Kounis Syndrome
Acute coronary syndrome in the setting of allergic or anaphylactic reactions, usually secondary to allergic coronary vasospasm
Hypersensitivity coronary disorder originally described in 1991 by Kounis as “acute coronary syndrome associated with allergic reaction”.
- Also known as “allergic angina”, “allergic myocardial infarction”, or “coronary hypersensitivity disorder”, the vasospastic changes seen in Kounis syndrome do not always lead to infarction
- Induced by various conditions, drugs, environmental exposures, foods and coronary stents. The most common recognised triggers are antibiotics (28%) and insect bites (23%).
Pathophysiology of Kounis Syndrome
- The exact underlying mechanism is not fully understood, and there are two proposed mechanisms. Allergic, hypersensitivity, anaphylactic and anaphylactoid reactions are associated with Kounis syndrome.
- Ischaemia is thought to be due to release of inflammatory cytokines and inappropriate platelet activation through mast cell activation, which leads to coronary artery vasospasm and/or atheromatous plaque erosion or rupture.
- Apart from coronary arteries, it affects the cerebral and mesenteric arteries.
- Other proposed mechanisms are that global myocardial hypoperfusion occurs as a result of systemic vasodilatation and decreased venous return in the context of anaphylaxis
Kounis syndrome is a ubiquitous disease which represents a magnificent natural paradigm and nature’s own experiment in a final trigger pathway implicated in cases of coronary artery spasm and plaque rupture. Kounis syndrome seems to be not a rare disease but an infrequently diagnosed clinical entity which has revealed that the same mediators released from the same inflammatory cells are also present and in acute coronary events of non allergic etiology. These cells are not only present in the culprit region before plaque erosion or rupture but they release their contents just before an actual coronary event.
Kounis 2016
Types of Kounis Syndrome
Vasospastic allergic angina, allergic myocardial infarction and stent thrombosis with occluding thrombus infiltrated by eosinophils and/or mast cells constitute are the three reported variants of this syndrome.
| Type | Cardiac history | Pathological changes |
| I | Normal coronary arteries No risk factors for IHD | Coronary artery vasospasm |
| II | Inactive preexisting atheromatous disease | Plaque erosion of rupture causes vasospasm or infarction |
| III | Previous coronary artery stenting | Stent thrombosis secondary to platelet activation |
Clinical significance
- Diagnosis and treatment requires attention to both cardiac and anaphylactic pathophysiology
- Morphine must be avoided in Kounis Syndrome as it may stimulate histamine release and exacerbate mast-cell induced vasospasm
- Some authors advocate that adrenaline should be used with caution as it may aggravate coronary ischaemia by worsening vasospasm
- ECG changes often resolve upon treatment and withdrawal of underlying allergic insult
- Patients who undergo angiography will have improvement of vasospastic changes with administration of intracoronary nitroglycerine
Addressing Kounis Syndrome (KS) as a separate entity in the ACS guidelines is imperative, as the conventional management of patients with ACS might not necessary apply to all patients with KS. In general, the prognosis of KS is better than the “conventional” acute coronary syndrome. This can be explained by several reasons including the known history of allergy to the trigger, the presence of other allergic manifestations and the early administration of the medical therapy which is effective in most of the cases.
Abdelghany 2017
History of Kounis Syndrome
1950 – Pfister and Plice published the first report of acute myocardial infarction during a prolonged allergic reaction to penicillin
1991 – Kounis and Zavras published the first complete description of the pathophysiology, aetiology and clinical symptomatology of histamine-induced coronary artery spasm and the ‘syndrome of allergic angina’.
1998 – Braunwald categorized allergic angina in a subgroup of dynamic coronary occlusion lesions by stating that “allergic reactions with mediators such as histamine or leukotrienes acting on coronary vascular smooth muscle” can induce vasospastic angina
2008 – Biteker et al published the first of four cases of children presenting with Kounis syndrome. They recount the case of a 9-year-old previously healthy girl stung about the head and neck several times by honeybees. She presented with an erythematous rash over the face, neck, and arms and complained of chest pain radiating to neck.
ECG showed ST segment elevation in II, III, aVF, and V5–V6 leads compatible with acute inferior myocardial infarction. Echo revealed inferior wall hypokinesia and ejection fraction of 50%. Labs revealed elevated troponin I of 4.3 ng/ml; CK-MB of 342 U/l; serum tryptase of 45 μg/l, and IgE of 190 IU/ml. Coronary angiography revealed normal coronary arteries. The patient was treated with oral antihistamines and prednisolone. Five days after admission, cardiac markers and serum tryptase levels were within normal limits with resolution of electrocardiographic abnormalities and regression of inferior wall motion abnormality on echocardiography.
