Libman-Sacks endocarditis
Libman–Sacks endocarditis (LSE) is a form of nonbacterial thrombotic endocarditis (NBTE), characterized by sterile, verrucous vegetations typically found on the mitral and aortic valves. These vegetations consist of immune complexes, fibrin, mononuclear cells, and platelet thrombi, often in the absence of infection.
LSE is classically associated with systemic lupus erythematosus (SLE) and antiphospholipid syndrome (APS), but may also occur with malignancies or other autoimmune diseases. Histologically, lesions may show active fibrinous inflammation, mixed active-healed patterns, or fully fibrotic/healed stages.
Epidemiology
Libman–Sacks vegetations are found in up to 50% of lupus patients at autopsy, though echocardiographic studies estimate prevalence around 11% among living SLE patients. The condition is more frequent in patients with longer disease duration, increased disease activity, and positive antiphospholipid antibodies. It predominantly affects women of childbearing age, particularly those of Black and Hispanic descent due to the demographics of SLE.
Clinical Diagnosis
LSE is frequently asymptomatic and may be discovered incidentally or during investigation of embolic events, valve dysfunction, or systemic symptoms. It most commonly involves the mitral valve (posterior leaflet), followed by the aortic valve. Diagnosis hinges on imaging—especially transesophageal echocardiography (TEE), with 3D-TEE offering superior detection and characterization of vegetations. Laboratory findings include SLE or APS markers (ANA, dsDNA, anticardiolipin, lupus anticoagulant).
Treatment
There is no specific treatment for the vegetations themselves; management is directed at the underlying autoimmune condition. Corticosteroids and immunosuppressive agents for SLE, and anticoagulation for APS-related thrombotic risk, are standard. In severe cases with valvular dysfunction or embolic risk, surgical valve replacement may be necessary. Differentiation from infective endocarditis is critical, particularly post-valve replacement or in febrile patients, as antimicrobial therapy may be incorrectly initiated.
History of Libman-Sacks endocarditis
1924 – Emanuel Libman (1872–1946) and Benjamin Sacks (1880–1949) published A hitherto undescribed form of valvular and mural endocarditis and describe four cases of “atypical verrucous endocarditis” in patients with features now recognized as SLE, establishing the entity now known as Libman–Sacks endocarditis.
The vegetative lesions on the heart valves were capped by blood platelet thrombus deposit showing various degrees of hyaline change… In places, the vegetations were covered with endothelium but large areas remained denuded… The endocarditic lesions in all cases were free of demonstrable bacteria
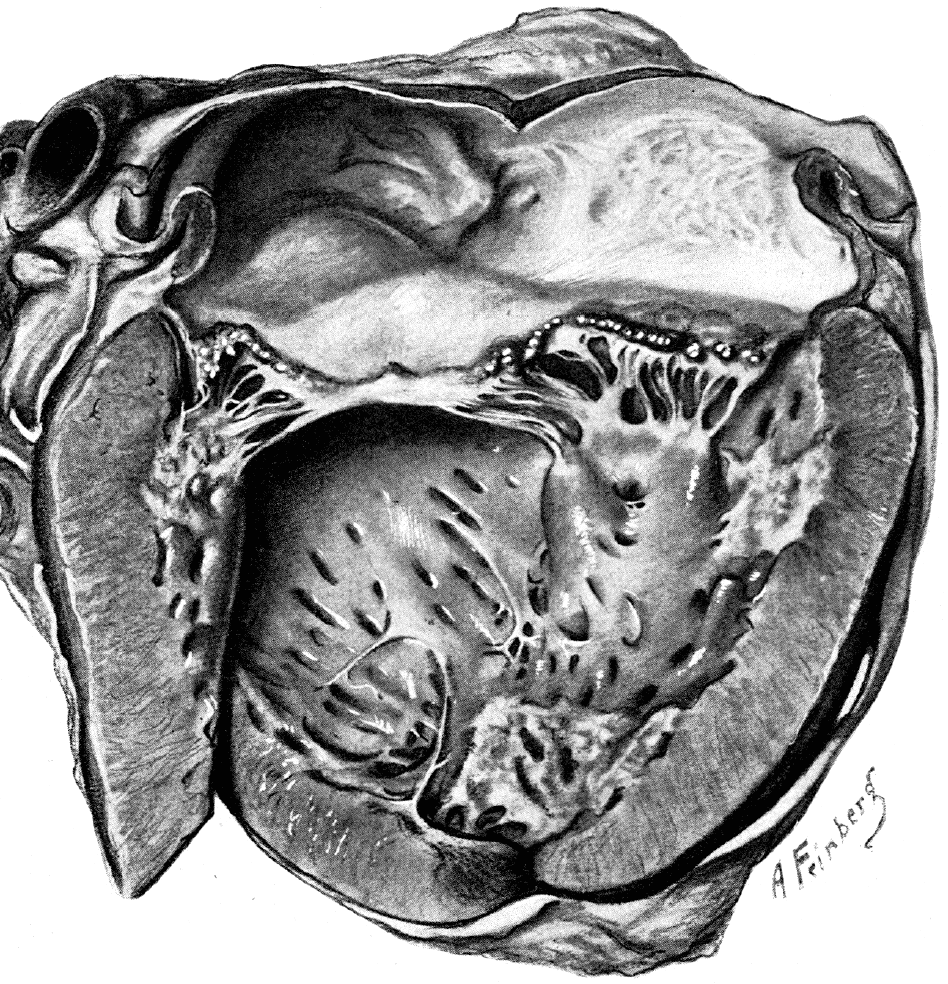
closure of mitral valve extending in places to the free edge. Areas
of endocarditis on papillary endocardium and adjacent mural endocardium; isolated patch of mural endocarditis in region of apex of ventricle. Adapted from Libman E, Sacks B. Arch Intern Med. 1924
1985 – D’Alton et al reports link LSE to antiphospholipid antibodies, suggesting a broader autoimmune thrombotic mechanism.
