Imaging of COVID-19 pneumonia: a critical care perspective
Author: Dr Greg Brogan – Peer Reviewer: A/Prof Chris Nickson
OVERVIEW
COVID-19 lung imaging is generally indicated in any COVID-19 patient with worsening respiratory status
- commonly manifests as ground glass opacities (CT chest), distributed bilaterally in bases and peripheries
- evolves rapidly and lung involvement is associated with severity; findings progress over 1-3 weeks, typically peaking at 10-14 days
- findings may be present in asymptomatic individuals or pre-symptomatic individuals and may be absent early in the course of disease
In general, the lung imaging findings of COVID-19 patients are consistent with other viral pneumonias – there is no proven specific finding for COVID-19, though there may be suggestive patterns.
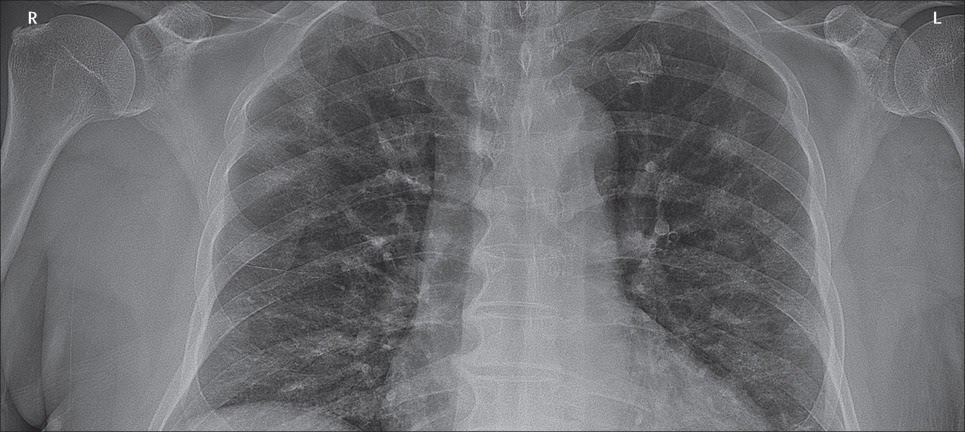
CHEST RADIOGRAPHY
Abnormalities are seen on chest x-ray (CXR) and are more common in severe COVID-19 disease
- CXR has low sensitivity compared to RT PCR – estimates of 59-69% (Guan, WJ et. al. 2020, Wong, HYF, et al. 2020)
- Findings progress with time and appear worse at day 10-12 (Wong, HYF, et al. 2020)
- Findings may even be present before patients test positive on RT PCR (Wong, HYF, et al. 2020)
Features Include (Guan, WJ et. al. 2020 Wong, HYF, et al. 2020)
- Bilateral shadowing (72.9%) – mostly ground glass opacity (68.5%)
- Unilateral disease (25%)
- Local patchy shadowing
- Interstitial abnormalities (less common finding, <5% in some studies)
- Pleural effusions are uncommon
COMPUTED TOMOGRAPHY (CT)
Abnormalities are seen on CT in a majority of COVID-19 cases (86% (Guan, WJ et. al. 2020))
- Involved lung is proportional to severity of disease (Zhao, W et al. 2020)
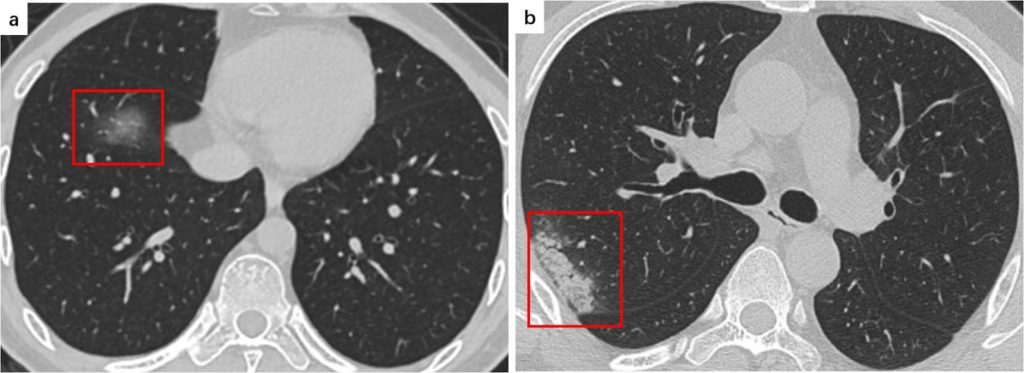
Common CT features (Guan, WJ et. al. 2020 Ye, Z et al 2020 Zhao, W et al. 2020)
- Ground Glass Opacities (GGOs)(Ye, Z et al 2020)
- Hazy areas with increased density and no obscuring of bronchial or vascular markings (see figure 2)
- Most common manifestation – in approximately 88% of cases (Salehi S et al. 2020)
- Most often bilateral (87.5%), peripherally distributed (76%) and multilobar (78.8%) (Salehi S et al. 2020)
