Johannes Zoon

Johannes Jacobus Zoon (1902-1958) was a Dutch dermatologist best remembered for the first description of chronic benign circumscript balanoposthitis – later eponymously known as Zoon’s balanitis.
Prof. Dr. Zoon was the second professor of dermatology in Utrecht. Zoon’s scientific work focused on skin diseases and less on venereal diseases. He published 97 articles and 7 were dissertations
Zoon succeeded in starting an inpatient department for dermatology at Utrecht. Eager to put an emphasis on underlying pathology, he also set up the hospital’s laboratories for dermatopathology, mycology, physics and chemistry.
Biography
- Born on April 28, 1902 at Wijk en Aalburg, Netherlands
- 1920-1927 Attended Universiteit van Utrecht
- 1927 – Assistant in the Dermatology clinic in the State University Hospital of Utrecht
- 1928 – PhD with a thesis on the compliment binding response in gonococcal infections
- 1929-1945 Chef de Clinique at the Dermatology Clinic
- 1946-1958 Chair of Dermatology at Utrecht University
- 1946-1951 Chair of the NVDV
- 1949 – Presented a series of three patients with chronic, well-circumscribed balanitis at a meeting of the Dutch Society of Dermatologists
- 1952 – Published his findings and described ‘balanitis chronic circumscripta benigna plasmacellularis’ in Dermatologica
- Died on January 28, 1958 at Utrecht, Netherlands
Medical Eponyms
Balanitis von Zoon (1952)
First published in Nederlands Tijdschrift voor Geneeskunde (1950) and later in Dermatologica (1952). Zoon described “balanitis chronica circumscripta plasmacellularis“, a condition he identified in males with chronic balanitis. It is described as a chronic, idiopathic, benign skin lesion that occurs on the glans penis, most commonly in middle- to old-aged men.
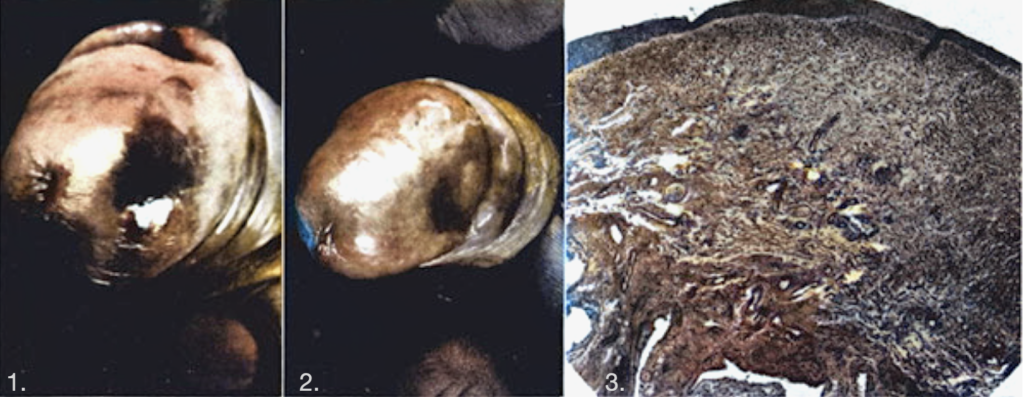
Les photographies des malades 2 et 3 (fîg. 1 et 2) montrent une affection parfaitement semblable à celle présentée dans les traités de dermatologie sous le nom de maladie de Queyrat. Il est frappant de remarquer que l’examen histologique donne chez tous nos malades, non seulement en gros, mais dans le détail, le même résultat.
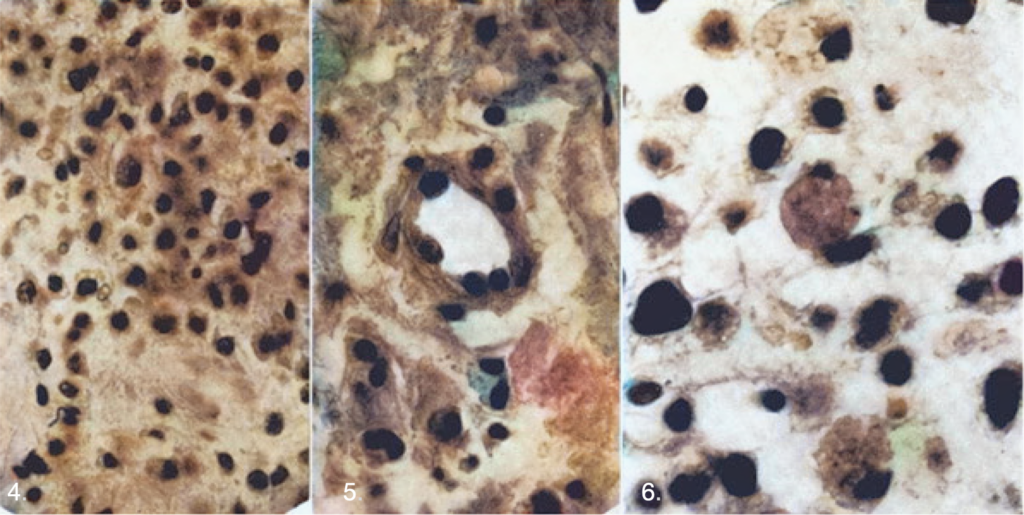
L’épiderme tend à s’atrophier (fig. 3) et est dans beaucoup de cas réduit à quelques couches cellulaires seulement. Dans un seul cas (n° 5) on a trouvé une acantilóse modérée (bénigne). En plusieurs endroits, il y a de l’oedème intra- et extracellulaire (type spongiose). Un certain nombre de cellules montrent une enflure hydropique et un aspect vacuolaire. Elles ressemblent à des cellules dyskératotiques. Les types et les formes cellulaires que l’on rencontre dans la maladie de Bowen ne se trouvent pas dans cette affection. On ne voit pas de mitoses. La couche granuleuse fait défaut dans toutes nos coupes, de même que l’hyperkératose. La limite dermo-épidermique est 6rectiligne, le corps papillaire du derme avec sa structure finement filamentaire manque également.