They reported the case report described a young woman with systemic lupus erythematosus (SLE), positive lupus anticoagulant, and verrucous endocarditis, marking the first recognized association between LSE and antiphospholipid antibodies
1989 – Asherson and Hughes provide further evidence which solidifies the association between LSE and APS. Their publication highlighted the broader spectrum of LSE manifestations and emphasized the significant role of antiphospholipid antibodies in its pathogenesis
2007 – Moyssakis et al. publish a large echocardiographic study (n=342) showing 11% prevalence of LSE in SLE patients, with significant correlation to disease severity, aPL antibodies, and thrombotic events.
2015 – Roldan et al. demonstrate the utility of 3D-TEE over 2D-TEE in detecting and characterizing LSE vegetations, particularly in patients with cerebrovascular disease.
Associated Persons
- Emanuel Libman (1872 – 1946)
- Benjamin Sacks (1896 – 1971)
Alternative names
- Atypical verrucous endocarditis
- Libman-Sacks vegetations
- Nonbacterial thrombotic endocarditis (NBTE)
References
Historic articles
- Libman E, Sacks B. A hitherto undescribed form of valvular and mural endocarditis. Arch Intern Med. 1924;33(6): 701–737
- D’Alton JG, Preston DN, Bormanis J, Green MS, Kraag GR. Multiple transient ischemic attacks, lupus anticoagulant and verrucous endocarditis. Stroke. 1985 May-Jun;16(3):512-4.
- Asherson RA, Hughes GR. The expanding spectrum of Libman Sacks endocarditis: the role of antiphospholipid antibodies. Clin Exp Rheumatol. 1989 May-Jun;7(3):225-8.
- Moyssakis I et al. Libman-Sacks endocarditis in systemic lupus erythematosus: prevalence, associations, and evolution. Am J Med. 2007 Jul;120(7):636-42.
- Roldan CA et al. Libman-Sacks Endocarditis: Detection, Characterization, and Clinical Correlates by Three-Dimensional Transesophageal Echocardiography. J Am Soc Echocardiogr. 2015; 28(7): 770-9.
Review articles
- Doherty NE, Siegel RJ. Cardiovascular manifestations of systemic lupus erythematosus. Am Heart J. 1985 Dec;110(6):1257-65.
- Hojnik M, George J, Ziporen L, Shoenfeld Y. Heart valve involvement (Libman-Sacks endocarditis) in the antiphospholipid syndrome. Circulation. 1996 Apr 15;93(8):1579-87.
- Lee JL, Naguwa SM, Cheema GS, Gershwin ME. Revisiting Libman-Sacks endocarditis: a historical review and update. Clin Rev Allergy Immunol. 2009 Jun;36(2-3):126-30.
- Geller SA. Infective endocarditis: a history of the development of its understanding. Autopsy Case Rep. 2013 Dec 31;3(4):5-12.
- Ibrahim AM, Siddique MS. Libman-Sacks Endocarditis. 2023 Sep 4. In: StatPearls
- Hennebicq S, Silberberg D, Dubois P. Libman-Sacks endocarditis. Acta Cardiol. 2024 Dec 24:1-2

eponymictionary
the names behind the name
Bret P. Nelson, MD, AEMUS-FPD, FACEP. Professor of Emergency Medicine, System Vice Chair for Education in the Department of Emergency Medicine, System Chief of the EM Ultrasound Division Mount Sinai Hospital | Sinai EM |

