Hip and Pelvis Injuries
aka Trauma Tribulation 028b
It’s time for a look at the latest review from EBMedicine. This post focuses on the following article:
Fiechtl JF, Gibbs MA (2010). An Evidence-Based Approach to Managing Hip and Pelvis Injuries in the Emergency Department. Emergency Medicine Practice, 12(12).
This review cover a lot of territory and is well worth reading for its comprehensive yet lucid overview of traumatic injuries to the pelvis and hip. The review’s selection of clinical and educational images alone makes it worth the effort. The following Q-and-A pearls are only the merest glimpse of what this paper contains in its 24 pages. One of the authors (Jim Fiechl) you may remember from the video on the FARES method of shoulder reduction produced by the guys at Keeping Up in Emergency Medicine.
Questions
Q1. How should you proceed if you suspect a hip fracture but initial radiographs are negative?
Answer and interpretation
Plain films are not sufficiently sensitive to rule out fractures of the hip or pelvis.
If plain films are negative, but a fracture is is still suspected then further imaging is required. Grounds for suspicion may include:
- patient unable to weight bear
- high risk mechanism
- severe osteoporosis
- a feeling in your gut
MRI is the investigation of choice. If unavailable, CT scan may be an option but sensitivity is considerably less than MRI for occult hip fractures.
Q2. When should you perform retrograde cystourethrogram on a patient with a pelvic fracture?
Answer and interpretation
Traditional ATLS teaching is that the retrograde cystourethrogram should be performed to detect urethral rupture prior to attempted IDC insertion if any of the following are present:
- scrotal or vulval hematoma
- high-riding or boggy prostate
- blood at the urethral meatus
However, a recent case series lends weight to the view that a gentle attempt at IDC insertion is acceptable even in the presence of these clinical signs. It should be remember that if performed, an RUG may interfere with subsequent angiographic investigation of pelvic bleeding.
Q3. Define a widened pubic symphysis and what is the significance?
Answer and interpretation
Widening of the pubic symphysis is typical of anteroposterior compression injuries of the pelvic ring.
In the non-pregnant patient the pubic symphysis is normally no greater than 5 mm. When the anterior pelvic ring is widened >2.5cm the posterior portion of the pelvis is routinely injured resulting in a significant increase in the pelvic volume and risk of hemorrhage.
Q4. To what type of fractures can a pelvic binder be applied? How?
Answer and interpretation
A pelvic binder can be applied to any type of pelvic fracture that causes ring disruption.
Any fracture resulting in pelvic ring disruption can result in life-threatening hemorrhage and imaging may not reveal the true extent of the injury as ‘pelvic recoil’ may have occurred after the injury but prior to imaging.
There is no evidence that commercial pelvic binders are better than low tech methods.
The purpose of pelvic binding is to reduce the volume of the pelvis thus tamponading any hemorrhage, as well as provide biomechanical stabilisation. This can be achieved by wrapping a folded sheet around the pelvis. The sheet should center on the greater trochanters and extend to the iliac crests. Taping the thighs or the feet together also helps maintain the anatomical position of the pelvis.
Q5. Should you rock the pelvis to check for stability?
Answer and interpretation
Hell no!
Check stability clinically by gently compressing the pelvis once, making sure that you don’t displace fracture fragments.
We’re meant to treat injury not cause it!
Q6. How can over-reduction of pelvic fractures be avoided?
Answer and interpretation
Over-reduction should be avoided as this may aggravate pelvic injuries.
Pelvic binders should be appropriately tensioned to achieve approximately anatomical alignment. Correct reduction should result in symmetrical positioning of the lower limbs, especially the greater trochanters and the patella.
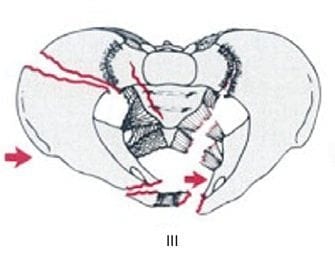
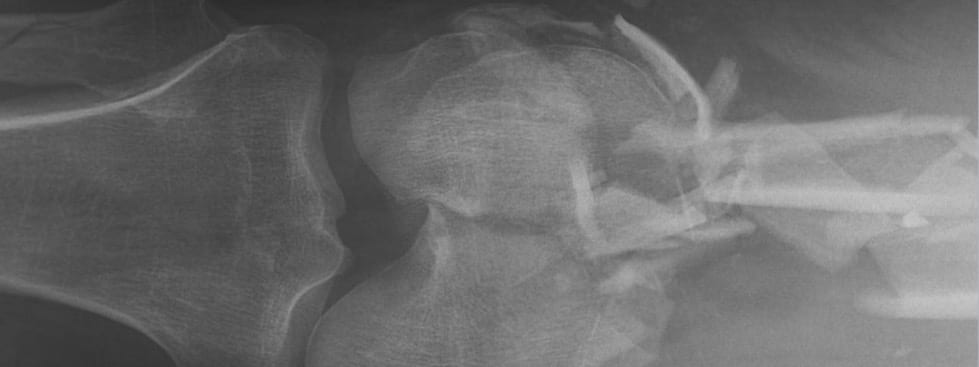
Q7. Using the Young-Burgess classification, what type of pelvic fracture is shown above?
Answer and interpretation
This radiograph shows a ‘wind swept’ pelvis consistent with a lateral compression type 3 injury.
The black arrows show iliac and pubic rami fractures resulting in an internal rotation deformity. The white arrow shows slight contra-lateral hemi-pelvis external rotation. The lateral compression force on the right hemipelvis has transmitted across to the left hemipelvis. Thus the ‘book is closed’ on the right and ‘open’ on the left.
The Young-Burgess classification is based on mechanism. There are 4 broad groupings:
- lateral compression
- anteroposterior compression
- vertical shear
- combined mechanisms
Q8. How useful is the plain radiograph in the investigation of pelvic ring trauma?
Answer and interpretation
The miss rate for pelvic fractures using plain films varies from about 4 to 23% in different studies, and other studies comparing radiographs to CT scans indicates that the sensitivity of pelvic radiographs is only 64-78%.
A CT scan is the imaging modality of choice for assessing pelvic ring injury.
Even when an injury is detected by plain radiography, CT is generally necessary to further delineate the nature of injury and rule out other injuries.
Q9. Which trauma patients do not require pelvic imaging?
Answer and interpretation
Those who are:
- Conscious (e.g. GCS >13)
- no pelvis, back, hip or abdominal complaints
- no tenderness over the lower back, bony pelvis, hip, groin or lower abdomen.
Q10. What should be performed immediately following relocation of a dislocated hip?
Answer and interpretation
Assess stability while the patient is still under procedural sedation.
Perform gentle hip flexion, extension, adduction, abduction, internal and external rotation. Apply downward pressure to the flexed hip to check posterior stability. If the hip re-dislocates, perform relocation and notify the orthopedics team that the hip is unstable. Unstable hips generally require operative intervention.
After this, perform post-reduction radiographs.
Video References
First, up the Allis reduction technique. Personally, I’m not a big fan of standing on the bed…
Here’s a modified Allis technique, what Billy Mallon calls the ‘Captain Morgan Spiced Rum’ method (I’m also a bit concerned about the patient’s knee in this video):
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC