Just another intoxicated head injury
At the start of another busy weekend nightshift in a rural ED you receive a handover from the day team.
A 31 year old female was brought in by police after an assault. Agitated, with a previous history of traumatic brain injury and intravenous drug use, the young lady is restrained and procedural sedation is required to perform the head CT scan.
The sedation was challenging, as a result of Withnail levels of tolerance to benzodiazepines. Following 30mg IV Midazolam and two doses of Droperidol 10mg IM, and 10mg IV, the patient is still fighting and needs further sedation with Ketamine.
Following confirmation of no intracranial bleed on CT brain the patient drifts into a sleeping-beauty style slumber and she is returned to the ED cubicle to sleep off the nights events.
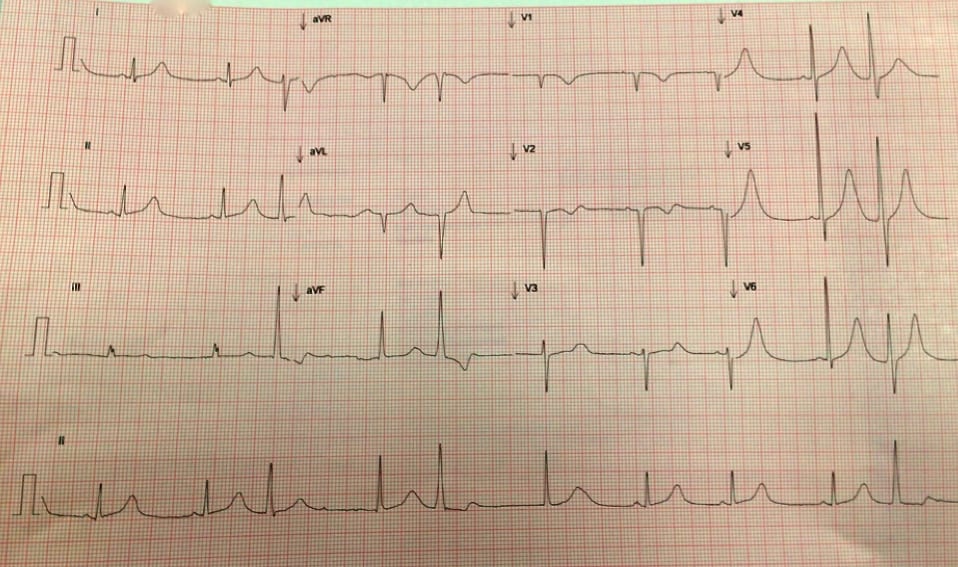
In the early hours of the morning her nurse approaches you stating the young lady has an odd rhythm on her telemetry. She’s still sleeping soundly, bar from the occasional obligatory swear word. An ECG is performed:
Describe the ECG
- Sinus bradycardia
- Three multifocal ventricular ectopic beats
- Large r-wave amplitude in V4-V6 suggesting left ventricular hypertrophy
- Broad and deep t-wave inversion in aVR and V1, biphasic t in V2 and broadly peaked t-waves in the lateral leads.
- QT prolongation 528, QTc 505
You scratch your head and mumble “I wonder whats happened here?”. There are no previous ECGs for comparison and her medical notes are scant and littered with ‘Did not wait’ notifications only.
A review of her medication chart reveals a long list of drug boluses administered during the sedation. You take a seat and start to look through them. Whilst deep in thought the telemetry lead catches your eye…
Describe the ECG trace
- Sinus bradycardia
- Prolonged QT
- “R on T” preceding a short run of polymorphic VT: “torsades de pointes (TdP)“
She is whisked to resus, pads are on and the nurses are looking at you expecting some useful suggestions….
What is the diagnosis?
Prolonged QT interval secondary to droperidol. Possibly this patient has a congenital long QT which has been exacerbated, but this dose has the potential to cause this on its own.
What is the immediate management?
- Check electrolytes
- Load with Magnesium, 10 mmol over 1-2 minutes followed by a slower infusion of a further 20 mmol over the next 6 hours.
- Consider increasing the ventricular rate (to reduce the QT) using isoprenaline or overdrive pacing
- Correct abnormality of any electrolyte and aim for upper limit of normal K+, Mg2+, Ca++
What are the potential causes?
Droperidol induced prolongation of the QT interval resulting in polymorphic ventricular tachycardia – or in this context “torsades de pointes”.
What happened next?
- Magnesium, potassium and calcium were administered.
- Regular ectopics persisted with 2-3 second runs of tdp every minute
- Commenced on an isoprenaline infusion to a rate >90bpm which resolved the ectopic beats and no further torsades.
- Uneventful full recovery.
Take home points
Be aware of the risk of antipsychotics causing QT prolongation, and then VT. Especially when large doses are used in the context of the sedation of an agitated patient.