Biteker 2009
They concluded:
The diagnosis of this unique disease should be entertained when acute onset chest pain is accompanied by allergic symptoms, electrocardiographic changes, and elevated cardiac enzymes. All patients admitted to the emergency departments with chest pain and ST elevation on electrocardiography should be interrogated for allergic insults.
Biteker 2009
2012 – Kounis syndrome associated with hypersensitivity responses and coronary stent implantation
Case examples
Example 1 (Memon et al)
75-year-old man with known diabetes mellitus, hypertension, and hyperlipidemia presents to ER with dysuria and fever. Intravenous ceftriaxone was administered for suspected urosepsis. Post injection he immediately developed a generalized erythematous macular rash, hypotension, and tachycardia followed by pulseless electrical activity and cardiac arrest.
IV adrenaline was administered as per ALS protocol and the ECG below taken post-ROSC
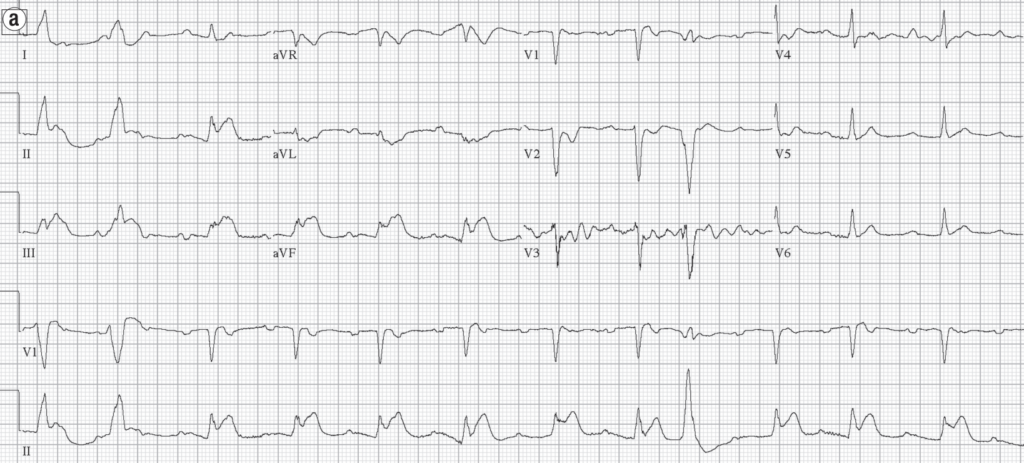
Source: Allergic acute coronary syndrome (Kounis Syndrome)
Th e patient also received intravenous diphenhydramine, famotidine, and methylprednisolone. Subsequent electrocardiograms taken 5 and 15 minutes later showed normalization of ST segments
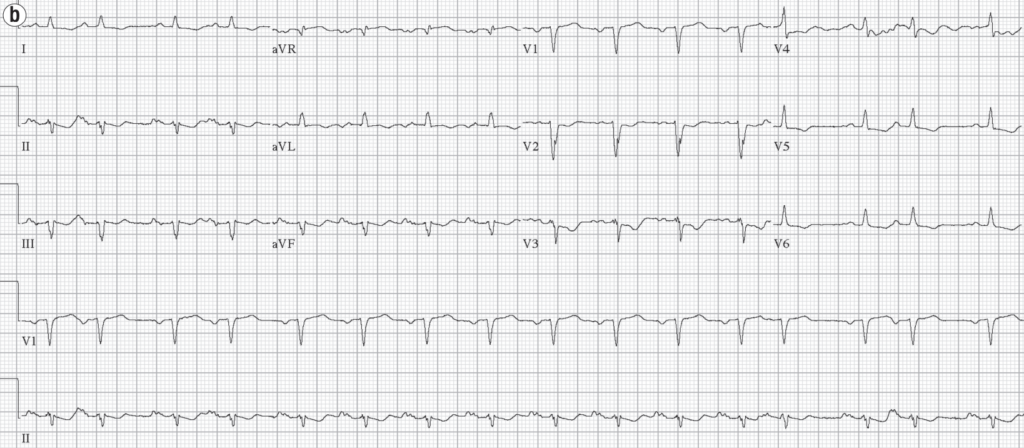
Source: Allergic acute coronary syndrome (Kounis Syndrome)
He suffered no troponin rise and was discharged home in a stable condition, with elective nuclear stress test showing no evidence of ischaemia
References
Original articles
- Pfister CW, Plice SG. Acute myocardial infarction during a prolonged allergic reaction to penicillin. Am Heart J. 1950 Dec;40(6):945-7.