- Reticular Pattern (Ye, Z et al 2020)
- Multiple small linear opacities (see figure 2)
- Common, perhaps second most common pattern to GGOs
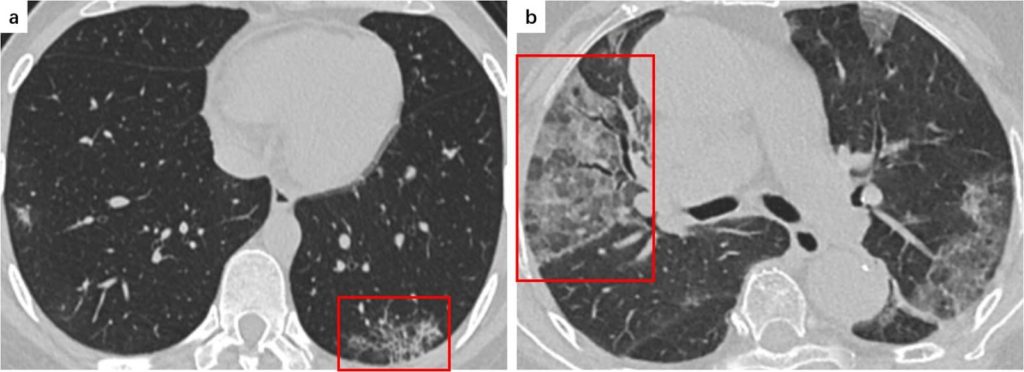
- Consolidation (Ye, Z et al 2020)
- Air spaces replaced with fluid which obscures margins of vessels and airways (see figure 3)
- Sign of progression of disease
- Multifocal, patchy or segmental
- Often subpleural or along bronchovascular bundles
- Crazy Paving Pattern (Ye, Z et al 2020)
- Resembles irregular paving stones from thickened interlobular septa/intralobular lines superimposed onto GGO (see figure 3)
- Seen in 5-36%
Uncommon CT manifestations include (Salehi S et al. 2020, Rodriguez JCL. et al 2020)
- Pleural effusion
- Pericardial effusion
- Lymphadenopathy
- Cavitation
- CT Halo sign
- Pneumothorax
Super-infection may be suggested by pleural effusion, extensive tiny lung nodules, tree-in-bud and lymphadenopathy (Rodriguez JCL. et al 2020)
When followed over time, a pattern to stages of disease emerges (Li, M et al 2020)
- Early Phase – Moderate clinical manifestations with lesions limited to single or multiple areas
- Progressive phase – Lesions progress in extent and density with the accumulation of cellular exudate in alveoli
- Severe Phase – Pulmonary lesions reach a peak at around 14 days with dense bilateral infiltration and a large amount of cellular exudate
- Dissipative Phase – after 14 days, gradual absorption of lesions occurs (may occur earlier if disease course shorter)
Role of CT in diagnosis:
- A single study of 1014 patients in Wuhan suggested high sensitivity (97%), but low specificity (25%) to detect disease the during outbreak (Ai, T et al. 2020)
- A small study of CT-radiologists were able differentiate COVID from non-COVID viral pneumonias (Bai, HX 2020), however they had a wide range of sensitivity (67-93%) and specificity (7-100%)
- Advantage of faster availability than PCR tests, though non-specific and risks of transport remain
- Changes can even be seen in asymptomatic patients (Shi, H et al. 2020)
- However, findings are time dependent (Rodriguez JCL. et al 2020) – Approximately half may have normal study 2 days after symptoms onset.
