years, before it became superseded by more novel valves.

References:
- Buis DR and Mandl ES. Roald Dahl’s contribution to neurosurgery: the Wade-Dahl-Till shunt. Acta Neurochir (Wien). 2011;153(2):429-430
- Sandler AL, Sturrock D, Branfield J, Abbott R, Goodrich JT, Biswas A, Daniels LB 3rd, Flamm ES. Marvelous medicine: the untold story of the Wade-Dahl-Till valve. J Neurosurg Pediatr. 2012 May;9(5):482-90
- Wikipedia – Wade-Dahl-Till valve
Question 3
You have heard of ‘toxic shock syndrome’…but what is ‘toxic squash syndrome’?
Reveal the funtabulous answer
Cucurbitacin poisoning.
Plants in the family of Cucurbitaceae include bottle gourds, cucumber, zucchini, eggplant, squash, pumpkin, and bitter melon. These plants produce cucurbitacin, a pheromone that protects the plants from insects and herbivores, its bitter taste generally prevents poisoning in humans. ‘Toxic Squash Syndrome’ has appeared in the botanical literature but we couldn’t find a similar term in the medical literature.
Out of interest, Cucurbitacins are also currently being explored as an anticancer therapeutic as proposed inhibitors of JAK-STAT3, HER2-integrin, and MAPK signalling pathways.
In one case report of 5 family members eating from the same bottle gourd, within 3 to 25 min of consuming the gourd all five adults developed a sensation of gastric fullness and nausea, followed by sudden onset abdominal cramping, fecal urgency, tenesmus, and diarrhea. The diarrhea was described as watery in three patients and bloody in two. Two patients developed vomiting that progressed to hematemesis within hours.
One day after eating the bottle gourd, all patients continued to experience anorexia and frequent watery diarrhea, more than 30 episodes each. They were each given 2-3L IV 0.9% sodium chloride with improvement of symptoms. The patient who ate the largest quantity was hospitalized for severe dehydration, hypotension, and persistent tachycardia that continued despite fluid resuscitation with 3L of normal saline.
References:
- Ranjan et al. Role of Phytochemicals in Cancer Prevention. Int J Mol Sci. 2019;20(20):4981
Question 4
A 32yo male presents with a painful bite mark to his right thumb and bilateral below knee sweating. What exactly has bitten your patient?
Reveal the funtabulous answer
Redback spider (Latrodectus hasselti).
Bilateral below knee sweating is a unique but pathognomonic feature of redback spider envenomation. Redback envenomation is a clinical diagnosis, and is NOT life-threatening.
The bite itself may not be felt initially, but can cause increasing and increasingly severe pain over minutes to hours; total duration of pain is somewhere between several hours to 5 days – rarely beyond one week. Pain often radiates proximally from the bite site and is associated with abdominal pain, headaches, chest and back pain. Systemic features are notable for nausea, vomiting and lethargy with mild tachycardia and hypertension. Affected children are more likely to exhibit irritability, mild fever and priapism.
The goal of therapy is analgesia. Paracetamol and ibuprofen will be sufficient for most cases, oxycodone will be required for some, stronger or intravenous opioids will be required on occasion.
Antivenom use is increasingly controversial and its benefits over that of analgesia are questionable, whereas its risks (allergy, anaphylaxis, serum sickness) are entirely predictable. It may be associated with possible earlier resolution of pain. Consult your friendly toxicologist when you are considering antivenom to get the latest advice.
Reference:
- Austin toxicology guidelines – Redback
- Hensley J. Has the bell tolled for redback antivenom? EBM Gone Wild
- Nickson C. Does Antivenom Work? CCC
- Long N. Redback Spider toxinology. LITFL
- Nickson C. Bitten by a Redback Spider. LITFL
- Nickson C. Is this a RedBack I see before me? LITFL
Question 5
What organ is affected by Kounis Syndrome?
Reveal the funtabulous answer
The heart (most commonly presenting as a STEMI).
Kounis syndrome, named after a Greek cardiologist Nicholas Kounis who described the phenomenon in 1991 as a histamine-induced coronary artery spasm. Hypersensitivity can be induced by exposure to drugs, food, environmental and other triggers like contrast media or unfortunately coronary stents. The most common manifestation is allergic acute coronary syndrome (referred to as ‘allergic angina’), which is most frequent in middle aged men. Three main variants exist:
- Vasospastic allergic angina.
- Allergic myocardial infarction.
- Stent thrombosis with occluding thrombus that is infiltrated by eosinophils and/or mast cells.
References:
- Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991;45(2):121-8
- Memon S et al. Allergic acute coronary syndrome (Kounis syndrome). Proc (Bayl Univ Med Cent). 2015;28(3):358-362
- Abdelghany M et al. Kounis syndrome: A review article on epidemiology, diagnostic findings, management and complications of allergic acute coronary syndrome. Int J Cardiol. 2017;232:1-4
…and Finally

FFFF
Funtabulously Frivolous Friday Five
Dr Mark Corden BSc, MBBS, FRACP. Paediatric Emergency Physician working in Northern Hospital, Melbourne. Loves medical history and trivia...and assumes everyone around him feels the same...| LinkedIn |
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.