Dans le derme, on voit une infiltration inflammatoire, située principalement dans le chorion. Cette zone est assez nettement délimitée du tissu conjonctif sous-jacent qui est de structure plus grossière, La délimitation avec le tissu normal latéral est moins nette. Dans quelques-unes de nos coupes, l’infiltration inflammatoire reste séparée de l’épiderme par un fin liseré de tissu conjonctif libre d’inflammation.
The photographs of patients 2 and 3 (fig. 1 and 2) show a condition perfectly similar to that presented in dermatology treatises under the name Queyrat’s disease. It is striking to note that the histological examination gives in all our patients, not only roughly, but in detail, the same result.
The epidermis tends to atrophy (fig. 3) and is in many cases reduced to only a few cellular layers. In only one case (No. 5) was moderate (benign) acantilosis found. In several places, there is intra- and extracellular edema (spongiosis type). A number of cells show dropsical swelling and a vacuolar appearance. They look like dyskeratotic cells. The cell types and shapes found in Bowen disease are not found in this condition. We do not see mitoses. The granular layer is missing in all our sections, as is hyperkeratosis. The dermo-epidermal boundary is 6rectilinear, the papillary body of the dermis with its finely filamentary structure is also missing.
In the dermis, we see an inflammatory infiltration, located mainly in the chorion. This area is quite clearly demarcated from the underlying connective tissue which is coarser in structure. The demarcation with the normal lateral tissue is less clear. In some of our sections, the inflammatory infiltration remains separated from the epidermis by a fine border of connective tissue free of inflammation.
Les cellules inflammatoires sont uniquement ou du moins en grande majorité des plasmocytes (fig. 4). A côté de ces plasmocytes on trouve quelques «Mastzellen» (principalement le long des vaisseaux et des nerfs), peu de lymphocytes et de cellules éosinophiles et quelques fibroblastes. On voit de très nombreux capillaires dilatés et on est frappé par le fait que leur paroi est en général épaissie (fig. 5). Le tissu conjonctif est oedématié. A l’endroit de l’infiltration inflammatoire, le réseau élastique coloré à l’orcéine est peu dense. C’est une conséquence de l’oedème. On ne constate pas de changements dégénératifs. Sur toutes les coupes se trouvent des corpuscules de Russel, qui sont des dérivés des plasmocytes (fig. 6). La réaction au bleu de Berlin est négative.
The inflammatory cells are solely or at least predominantly plasma cells (fig. 4). Alongside these plasma cells we find a few “Mastzellen” (mainly along the vessels and nerves), a few lymphocytes and eosinophil cells and a few fibroblasts. We see many dilated capillaries and we are struck by the fact that their wall is generally thickened (fig. 5). The connective tissue is edematous. At the site of the inflammatory infiltration, the elastic network stained with orcein is not very dense. This is a consequence of edema. No degenerative changes are observed. On all sections there are Russell corpuscles, which are derivatives of plasma cells (fig. 6). The reaction to Berlin blue is negative.
Zoon concluded:
In 8 cases clinically diagnosed as erythroplasia of Queyrat, the author found on histological examination an inflammatory infiltration composed chiefly of plasm a cells with no malignant change in the epithelium instead of the usual precancerous lesion. He names this condition balanoposthitis chronica circumscripta plasmacellularis and differentiates it from Morbus Queyrat which is to be considered cancerous or precancerous.
Major Publications
- Zoon JJ. Balanitis circumscripta chronica met plasmacellen-infiltraat [Chronic circumscribed balanitis with plasma cell infiltration]. Ned Tijdschr Geneeskd. 1950 May 27;94(21):1529-30
- Zoon JJ. Balanoposthite chronique circonscrite bénigne à plasmocytes [Chronic benign circumscript plasmocytic balanoposthitis]. Dermatologica. 1952;105(1):1-7.
- Zoon JJ. Balanitis chronica cirucumscripta benigna plasmacellularis (onderscheiden van erythroplasia Queyrat) [Differential diagnosis between chronic circumscribed benign plasmacellular balanitis and Queyrat’s erythroplasia]. Ned Tijdschr Geneeskd. 1952 Sep 20;96(38):2349-53.
- Zoon JJ, Jansen LH, Hovenkamp A. The nature of colloid milium. Br J Dermatol. 1955 Jun;67(6):212-7.
- Zoon JJ. Tuberculosis of the skin; considerations about pathogenesis. AMA Arch Derm. 1957 Feb;75(2):161-70.
References
Biography
- Goddard JC. Who was Zoon? Urology News 2016; V20(2)
- Doyle C. H18: Professor J.J Zoon (1902–1958) and his contribution to dermatology. British Journal of Dermatology 2022; 181(S1): 192
- Menke H, van Everdingen J, Faber W (eds.) Johannes Jacobus Zoon In: Dutch contributions to dermatology. Overveen, The Netherlands: Belvédère Publishers Limited, 2014: 65.
Eponymous terms
[cite]
Eponym
the person behind the name
MB, BCh, BAO LRCP & SI (Hons). Graduated RCSI Dublin May 2021. Currently working in Western Australia as a junior doctor. Interests include Urology and General Surgery.