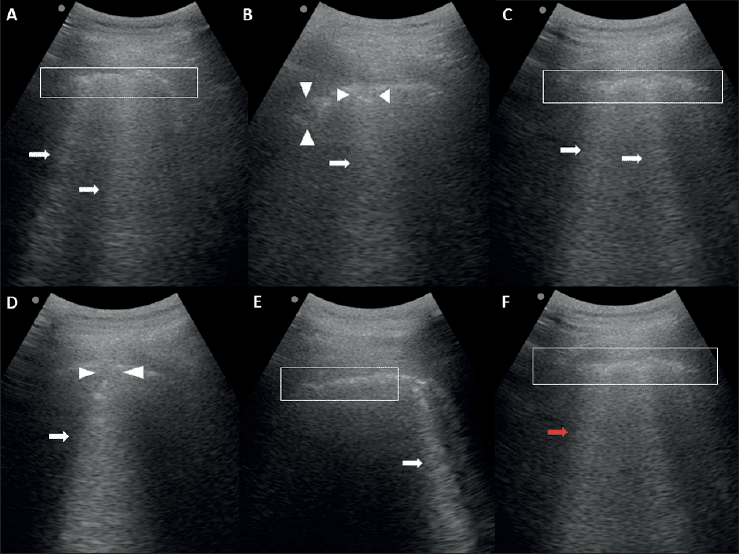
Lung Ultrasonography (US)
The role of lung ultrasonography is still being defined, but no specific COVID-19 findings have been confirmed (Soldati G et al. 2020, Vetrugno, L et al 2020)
- Only sparse case series and case reports currently available
Uses
- May help reduce the amount of CT scans and X-rays required (Vetrugno et al 2020)
- May provide a useful alternative in a climate where transport capabilities, staffing and imaging availabilities are stressed (Smith et al 2020)
Cases exhibit presence of viral pneumonia with features including (Buonsenso, D et al. 2020):
- Irregular pleural line
- B-lines (may be irregular and even confluent)
- Patchy pattern with bilateral sparing
- Areas of white lung
- Subpleural consolidations
Risks
- It is important to consider infection control and prevention of transmission via contact with ultrasound machine
References
LITFL
- LITFL Coronavirus resources
- Coronavirus 2019 (COVID-19) (overview from the Critical Care Compendium)
- Lung Ultrasound in COVID-19
Journal articles
- Ai T, Yang Z, Hou H, et al. Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases [published online ahead of print, 2020 Feb 26]. Radiology. 2020;200642. doi:10.1148/radiol.2020200642
- Bai HX, Hsieh B, Xiong Z, et al. Performance of radiologists in differentiating COVID-19 from viral pneumonia on chest CT [published online ahead of print, 2020 Mar 10]. Radiology. 2020;200823. doi:10.1148/radiol.2020200823
- Buonsenso D, Piano A, Raffaelli F, Bonadia N, de Gaetano Donati K, Franceschi F. Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24(5):2776–2780. doi:10.26355/eurrev_202003_20549
- Guan WJ, Ni ZY, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China [published online ahead of print, 2020 Feb 28]. N Engl J Med. 2020;10.1056/NEJMoa2002032. doi:10.1056/NEJMoa2002032
- Li M, Lei P, Zeng B, et al. Coronavirus Disease (COVID-19): Spectrum of CT Findings and Temporal Progression of the Disease [published online ahead of print, 2020 Mar 20]. Acad Radiol. 2020;S1076-6332(20)30144-6. doi:10.1016/j.acra.2020.03.003
- Rodrigues JCL, Hare SS, Edey A, et al. An update on COVID-19 for the radiologist – A British society of Thoracic Imaging statement. Clin Radiol. 2020;75(5):323–325. doi:10.1016/j.crad.2020.03.003
- Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis [published online ahead of print, 2020 Mar 13]. Travel Med Infect Dis. 2020;101623. doi:10.1016/j.tmaid.2020.101623
- Salehi S, Abedi A, Balakrishnan S, Gholamrezanezhad A. Coronavirus Disease 2019 (COVID-19): A Systematic Review of Imaging Findings in 919 Patients [published online ahead of print, 2020 Mar 14]. AJR Am J Roentgenol. 2020;1–7. doi:10.2214/AJR.20.23034
- Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi:10.1016/S1473-3099(20)30086-4
- Silverstein WK, Stroud L, Cleghorn GE, Leis JA. First imported case of 2019 novel coronavirus in Canada, presenting as mild pneumonia [published correction appears in Lancet. 2020 Feb 29;395(10225):e41]. Lancet. 2020;395(10225):734. doi:10.1016/S0140-6736(20)30370-6
- Smith MJ, Hayward SA, Innes SM, Miller A. Point-of-care lung ultrasound in patients with COVID-19 – a narrative review [published online ahead of print, 2020 Apr 10]. Anaesthesia. 2020;10.1111/anae.15082. doi:10.1111/anae.15082
- Soldati G, Smargiassi A, Inchingolo R, et al. Is there a role for lung ultrasound during the COVID-19 pandemic? [published online ahead of print, 2020 Mar 20]. J Ultrasound Med. 2020;10.1002/jum.15284. doi:10.1002/jum.15284
- Vetrugno L, BoveT, Orso D, et al. Our Italian experience using lung ultrasound for identification, grading and serial follow-up of severity of lung involvement for management of patients with COVID-19 [published online ahead of print, 2020 Apr 1]. Echocardiography. 2020;10.1111/echo.14664. doi:10.1111/echo.14664
- Wong HYF, Lam HYS, Fong AH, et al. Frequency and Distribution of Chest Radiographic Findings in COVID-19 Positive Patients [published online ahead of print, 2019 Mar 27]. Radiology. 2019;201160. doi:10.1148/radiol.2020201160
- Ye Z, Zhang Y, Wang Y, Huang Z, Song B. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review [published online ahead of print, 2020 Mar 19]. Eur Radiol. 2020;10.1007/s00330-020-06801-0. doi:10.1007/s00330-020-06801-0
- Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study [published online ahead of print, 2020 Mar 3]. AJR Am J Roentgenol. 2020;1–6. doi:10.2214/AJR.20.22976
FOAM and web resources
- Radiopaedia – COVID-19
- Intensive and The Alfred ICU – COVID-19 resources
SARS-CoV-2
novel coronavirus of COVID-19