If the patient is in a chemically induced unconscious state make sure they have adequate monitoring in place.This type of patient may not have old medical notes to look at and wont tell you (or wont know) their medical history, so think of the worst case scenario when you approach cases like this!
ED registrar with lots of interests- the usual- sport, music and wine


is this a case that you encountered personally ?
i assume midazolam was given first ; then droperidol ?
and in a rural ED with paucity of staff ; quick neuroleptisation for safety is a priority…
pretty unfortunate ; i guess… i hope this case does not deter people/junior doctors from using droperidol though.
there are possibly some confounders in why your patient had torsades i.e. (pre-existing use of drugs which may be implicated )
the DORM2 (which demonstrated that droperidol is safe and efficacious for sedation of acutely behaved in ED) study was recently published :
http://www.annemergmed.com/article/S0196-0644%2815%2900222-X/abstract
this study’s conclusion was : “.. supports the use of high-dose droperidol as a safe sedating agent for patients with acute behavioral disturbance in the ED. There is no evidence of increased risk for QT prolongation with the doses used in this study.”
yes, there are some limitations i.e the authors admit that : “Despite the large number of ECGs, the study
was still unable to rule out rare adverse events (<0.1%): torsades de pointes. The rarity of torsades de pointes means
that much larger studies are required to show that there is no or minimal association between droperidol and torsades
de pointes."
agree with your statement where these patients need monitoring !
what about propofol? Sedation dose boluses then a continuousc infusion i.e. TIVA?
Hi John and Ayman! I had seen the study that you mention- makes this a topical issue! It’s not my aim to discourage the use of droperidol, rather to highlight the importance of monitoring patients closely after they are given any sedation. I was involved in this case and she had been given multiple doses of midazolam, droperidol and finally ketamine to achieve sedation to get her through a CT scan.
You make lots of good points- there are other possible causes of her TdP, she may have an underlying QT abnormality or have taken other drugs. Even if she did, it is reasonable to suspect that droperidol was a factor. The take home point is without being aware of the possibility of TdP you might not pick it up, as rare as it has been shown to be!
As for propofol.. there are lots of ways to skin a cat! For what its worth I think ketamine was a good third line agent. It would be interesting to hear the FOAM community’s opinion? Her airway was not for the faint-hearted!
While I know the ED community seems to have embraced droperidol, it is worth talking to anyone who ever had droperidol in the old days of ‘neuroleptanalgesia’ and experienced the absolute terror described as “inner turmoil, outer calm”. One of my teachers used to use a lot of droperidol until he personally experienced it as part of an anaesthetic then never ever gave it to a patient again, having experienced its effects. Low dose droperidol (0.5mg or 0.01 mg/kg) is an excellent antiemetic. High dose droperidol is a DREADFUL sedative, when there are so many better agents available. I agree it does not warrant the ‘drop-dead-erol’ epithet, but studies such as the ones quoted for its “safety” only look at cardiovascular effects and do not evaluate the neurocognitive consequences of a very poor choice of sedative.
A few counter points.
Your teacher used it a lot. This would make me think that it had safety and usage characteristics that made it more favourable than the other options. Then he had a bad experience with ONE anaesthetic – which presumably included a number of other agents – and changed his practice because of it. This is absolutely an understandable human response to the situation, but is counter-intuitive to use it to guide practice. Presumably he had also not had enough complaints from those who he had administered it to. Anecdotes alone should not guide practice.
The highest use for droperidol in most EDs I have encountered is for the acutely behaviourally challenged patient. This is a unique group for several reasons: often young, frequently on a cocktail of medications including various typical and atypical antipsychotics, often with recreational drug use / abuse and relative tolerance to benzodiazepines and / or narcotics, and frequently intoxicated with alcohol or recreational drugs at the time of presentation. These patients generally need to be rapidly de-escalated for everyone’s safety and generally need to be assessed for physical injury, adverse drug effects, and often neuroimaging. In this context and often at considerable risk to staff with any delay, any drug that can be given IM, rapidly titrated, with less effects on respiratory drive and a predictable course including usually waking up more civil should be strongly considered. Benzos are often unhelpful due to tolerance and respiratory depression, propofol results in the same safety / behavioural problem being encountered after the infusion is stopped with a few severe allergies, olanzapine usually takes a bit longer to work, ketamine may tansiently exacerbate the problem and in combination with recreational cardiovascular stimulants may be dangerous…
Is inner turmoil a problem in the patient with inner and outer turmoil already?
I still prefer haloperidol, but mostly because of familiarity. The two seem near equivalent in practice.
This is a very different scenario from general anaesthesia in the peri-procedural environment with a lucid, co-operative patient.
What are the ‘so many better agents’?
I’m a propofol believer. The speed of scanners these days make a single titrated bolus last beyond the scan duration, and tolerance is not an issue. DOI: Anaesthetist who would have RSI on standby just in case.