- Kounis NG, Zavras GM, Soufras GD, Kitrou MP. Hypersensitivity myocarditis. Ann Allergy. 1989 Feb;62(2):71-4
- Kounis NG, Zavras GM. Histamine-induced coronary artery spasm: the concept of allergic angina. Br J Clin Pract. 1991; 45(2): 121-128 [First complete description of the pathophysiology, etiology and clinical symptomatology of ‘allergic angina’ syndrome.]
- Nikolaidis LA, Kounis NG, Gradman AH. Allergic angina and allergic myocardial infarction: a new twist on an old syndrome. Can J Cardiol. 2002 May;18(5):508-11 [First description of the first two type variants of Kounis syndrome]
- Kounis NG. Kounis syndrome (allergic angina and allergic myocardial infarction): a natural paradigm? Int J Cardiol. 2006 Jun 7;110(1):7-14 [Complete description of Kounis syndrome]
- Kounis NG, Mazarakis A, Tsigkas G, Giannopoulos S, Goudevenos J. Kounis syndrome: a new twist on an old disease. Future Cardiol. 2011 Nov;7(6):805-24
- Kounis NG, Giannopoulos S, Tsigkas GG, Goudevenos J. Eosinophilic responses to stent implantation and the risk of Kounis hypersensitivity associated coronary syndrome. Int J Cardiol. 2012 Apr 19;156(2):125-32 [Kounis syndrome is associated with hypersensitivity responses and coronary stent implantation]
- Kounis NG. Coronary hypersensitivity disorder: the Kounis syndrome. Clin Ther. 2013 May;35(5):563-71
- Kounis NG. Kounis syndrome: an update on epidemiology, pathogenesis, diagnosis and therapeutic management. Clin Chem Lab Med. 2016 Oct 1;54(10):1545-59
Review articles
- Braunwald E. Unstable angina: an etiologic approach to management. Circulation. 1998 Nov 24;98(21):2219-22.
- Zavras GM, Papadaki PJ, Kokkinis CE, Kalokairinov K, Kouni SN, Batsolaki M, Gouvelou-Deligianni GV, Koutsojannis C. Kounis syndrome secondary to allergic reaction following shellfish ingestion. Int J Clin Pract. 2003 Sep;57(7):622-4 [First report using of the term ‘Kounis syndrome’]
- Nemmar A, Hoet PH, Vermylen J, Nemery B, Hoylaerts MF. Pharmacological stabilization of mast cells abrogates late thrombotic events induced by diesel exhaust particles in hamsters. Circulation. 2004 Sep 21;110(12):1670-7 [Experimental study which shows that late thrombotic events can be inhibited with the use of sodium cromoglycate and dexamethasone]
- Biteker M, Duran NE, Biteker FS, Ertürk E, Aykan AC, Civan HA, Ozkan M. Kounis syndrome secondary to amoxicillin/clavulanic acid use in a child. Int J Cardiol. 2009 Jul 24;136(1):e3-5
- Biteker M, Duran NE, Biteker FS, Civan HA, Kaya H, Gökdeniz T, Yildiz M, Ozkan M. Allergic myocardial infarction in childhood: Kounis syndrome. Eur J Pediatr. 2010 Jan;169(1):27-9 [First clinical study describing the frequency of Kounis syndrome in childhood]
- Lopez PR, Peiris AN. Kounis syndrome. South Med J. 2010 Nov;103(11):1148-55 [Comprehensive review on Kounis syndrome]
- Caglar FN, Caglar IM, Coskun U, Ugurlucan M, Okcun B. Kounis syndrome: myocardial infarction secondary to an allergic insult–a rare clinical entity. Acta Cardiol. 2011 Aug;66(4):559-62
- Abdelghany M, Subedi R, Shah S, Kozman H. Kounis syndrome: a review article on epidemiology, diagnostic findings, management and complications of allergic acute coronary syndrome. Int J Cardiol. 2017;232:1–4.
- Memon et al. Allergic acute coronary syndrome (Kounis syndrome). Proc (Bayl Univ Med Cent). 2015 Jul; 28(3): 358–362
Further reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
ECG LIBRARY
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


Again, translated to catalan in my website. Thanks a lot
I had a patient with a severe anaphylactic reaction secondary to tick bite who had acute onset global ST depressions. No previous cardiac history. Never seen that before and when googling (as one does), it led me straight to this article and helped so much! You learn something new every day.